Perinatology.
2018 Jun;29(2):97-100. 10.14734/PN.2018.29.2.97.
Spinal Cord Infarction Following Total Hysterectomy Due to Severe Postpartum Hemorrhage
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Dankook University College of Medicine, Cheonan, Korea. soo8541@hanmail.net
- KMID: 2468556
- DOI: http://doi.org/10.14734/PN.2018.29.2.97
Abstract
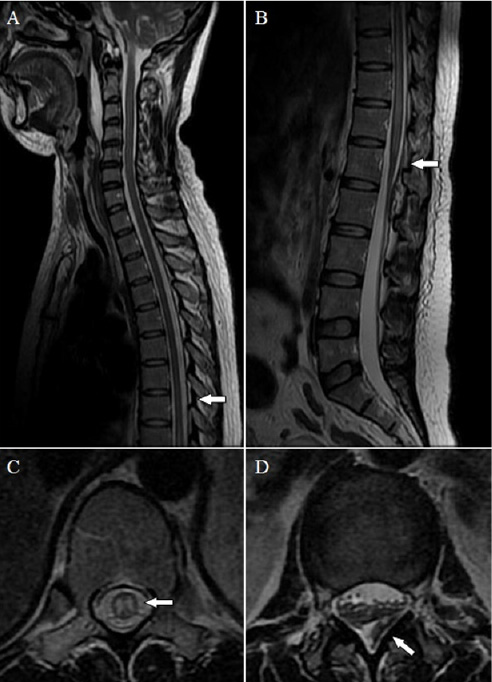
- Spinal cord infarction (SCI) is a rare but often disastrous disorder caused by various pathologic status. The research reports a 34-year-old woman developed SCI after spinal anesthesia for relieving labor pain and total hysterectomy, due to postpartum hemorrhage. Three times of spinal anesthesia were performed, two for controlling labor pain, which were succeeded and one for cesarean delivery, which was failed. After delivery, she was referred to Dankook University Hospital because of uterine atony. On arrival in the emergency room, the blood pressure decreased to 58/32 mmHg, she had a pulse rate of 144 beats/min. While emergent total hysterectomy was performed, she remained hemodynamically stable and there was no episode of hypotension. Since she complained of immobility and loss of sensations the day after the operation, magnetic resonance imaging was performed and showed ischemic change at central portion of the spinal cord at T8 to L1 level.
Keyword
MeSH Terms
Figure
Reference
-
1. Sandson TA, Friedman JH. Spinal cord infarction. Report of 8 cases and review of the literature. Medicine (Baltimore). 1989; 68:282–292.2. Weidauer S, Nichtweiß M, Hattingen E, Berkefeld J. Spinal cord ischemia: aetiology, clinical syndromes and imaging features. Neuroradiology. 2015; 57:241–257.
Article3. Vongveeranonchai N, Zawahreh M, Strbian D, Sundararajan S. Evaluation of a patient with spinal cord infarction after a hypotensive episode. Stroke. 2014; 45:e203–e205.
Article4. Satran R. Spinal cord infarction. Stroke. 1988; 19:529–532.
Article5. Colman MW, Hornicek FJ, Schwab JH. Spinal cord blood supply and its surgical implications. J Am Acad Orthop Surg. 2015; 23:581–591.
Article6. Novy J, Carruzzo A, Maeder P, Bogousslavsky J. Spinal cord ischemia: clinical and imaging patterns, pathogenesis, and outcomes in 27 patients. Arch Neurol. 2006; 63:1113–1120.7. Vargas MI, Gariani J, Sztajzel R, Barnaure-Nachbar I, Delattre BM, Lovblad KO, et al. Spinal cord ischemia: Practical imaging tips, pearls, and pitfalls. AJNR Am J Neuroradiol. 2015; 36:825–830.
Article8. Rao Shailaja V, Anjali P, Borkar MS, Gajanan S, Vimlesh P. A rare complication of pre-eclampsia and severe postpartum hemorrhage-spinal cord leading to anterior spinal artery syndrome. IOSR-JDMS. 2015; 14:38–40.9. Scott DB, Hibbard BM. Serious non-fatal complications associated with extradural block in obstetric practice. Br J Anaesth. 1990; 64:537–541.
Article10. Soda T, Shimizu I, Takagaki M, Yamada K, Dehara M, Teramoto Y, et al. A case of benign postpartum anterior spinal artery syndrome with thrombocytosis and high fibrolytic activity. Brain Nerve. 2011; 63:1125–1129.11. Nardone R, Pikija S, Mutzenbach JS, Seidl M, Leis S, Trinka E, et al. Current and emerging treatment options for spinal cord ischemia. Drug Discov Today. 2016; 21:1632–1641.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of Bilateral Uterine Artery Ligation in Postpartum Hemorrhage
- Cervical Spinal Cord Infarction Presenting as Chest Pain in Patients with Acute Cerebellar Infarction
- Paraplegia due to Spinal Cord Infarction After Lifting Heavy Objects
- Acute Sheehan's Syndrome Associated with Postpartum Hemorrhage
- Posterior Thoracic Spinal Cord Artery Infarction