J Korean Soc Radiol.
2020 Jan;81(1):70-80. 10.3348/jksr.2020.81.1.70.
MR Lymphangiography
- Affiliations
-
- 1Department of Radiology, Asan Medical Center, University of Ulsan, College of Medicine, Seoul, Korea. shlee@amc.seoul.kr
- 2Department of Plastic Surgery, Asan Medical Center, University of Ulsan, College of Medicine, Seoul, Korea.
- KMID: 2469183
- DOI: http://doi.org/10.3348/jksr.2020.81.1.70
Abstract
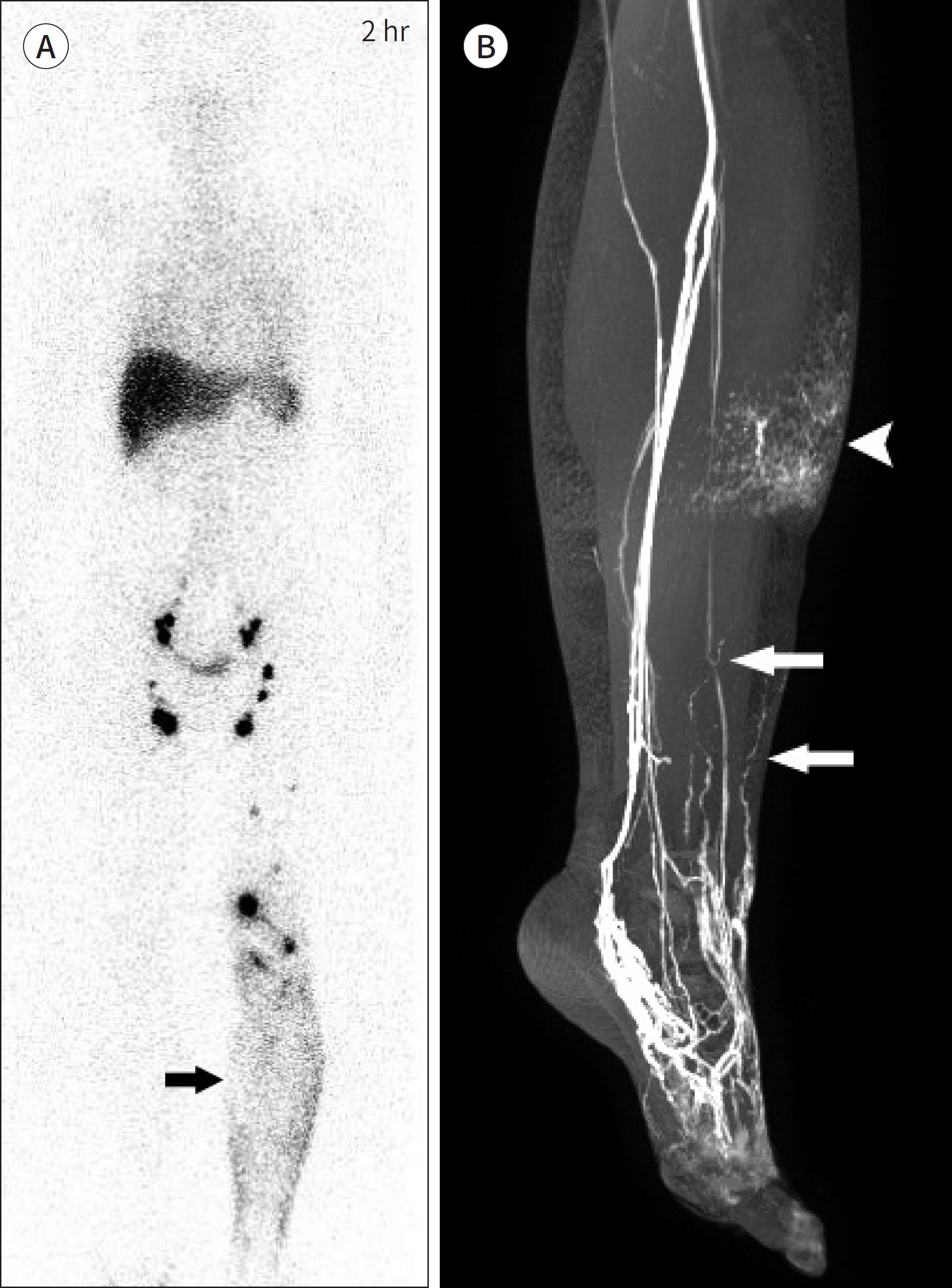
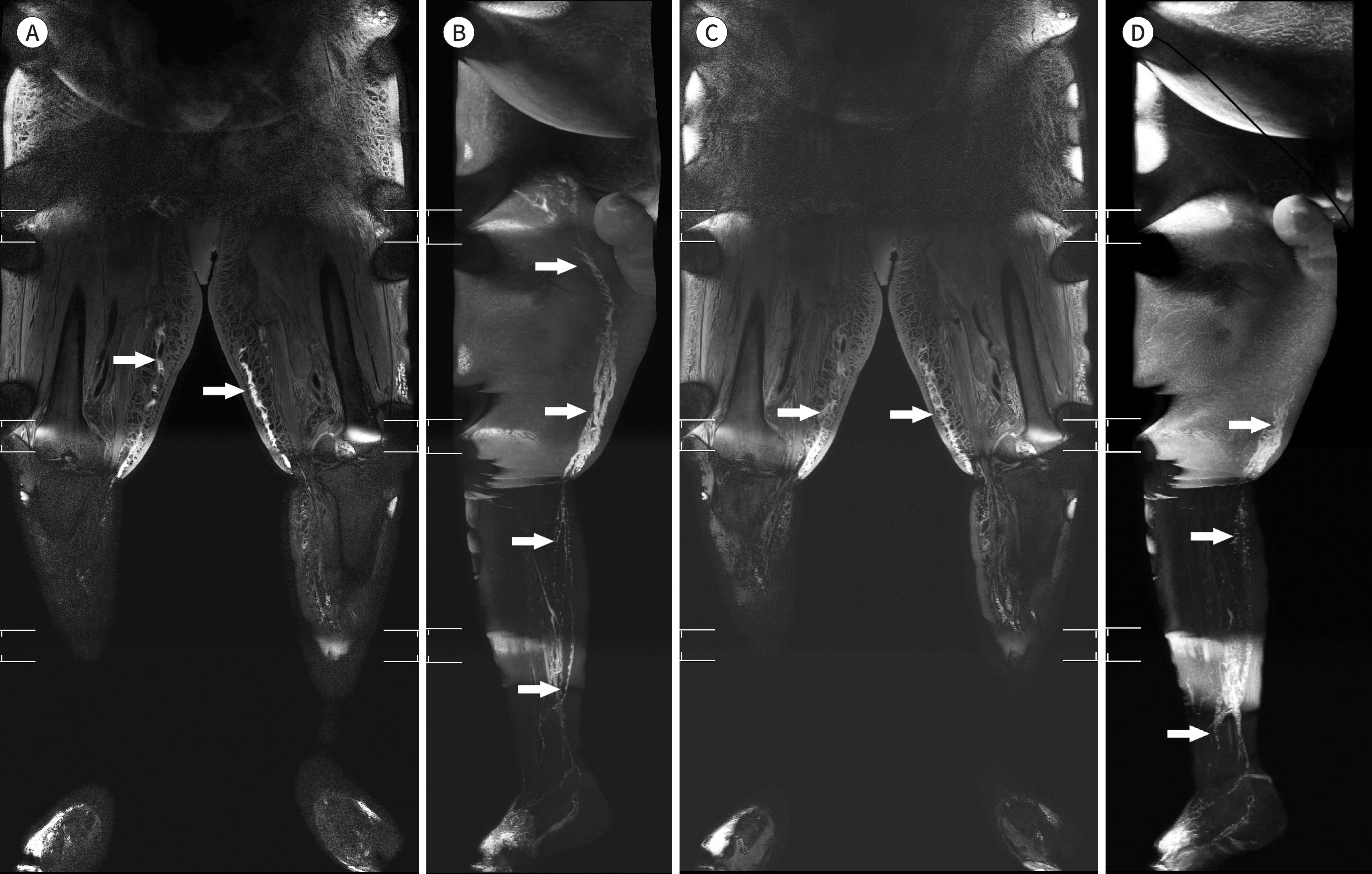
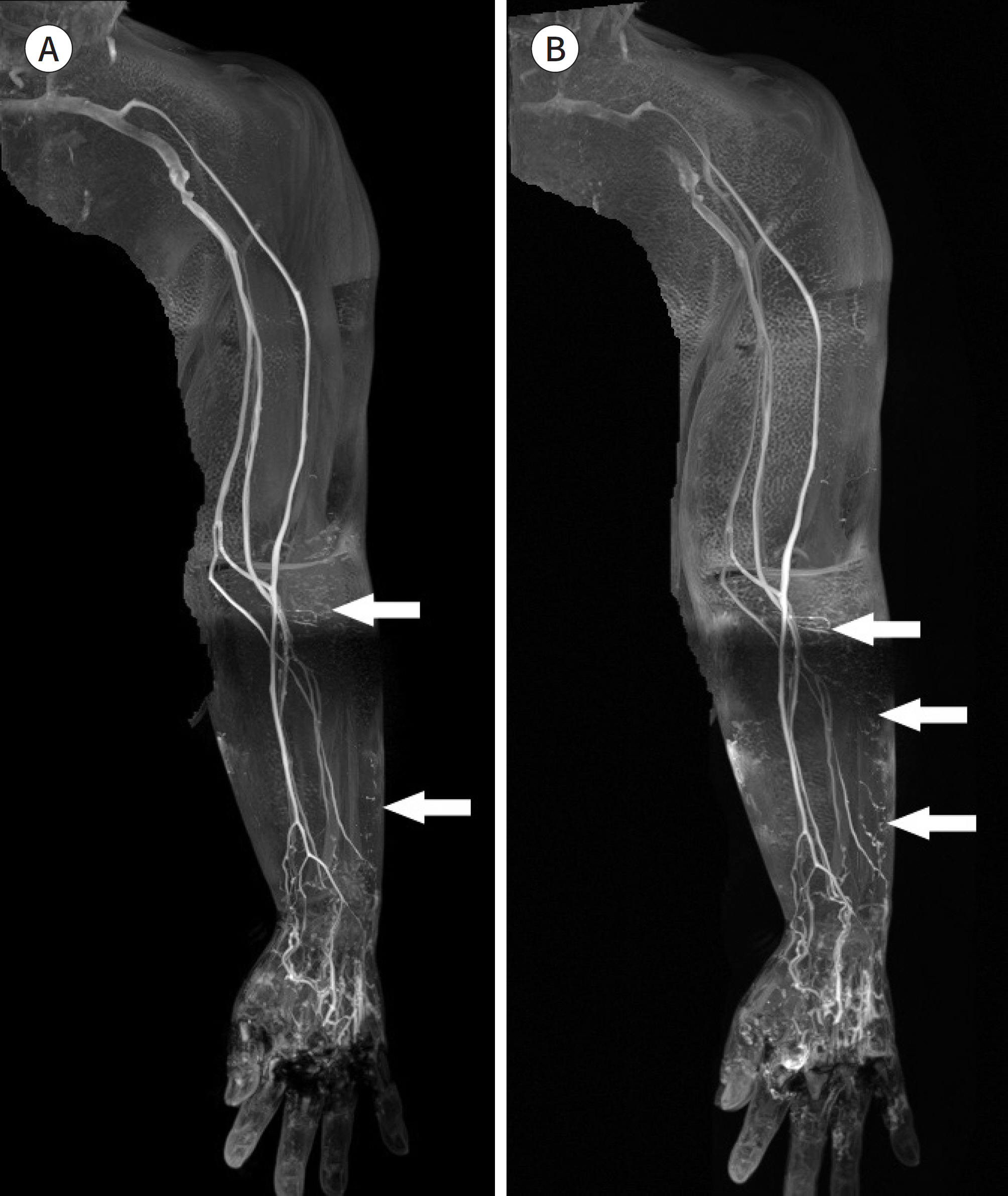
- Currently, there has been an increase in the use of surgical modalities to treat lymphedema and MR imaging to examine lymphatic vessels. Furthermore, there have been several advancements in the field of MR imaging, from the traditional heavily T2-weighted images to three-dimensional images. Three-dimensional images include spoiled gradient echo images, and numerous advanced techniques have been implemented. Among the fat suppression techniques, mDixon technique has recently been in the spotlight.
