J Korean Orthop Assoc.
2019 Dec;54(6):519-527. 10.4055/jkoa.2019.54.6.519.
Study of Deformity by the Involvement of the Femoral Head of the Proximal Femur in Polyostotic Fibrous Dysplasia
- Affiliations
-
- 1Department of Orthopedic Surgery, Chonnam National University Medical School, Gwangju, Korea. stjung@chonnam.ac.kr
- KMID: 2469883
- DOI: http://doi.org/10.4055/jkoa.2019.54.6.519
Abstract
- PURPOSE
To evaluate the treatment result in polyostotic fibrous dysplasia classified according to the involvement of the femoral head.
MATERIALS AND METHODS
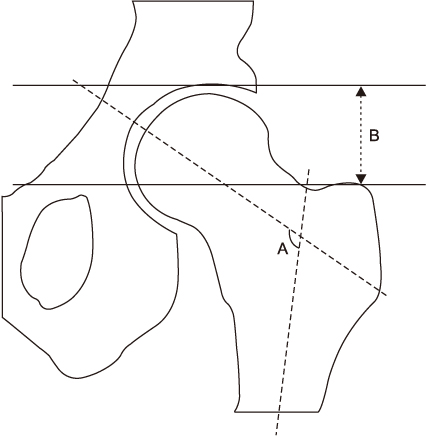
Twenty-three patients from March 1987 to March 2014 were reviewed retrospectively. Patients with no involvement of the physeal scar in the femoral head were classified as Type I, and those with involvement of the physeal scar were classified as Type II. A plain radiograph was used to measure the femoral neck shaft angle, articulo-trochanteric distance (ATD), and anterior bowing through the lateral view. A teleoroentgenogram of the lower limb was used to measure the leg length discrepancy and lower extremity mechanical axis. The pre- and postoperative femoral neck-shaft angle and ATD were compared to assess the degree of correction of the deformity.
RESULTS
Among a total of 46 cases (23 patients), 28 cases (23 patients) had lesions in the proximal femur. Type I were 16/28 cases (15/23 patients) and Type II were 12/28 cases (9/23 patients). The preoperative proximal femoral neck-shaft angle was 116.8° in Type I and 95.3° in Type II. The ATD was 12.08 mm in Type I and −5.54 mm in Type II. The deformity correction showed significant improvement immediately after surgery, the deformity correction was lost in Type II (neck shaft angle Type I: 133.8°-130.8°, Type II: 128.6°-116.9°, and ATD Type I: 17.66-15.72 mm, Type II: 7.44-4.16 mm). The extent of anterior bowing was 12.74° in Type I and 20.19° in Type II. The mean differences of 12 mm between the 9 patients who showed a leg length discrepancy and the lower extremity mechanical axis showed 4 cases of lateral deviation and 7 cases of medial deviation.
CONCLUSION
In polyostotic fibrous dysplasia, when the femur head is involved, the femur neck shaft angle, ATD, and anterior bowing of the femur had more deformity, and the postoperative correction of deformity was lost, suggesting that the involvement of the femoral head was an important factor in the prognosis of the disease.
MeSH Terms
Figure
Reference
-
1. Lichtenstein L. Polyostotic fibrous dysplasia. Arch Surg. 1938; 36:874–898.
Article2. Harris WH, Dudley HR Jr, Barry RJ. The natural history of fibrous dysplasia. An orthopaedic, pathological, and roentgenographic study. J Bone Joint Surg Am. 1962; 44-A:207–233.3. Zhang X, Chen C, Duan H, Tu C. Radiographic classification and treatment of fibrous dysplasia of the proximal femur: 227 femurs with a mean follow-up of 6 years. J Orthop Surg Res. 2015; 10:171.
Article4. Ippolito E, Farsetti P, Boyce AM, Corsi A, De Maio F, Collins MT. Radiographic classification of coronal plane femoral deformities in polyostotic fibrous dysplasia. Clin Orthop Relat Res. 2014; 472:1558–1567.
Article5. Stephenson RB, London MD, Hankin FM, Kaufer H. Fibrous dysplasia. An analysis of options for treatment. J Bone Joint Surg Am. 1987; 69:400–409.6. Reed RJ. Fibrous dysplasia of bone. A review of 25 cases. Arch Pathol. 1963; 75:480–495.7. Funk FJ Jr, Wells RE. Hip problems in fibrous dysplasia. Clin Orthop Relat Res. 1973; (90):77–82.
Article8. Lee HK, Kim HJ, Huh MG, Yeo BG. Treatment of fibrous dysplasia. J Korean Orthop Assoc. 1990; 25:1487–1495.
Article9. Weinstein LS, Shenker A, Gejman PV, Merino MJ, Friedman E, Spiegel AM. Activating mutations of the stimulatory G protein in the McCune-Albright syndrome. N Engl J Med. 1991; 325:1688–1695.
Article10. Enneking WF, Gearen PF. Fibrous dysplasia of the femoral neck. Treatment by cortical bone-grafting. J Bone Joint Surg Am. 1986; 68:1415–1422.
Article11. Freeman BH, Bray EW 3rd, Meyer LC. Multiple osteotomies with Zickel nail fixation for polyostotic fibrous dysplasia involving the proximal part of the femur. J Bone Joint Surg Am. 1987; 69:691–698.
Article12. Guille JT, Kumar SJ, MacEwen GD. Fibrous dysplasia of the proximal part of the femur. Long-term results of curettage and bone-grafting and mechanical realignment. J Bone Joint Surg Am. 1998; 80:648–658.
Article13. Ippolito E, Bray EW, Corsi A, et al. Natural history and treatment of fibrous dysplasia of bone: a multicenter clinicopathologic study promoted by the European Pediatric Orthopaedic Society. J Pediatr Orthop B. 2003; 12:155–177.
Article14. Keijser LC, Van Tienen TG, Schreuder HW, Lemmens JA, Pruszczynski M, Veth RP. Fibrous dysplasia of bone: management and outcome of 20 cases. J Surg Oncol. 2001; 76:157–166. discussion 167-8.
Article15. Leet AI, Collins MT. Current approach to fibrous dysplasia of bone and McCune-Albright syndrome. J Child Orthop. 2007; 1:3–17.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Osteosarcoma Arising in a Polyostotic Fibrous Dysplasia: A Case Report
- Monostotic Fibrous Dysplasia of Inferior Turbinate
- The Results after Surgically Managing Patients with Fibrous Dysplasia of the Proximal Femur
- A Case of Extensive polyostotic fibrous dysplasia
- A case report of polyostotic fibrous dysplasia