Clin Orthop Surg.
2020 Mar;12(1):76-85. 10.4055/cios.2020.12.1.76.
Effectiveness of Ultrasound in Evaluation of Fatty Infiltration in Rotator Cuff Muscles
- Affiliations
-
- 1Department of Orthopedic Surgery, Korea University College of Medicine, Seoul, Korea. drshoulder@gmail.com
- KMID: 2470054
- DOI: http://doi.org/10.4055/cios.2020.12.1.76
Abstract
- BACKGROUND
This study aimed to verify the diagnostic performance of Ultrasonography (US) in the evaluation of fatty infiltration (FI) in rotator cuff muscles and to analyze the diagnostic values of each measurement component.
METHODS
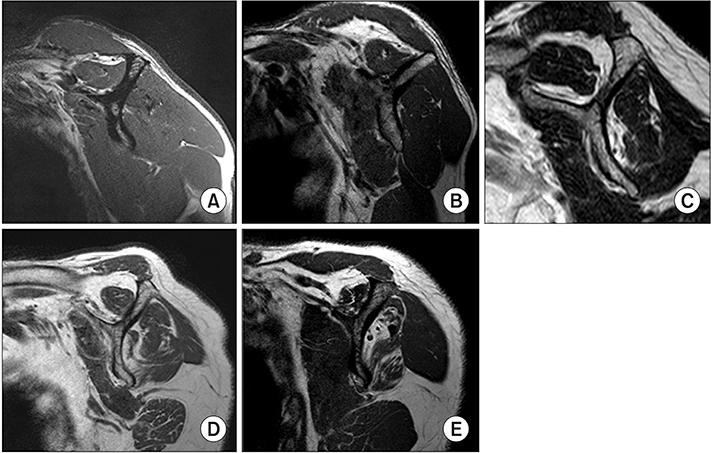
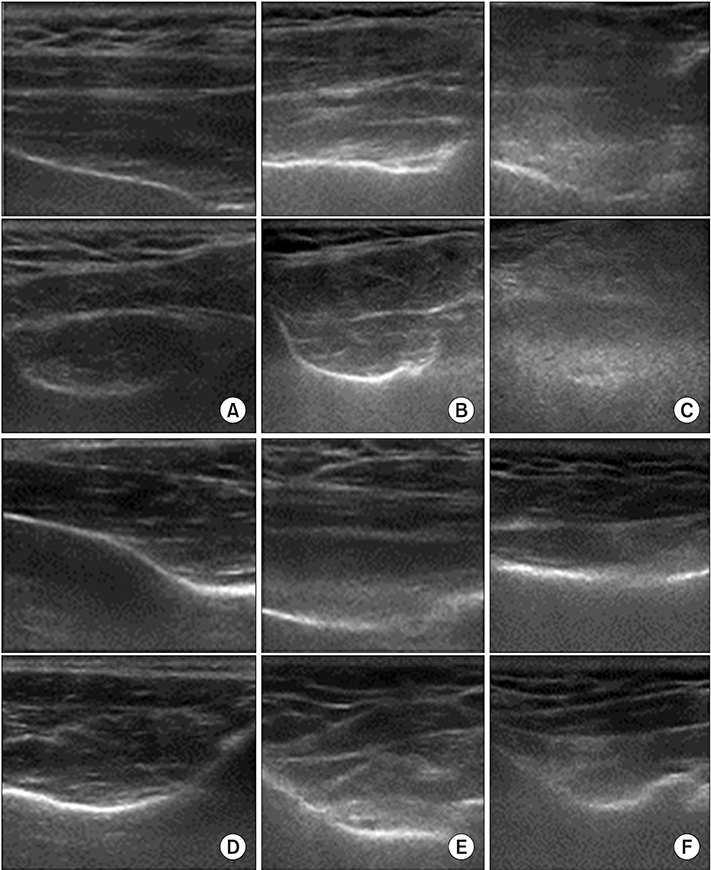
The degree of FI in 108 shoulders was assessed by magnetic resonance imaging (MRI) and US. MRI findings were graded by the Goutallier classification. US findings were graded by the Strobel method. Agreement between MRI and US findings was evaluated. The sensitivity and specificity for detecting FI and intraobserver reliabilities were also assessed.