MeSH Terms
Figure
Reference
-
1. Executive Committee. The diagnosis and treatment of peripheral lymphedema: 2016 consensus document of the International Society of Lymphology.Lymphology. 2016; 49:170–184.2. Ki EY, Park JS, Lee KH, Hur SY. Incidence and risk factors of lower extremity lymphedema after gynecologic surgery in ovarian cancer. Int J Gynecol Cancer. 2016; 26:1327–1332.
Article3. Hayes SC, Janda M, Ward LC, Reul-Hirche H, Steele ML, Carter J, et al. Lymphedema following gynecological cancer: results from a prospective, longitudinal cohort study on prevalence, incidence and risk factors.Gynecol Oncol. 2017; 146:623–629.4. Shah C, Vicini FA. Breast cancer-related arm lymphedema: incidence rates, diagnostic techniques, optimal management and risk reduction strategies. Int J Radiat Oncol Biol Phys. 2011; 81:907–914.
Article5. Mihara M, Hara H, Hayashi Y, Narushima M, Yamamoto T, Todokoro T, et al. Pathological steps of cancer-re-lated lymphedema: histological changes in the collecting lymphatic vessels after lymphadenectomy.PLoS One. 2012; 7:e41126.6. Ciudad P, Sabbagh MD, Agko M, Huang TCT, Manrique OJ, Román C, et al. Surgical management of lower extremity lymphedema: a comprehensive review.Indian J Plast Surg. 2019; 52:81–92.7. Karpanen T, Alitalo K. Molecular biology and pathology of lymphangiogenesis.Annu Rev Pathol. 2008; 3:367–397.8. Kim H, Kataru RP, Koh GY. Regulation and implications of inflammatory lymphangiogenesis.Trends Immu-nol. 2012; 33:350–356.9. Koshima I, Inagawa K, Urushibara K, Moriguchi T. Supermicrosurgical lymphaticovenular anastomosis for the treatment of lymphedema in the upper extremities.J Reconstr Microsurg. 2000; 16:437–442.10. Neligan PC, Kung TA, Maki JH. MR lymphangiography in the treatment of lymphedema.J Surg Oncol. 2017; 115:18–22.11. Garza RM, Chang DW. Lymphovenous bypass for the treatment of lymphedema.J Surg Oncol. 2018; 118:743–749.12. Barrett T, Choyke PL, Kobayashi H. Imaging of the lymphatic system: new horizons.Contrast Media Mol Imaging. 2006; 1:230–245.13. Zaleska MT, Olszewski WL. Imaging lymphatics in human normal and lymphedema limbs-usefulness of var-ious modalities for evaluation of lymph and edema fluid flow pathways and dynamics.J Biophotonics. 2018; 11:e201700132.14. Keo HH, Gretener SB, Staub D. Clinical and diagnostic aspects of lymphedema. Vasa. 2017; 46:255–261.
