J Korean Med Sci.
2016 Nov;31(11):1846-1850. 10.3346/jkms.2016.31.11.1846.
Relapsing Polychondritis with Central Nervous System Involvement: Experience of Three Different Cases in a Single Center
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Soonchunhyang University Hospital, Bucheon, Korea. chjeon@gmail.com
- KMID: 2470284
- DOI: http://doi.org/10.3346/jkms.2016.31.11.1846
Abstract
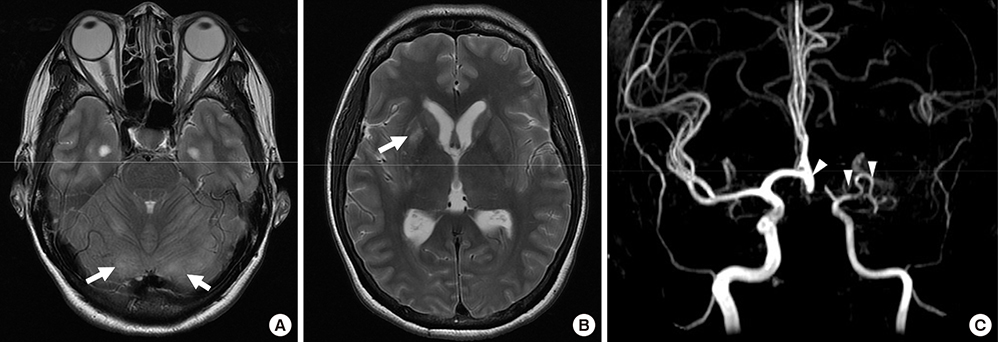
- Relapsing polychondritis (RP) is an autoimmune disorder characterized by inflammation in cartilaginous structures including the ears, noses, peripheral joints, and tracheobronchial tree. It rarely involves the central nervous system (CNS) but diagnosis of CNS complication of RP is challenging because it can present with varying clinical features. Herein we report 3 cases of relapsing polychondritis involving CNS with distinct manifestations and clinical courses. The first patient presented with rhombencephalitis resulting in brain edema and death. The second patient had acute cognitive dysfunction due to limbic encephalitis. He was treated with steroid pulse therapy and recovered without sequelae. The third patient suffered aseptic meningitis that presented as dementia, which was refractory to steroid and immune suppressive agents. We also reviewed literature on CNS complications of RP.
MeSH Terms
-
Brain/diagnostic imaging
Central Nervous System Diseases/*diagnosis/etiology
Cognitive Dysfunction/diagnosis/etiology
Dementia/diagnosis/etiology
Electroencephalography
Female
Humans
Limbic Encephalitis/complications/diagnosis/drug therapy
Magnetic Resonance Imaging
Male
Meningitis/complications/diagnosis
Middle Aged
Polychondritis, Relapsing/complications/*diagnosis
Positron Emission Tomography Computed Tomography
Steroids/therapeutic use
Figure
Reference
-
1. McAdam LP, O’Hanlan MA, Bluestone R, Pearson CM. Relapsing polychondritis: prospective study of 23 patients and a review of the literature. Medicine (Baltimore). 1976; 55:193–215.2. Puéchal X, Terrier B, Mouthon L, Costedoat-Chalumeau N, Guillevin L, Le Jeunne C. Relapsing polychondritis. Joint Bone Spine. 2014; 81:118–124.3. Sampaio L, Silva L, Mariz E, Ventura F. Central nervous system involvement in relapsing polychondritis. Joint Bone Spine. 2010; 77:619–620.4. Kashihara K, Kawada S, Takahashi Y. Autoantibodies to glutamate receptor GluRepsilon2 in a patient with limbic encephalitis associated with relapsing polychondritis. J Neurol Sci. 2009; 287:275–277.5. Mihara T, Ueda A, Hirayama M, Takeuchi T, Yoshida S, Naito K, Yamamoto H, Mutoh T. Detection of new anti-neutral glycosphingolipids antibodies and their effects on Trk neurotrophin receptors. FEBS Lett. 2006; 580:4991–4995.6. Fujiki F, Tsuboi Y, Hashimoto K, Nakajima M, Yamada T. Non-herpetic limbic encephalitis associated with relapsing polychondritis. J Neurol Neurosurg Psychiatry. 2004; 75:1646–1647.7. Yang SM, Chou CT. Relapsing polychondritis with encephalitis. J Clin Rheumatol. 