RESULTS
US grading of the infraspinatus based on short-axis architecture showed good agreement (κ = 0.62). US grading-based on architecture showed good agreement for both supraspinatus and infraspinatus in long- and short-axis scans (supraspinatus, κ = 0.63; infraspinatus, κ = 0.68), while that based on echogenicity showed moderate agreement (supraspinatus, κ = 0.51; infraspinatus, κ = 0.50). The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of detecting advanced FI were significant in both axes.
CONCLUSIONS
US is effective for detecting advanced FI in the rotator cuff muscles. US can assess the infraspinatus more accurately than the supraspinatus, and architecture is a more decisive component of FI status than echogenicity.
Keyword
MeSH Terms
Figure
Reference
-
1. Cho NS, Rhee YG. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg. 2009; 1(2):96–104.
Article2. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994; (304):78–83.3. Shen PH, Lien SB, Shen HC, Lee CH, Wu SS, Lin LC. Long-term functional outcomes after repair of rotator cuff tears correlated with atrophy of the supraspinatus muscles on magnetic resonance images. J Shoulder Elbow Surg. 2008; 17(1 Suppl):1S–7S.
Article4. Wall LB, Teefey SA, Middleton WD, et al. Diagnostic performance and reliability of ultrasonography for fatty degeneration of the rotator cuff muscles. J Bone Joint Surg Am. 2012; 94(12):e83.
Article5. Yoo JC, Ahn JH, Yang JH, Koh KH, Choi SH, Yoon YC. Correlation of arthroscopic repairability of large to massive rotator cuff tears with preoperative magnetic resonance imaging scans. Arthroscopy. 2009; 25(6):573–582.
Article6. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999; 8(6):599–605.
Article7. Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003; 12(6):550–554.
Article8. Prickett WD, Teefey SA, Galatz LM, Calfee RP, Middleton WD, Yamaguchi K. Accuracy of ultrasound imaging of the rotator cuff in shoulders that are painful postoperatively. J Bone Joint Surg Am. 2003; 85(6):1084–1089.
Article9. Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff: a comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am. 2000; 82(4):498–504.10. Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears: comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004; 86(4):708–716.11. Forsberg AM, Nilsson E, Werneman J, Bergstrom J, Hultman E. Muscle composition in relation to age and sex. Clin Sci (Lond). 1991; 81(2):249–256.
Article12. Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. AJR Am J Roentgenol. 2008; 190(4):1105–1111.
Article13. Strobel K, Hodler J, Meyer DC, Pfirrmann CW, Pirkl C, Zanetti M. Fatty atrophy of supraspinatus and infraspinatus muscles: accuracy of US. Radiology. 2005; 237(2):584–589.
Article14. Tsubahara A, Chino N, Akaboshi K, Okajima Y, Takahashi H. Age-related changes of water and fat content in muscles estimated by magnetic resonance (MR) imaging. Disabil Rehabil. 1995; 17(6):298–304.
Article15. Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998; 33(3):163–170.
Article16. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33(1):159–174.
Article17. Rice CL, Cunningham DA, Paterson DH, Lefcoe MS. Arm and leg composition determined by computed tomography in young and elderly men. Clin Physiol. 1989; 9(3):207–220.
Article18. Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007; 35(5):719–728.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship of the Sagittal Extent of Rotator Cuff Tears to the Grade of Fatty Degeneration of the Rotator Cuff Muscles
- Ultrasound Images after Rotator Cuff Surgery: Usefulness of Postoperative Follow-Up
- Analysis of the Change in Fatty Degeneration of the Rotator Cuff and Its Influence on the Outcome of Rotator Cuff Repair
- Relationship of Posterior Decentering of the Humeral Head with Tear Size and Fatty Degeneration in Rotator Cuff Tear
- Preoperative Korean Shoulder Scoring System Correlates with Preoperative Factors of Rotator Cuff Tears