Korean J Ophthalmol.
2020 Feb;34(1):27-34. 10.3341/kjo.2019.0099.
Clinical Manifestations and Visual Prognosis of Cilioretinal Artery Sparing Central Retinal Artery Occlusion
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. sejoon1@snu.ac.kr
- 2Department of Ophthalmology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2469284
- DOI: http://doi.org/10.3341/kjo.2019.0099
Abstract
- PURPOSE
To investigate the clinical manifestations and prognosis of eyes with cilioretinal artery sparing central retinal artery occlusion (CRAO).
METHODS
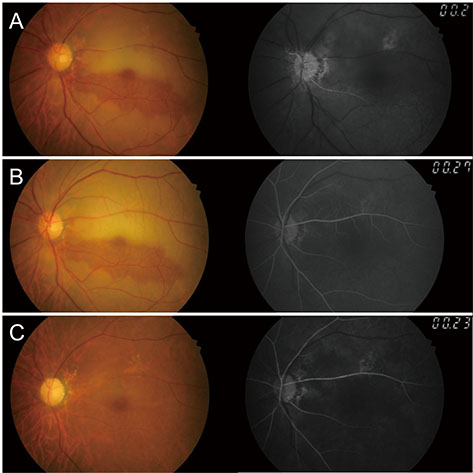
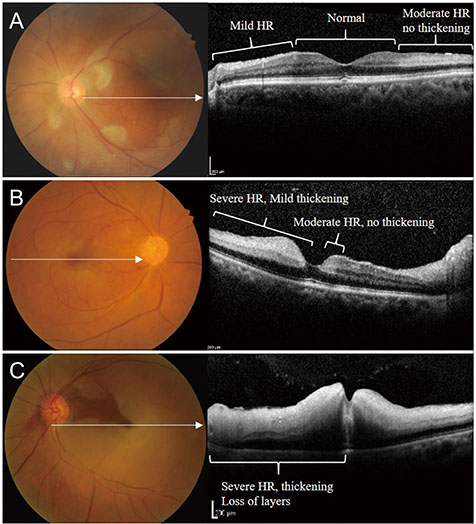
A retrospective study was conducted on 90 eyes diagnosed with complete CRAO, including 16 cases of cilioretinal artery sparing CRAO. Clinical features, visual outcome, papillomacular bundle involvement, and remnant visual field were analyzed according to cilioretinal artery sparing.
RESULTS
Among eyes with complete CRAO, the proportion of cilioretinal artery sparing CRAO was 17.8% (16 / 90). Mean initial best-corrected visual acuities (BCVAs) (2.04 ± 0.69 vs. 2.34 ± 0.47, p = 0.039) and final BCVAs (1.65 ± 0.87 vs. 2.22 ± 0.84, p = 0.001) were significantly better in eyes of the cilioretinal artery sparing group than the non-sparing group. The proportion with poor visual outcome (final BCVA <20 / 200) was 81.3% in the cilioretinal artery sparing group and 97.3% in the non-sparing group (p = 0.01). In sub-group analysis within cilioretinal artery sparing CRAO eyes, ischemic involvement of the papillomacular bundle at disease onset was significantly more frequent in the poor vision group (BCVA <20 / 200, 12 / 13 [92.3%]) than in the good vision group (BCVA ≥20 / 200, 1 / 3 [33.3%], p = 0.016) and it was associated with preserved central visual field.
CONCLUSIONS
Although cilioretinal artery sparing is common in CRAO and has a better prognosis than complete CRAO, the visual outcome is generally poor and only a small proportion of eyes has preserved small central visual field. Ischemic injury of the papillomacular bundle at the acute stage of CRAO correlates with poor visual outcome and could be a prognostic sign.
MeSH Terms
Figure
Reference
-
1. Varma DD, Cugati S, Lee AW, Chen CS. A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond). 2013; 27:688–697.
Article2. Cugati S, Varma DD, Chen CS, Lee AW. Treatment options for central retinal artery occlusion. Curr Treat Options Neurol. 2013; 15:63–77.
Article3. Hayreh SS. Acute retinal arterial occlusive disorders. Prog Retin Eye Res. 2011; 30:359–394.
Article4. Brown GC, Shields JA. Cilioretinal arteries and retinal arterial occlusion. Arch Ophthalmol. 1979; 97:84–92.
Article5. Liu L, Liu LM, Chen L. Incidence of cilioretinal arteries in Chinese Han population. Int J Ophthalmol. 2011; 4:323–325.6. Doguizi S, Sekeroglu MA, Anayol MA, Yilmazbas P. Central retinal artery occlusion with double cilioretinal artery sparing. Retin Cases Brief Rep. 2019; 13:75–78.
Article7. Bansal N, Bansal RK. A middle hyper-reflective band on spectral domain optical coherence tomography in a case of acute nonarteritic central retinal artery occlusion with sparing of cilioretinal artery. Indian J Ophthalmol. 2019; 67:1345.
Article8. Cho KH, Ahn SJ, Jung C, et al. Ischemic injury of the papillomacular bundle is a predictive marker of poor vision in eyes with branch retinal artery occlusion. Am J Ophthalmol. 2016; 162:107–120.
Article9. Chen CS, Lee AW. Management of acute central retinal artery occlusion. Nat Clin Pract Neurol. 2008; 4:376–383.
Article10. Hayreh SS, Zimmerman MB. Central retinal artery occlusion: visual outcome. Am J Ophthalmol. 2005; 140:376–391.
Article11. Justice J Jr, Lehmann RP. Cilioretinal arteries. A study based on review of stereo fundus photographs and fluorescein angiographic findings. Arch Ophthalmol. 1976; 94:1355–1358.12. Ahn SJ, Woo SJ, Park KH, et al. Retinal and choroidal changes and visual outcome in central retinal artery occlusion: an optical coherence tomography study. Am J Ophthalmol. 2015; 159:667–676.
Article13. Kim HM, Park YJ, Park KH, Woo SJ. Visual field defects and changes in central retinal artery occlusion. PLoS One. 2019; 14:e0209118.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cilioretinal Artery Occlusion Associated with Central Retinal Vein Occlusion
- Central retinal vein occlusion combined with cilioretinal artery occlusion
- A Clinical Study of 36 Cases of Retinal Artery Occlusion
- Visual Improvement following Acute Obstruction of the Retinal and Choroidal Blood Flows
- Incomplete Central Retinal Artery Occlusion