2004; 10:83–85.8. Niwa A, Okamoto Y, Kondo T, Nabatame H, Takahashi R, Tomimoto H. Perivasculitic panencephalitis with relapsing polychondritis: an autopsy case report and review of previous cases. Intern Med. 2014; 53:1191–1195.9. Garcia-Egido A, Gutierrez C, De la Fuente C, Gomez F. Relapsing polychondritis-associated meningitis and encephalitis: response to infliximab. Rheumatology (Oxford). 2011; 50:1721–1723.10. Choi HJ, Lee HJ. Relapsing polychondritis with encephalitis. J Clin Rheumatol. 2011; 17:329–331.11. Yaguchi H, Tsuzaka K, Niino M, Yabe I, Sasaki H. Aseptic meningitis with relapsing polychondritis mimicking bacterial meningitis. Intern Med. 2009; 48:1841–1844.12. Hsu KC, Wu YR, Lyu RK, Tang LM. Aseptic meningitis and ischemic stroke in relapsing polychondritis. Clin Rheumatol. 2006; 25:265–267.13. Karapanayiotides T, Kouskouras K, Ioannidis P, Polychroniadou E, Grigoriadis N, Karacostas D. Internal carotid artery floating thrombus in relapsing polychondritis. J Neuroimaging. 2015; 25:142–144.14. Lawn ND, Westmoreland BF, Kiely MJ, Lennon VA, Vernino S. Clinical, magnetic resonance imaging, and electroencephalographic findings in paraneoplastic limbic encephalitis. Mayo Clin Proc. 2003; 78:1363–1368.15. Nara M, Komatsuda A, Togashi M, Wakui H. Relapsing polychondritis with encephalitis: a case report and literature review. Intern Med. 2015; 54:231–234.16. Yan M, Cooper W, Harper C, Schwartz R. Dementia in a patient with non-paraneoplastic limbic encephalitis associated with relapsing polychondritis. Pathology. 2006; 38:596–599.17. Erten-Lyons D, Oken B, Woltjer RL, Quinn J. Relapsing polychondritis: an uncommon cause of dementia. J Neurol Neurosurg Psychiatry. 2008; 79:609–610.18. Head E, Starr A, Kim RC, Parachikova A, Lopez GE, Dick M, Cribbs DH. Relapsing polychondritis with features of dementia with Lewy bodies. Acta Neuropathol. 2006; 112:217–225.19. Wang ZJ, Pu CQ, Wang ZJ, Zhang JT, Wang XQ, Yu SY, Shi Q, Liu JX, Huang XL, Fu CJ, et al. Meningoencephalitis or meningitis in relapsing polychondritis: four case reports and a literature review. J Clin Neurosci. 2011; 18:1608–1615.20. Kondo T, Fukuta M, Takemoto A, Takami Y, Sato M, Takahashi N, Suzuki T, Sato J, Atsuta N, Sobue G, et al. Limbic encephalitis associated with relapsing polychondritis responded to infliximab and maintained its condition without recurrence after discontinuation: a case report and review of the literature. Nagoya J Med Sci. 2014; 76:361–368.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Meningoencephalitis due to Relapsing Polychondritis Presenting Cognitive Impairment; Serial Neuropsychological Tests
- A Case of Relapsing Polychondritis Presenting with Diffuse Tracheobronchial Involvement
- A Case of Relapsing Polychondritis Associated with Ankylosing Spondylitis
- A Case of Relapsing Polychondritis Developed in Both Auricles
- A Case of Cutaneous Panniculitis in Relapsing Polychondritis