Article15. Mihara M, Hara H, Araki J, Kikuchi K, Narushima M, Yamamoto T, et al. Indocyanine green (ICG) lymphography is superior to lymphoscintigraphy for diagnostic imaging of early lymphedema of the upper limbs. PLoS One. 2012; 7:e38182.
Article16. Notohamiprodjo M, Weiss M, Baumeister RG, Sommer WH, Helck A, Crispin A, et al. MR lymphangiography at 3.0 T: correlation with lymphoscintigraphy. Radiology. 2012; 264:78–87.
Article17. Landau MJ, Gould DJ, Patel KM. Advances in fluorescent-image guided surgery.Ann Transl Med. 2016; 4:392.18. Akita S, Mitsukawa N, Kazama T, Kuriyama M, Kubota Y, Omori N, et al. Comparison of lymphoscintigraphy and indocyanine green lymphography for the diagnosis of extremity lymphoedema. J Plast Reconstr Aes-thet Surg. 2013; 66:792–798.
Article19. Liu NF, Yan ZX, Wu XF. Classification of lymphatic-system malformations in primary lymphoedema based on MR lymphangiography. Eur J Vasc Endovasc Surg. 2012; 44:345–349.
Article20. Lee BB, Antignani PL, Baroncelli TA, Boccardo FM, Brorson H, Campisi C, et al. IUA-ISVI consensus for diagnosis guideline of chronic lymphedema of the limbs. Int Angiol. 2015; 34:311–332.21. Seki Y, Kajikawa A, Yamamoto T, Takeuchi T, Terashima T, Kurogi N. Real-time Indocyanine green videolym-phography navigation for lymphaticovenular anastomosis.Plast Reconstr Surg Glob Open. 2019; 7:e2253.22. Ogata F, Narushima M, Mihara M, Azuma R, Morimoto Y, Koshima I. Intraoperative lymphography using indocyanine green dye for near-infrared fluorescence labeling in lymphedema.Ann Plast Surg. 2007; 59:180–184.23. Mitsumori LM, McDonald ES, Neligan PC, Maki JH. Peripheral magnetic resonance lymphangiography: techniques and applications. Tech Vasc Interv Radiol. 2016; 19:262–272.
Article24. Lohrmann C, Foeldi E, Speck O, Langer M. High-resolution MR lymphangiography in patients with primary and secondary lymphedema.AJR Am J Roentgenol. 2006; 187:556–561.25. Fink C, Bock M, Kiessling F, Delorme S. Interstitial magnetic resonance lymphography with gadobutrol in rats: evaluation of contrast kinetics. Invest Radiol. 2002; 37:655–662.26. Dimakakos E, Koureas A, Skiadas V, Kostapanagiotou G, Katsenis K, Arkadopoulos N, et al. Interstitial magnetic resonance lymphography with gadobutrol in rabbits and an initial experience in humans.Lymphology. 2006; 39:164–170.27. Jeon JY, Lee SH, Shin MJ, Chung HW, Lee MH. Three-dimensional isotropic fast spin-echo MR lymphangiography of T1-weighted and intermediate-weighted pulse sequences in patients with lymphoedema. Clin Radiol. 2016; 71:e56–e63.
Article28. Bae JS, Yoo RE, Choi SH, Park SO, Chang H, Suh M, et al. Evaluation of lymphedema in upper extremities by MR lymphangiography: comparison with lymphoscintigraphy.Magn Reson Imaging. 2018; 49:63–70.29. Alazraki NP, Styblo T, Grant SF, Cohen C, Larsen T, Waldrop S, et al. Sentinel node staging of early breast cancer using lymphoscintigraphy and the intraoperative gamma detecting probe.Radiol Clin North Am. 2001; 39:947–956. viii.30. Kobayashi H, Brechbiel MW. Dendrimer-based macromolecular MRI contrast agents: characteristics and ap-plication. Mol Imaging. 2003; 2:1–10.
Article31. Nakajima T, Turkbey B, Sano K, Sato K, Bernardo M, Hoyt RF, et al. MR lymphangiography with intradermal gadofosveset and human serum albumin in mice and primates.J Magn Reson Imaging. 2014; 40:691–697.32. Kobayashi H, Kawamoto S, Bernardo M, Brechbiel MW, Knopp MV, Choyke PL. Delivery of gadolinium-la-beled nanoparticles to the sentinel lymph node: comparison of the sentinel node visualization and estima-tions of intra-nodal gadolinium concentration by the magnetic resonance imaging. J Control Release. 2006; 111:343–351.
Article33. Ripley B, Wilson GJ, Lalwani N, Briller N, Neligan PC, Maki JH. Initial clinical experience with dual-agent re-laxation contrast for isolated lymphatic channel mapping. Radiology. 2018; 286:705–714.
Article34. Finn JP, Nguyen KL, Hu P. Ferumoxytol vs. gadolinium agents for contrast-enhanced MRI: thoughts on evolv-ing indications, risks, and benefits.J Magn Reson Imaging. 2017; 46:919–923.35. Liu NF, Lu Q, Jiang ZH, Wang CG, Zhou JG. Anatomic and functional evaluation of the lymphatics and lymph nodes in diagnosis of lymphatic circulation disorders with contrast magnetic resonance lymphangiography. J Vasc Surg. 2009; 49:980–987.
Article36. Mitsumori LM, McDonald ES, Wilson GJ, Neligan PC, Minoshima S, Maki JH. MR lymphangiography: how i do it.J Magn Reson Imaging. 2015; 42:1465–1477.37. Weiss M, Burgard C, Baumeister R, Strobl F, Rominger A, Bartenstein P, et al. Magnetic resonance imaging versus lymphoscintigraphy for the assessment of focal lymphatic transport disorders of the lower limb: first experiences. Nuklearmedizin. 2014; 53:190–196.38. Cellina M, Oliva G, Menozzi A, Soresina M, Martinenghi C, Gibelli D. Non-contrast magnetic resonance lymphangiography: an emerging technique for the study of lymphedema.Clin Imaging. 2019; 53:126–133.39. Kim EY, Hwang HS, Lee HY, Cho JH, Kim HK, Lee KS, et al. Anatomic and functional evaluation of central lymphatics with noninvasive magnetic resonance lymphangiography. Medicine (Baltimore). 2016; 95:e3109.
Article40. Wright KL, Harrell MW, Jesberger JA, Landeras L, Nakamoto DA, Thomas S, et al. Clinical evaluation of CAIPIRINHA: comparison against a GRAPPA standard. J Magn Reson Imaging. 2014; 39:189–194.
Article41. Boettcher J, Pfeil A, Wolf G, Hansch A. Magnetic resonance venography of the upper venous system with blood pool contrast agent: comparison of two different T1-weighted sequences.Clin Imaging. 2013; 37:245–250.42. Eggers H, Brendel B, Duijndam A, Herigault G. Dual-echo Dixon imaging with flexible choice of echo times. Magn Reson Med. 2011; 65:96–107.
Article43. Pieper CC, Schild HH. Interstitial transpedal MR-lymphangiography of central lymphatics using a standard MR contrast agent: feasibility and initial results in patients with chylous effusions.Rofo. 2018; 190:938–945.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postoperative Chylothorax: the Use of Dynamic Magnetic Resonance Lymphangiography and Thoracic Duct Embolization
- 2 Cases of Lymphangiography for the Diagnosis of Retroperitoneal Metastasis
- Lymphangiography to Treat Postoperative Lymphatic Leakage: A Technical Review
- A Case of Congenital Lymphatic Dysplasia Complicated by Hydrops Fetalis
- The role of lymphatic interventional radiology for postoperative lymphorrhea