J Korean Med Sci.
2016 Sep;31(9):1485-1490. 10.3346/jkms.2016.31.9.1485.
Comparison of an Intraoperative Infusion of Dexmedetomidine, Fentanyl, and Remifentanil on Perioperative Hemodynamics, Sedation Quality, and Postoperative Pain Control
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, St. Vincent's Hospital, The Catholic University of Korea, Seoul, Korea. flood1@naver.com
- KMID: 2468284
- DOI: http://doi.org/10.3346/jkms.2016.31.9.1485
Abstract
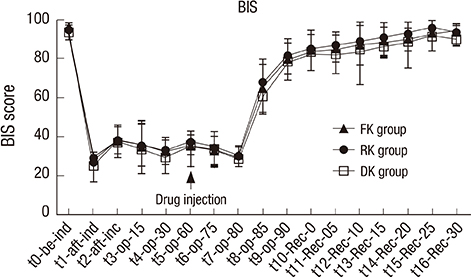
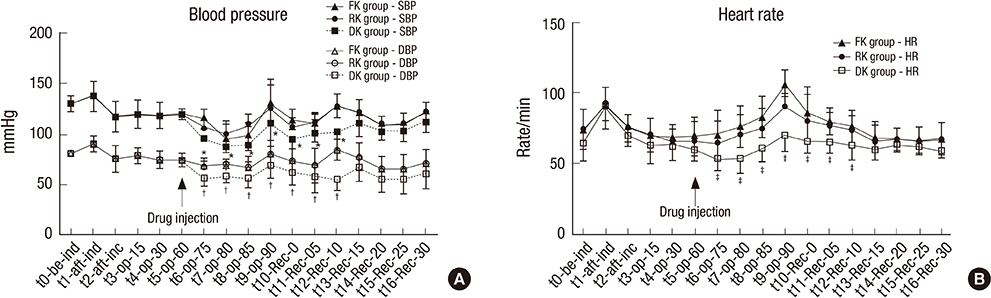
- We aimed to compare fentanyl, remifentanil and dexmedetomidine with respect to hemodynamic stability, postoperative pain control and achievement of sedation at the postanesthetic care unit (PACU). In this randomized double-blind study, 90 consecutive total laparoscopic hysterectomy patients scheduled for elective surgery were randomly assigned to receive fentanyl (1.0 µg/kg) over 1 minute followed by a 0.4 µg/kg/hr infusion (FK group, n = 30), or remifentanil (1.0 µg/kg) over 1 minute followed by a 0.08 µg/kg/min infusion (RK group, n = 30), or dexmedetomidine (1 µg/kg) over 10 minutes followed by a 0.5 µg/kg/hr infusion (DK group, n = 30) initiating at the end of main procedures of the operation to the time in the PACU. A single dose of intravenous ketorolac (30 mg) was given to all patients at the end of surgery. We respectively evaluated the pain VAS scores, the modified OAA/S scores, the BIS, the vital signs and the perioperative side effects to compare the efficacy of fentanyl, remifentanil and dexmedetomidine. Compared with other groups, the modified OAA/S scores were significantly lower in DK group at 0, 5 and 10 minutes after arrival at the PACU (P < 0.05), whereas the pain VAS and BIS were not significantly different from other groups. The blood pressure and heart rate in the DK group were significantly lower than those of other groups at the PACU (P < 0.05). DK group, at sedative doses, had the better postoperative hemodynamic stability than RK group or FK group and demonstrated a similar effect of pain control as RK group and FK group with patient awareness during sedation in the PACU. (World Health Organization registry, KCT0001524).
MeSH Terms
-
Adolescent
Adult
Analgesics, Opioid/*administration & dosage/adverse effects
Blood Pressure
Dexmedetomidine/*administration & dosage/adverse effects
Double-Blind Method
Female
Fentanyl/*administration & dosage/adverse effects
Heart Rate
Hemodynamics/physiology
Humans
Hypotension/etiology
Laparoscopy
Male
Middle Aged
Nausea/etiology
Pain Management
Pain, Postoperative/*drug therapy
Piperidines/*administration & dosage/adverse effects
Young Adult
Analgesics, Opioid
Piperidines
Dexmedetomidine
Remifentanil
Fentanyl
Figure
Reference
-
1. Kamibayashi T, Maze M. Clinical uses of alpha2 -adrenergic agonists. Anesthesiology. 2000; 93:1345–1349.2. Hall JE, Uhrich TD, Barney JA, Arain SR, Ebert TJ. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg. 2000; 90:699–705.3. Venn RM, Hell J, Grounds RM. Respiratory effects of dexmedetomidine in the surgical patient requiring intensive care. Crit Care. 2000; 4:302–308.4. Bhana N, Goa KL, McClellan KJ. Dexmedetomidine. Drugs. 2000; 59:263–268.5. Bekker A, Sturaitis MK. Dexmedetomidine for neurological surgery. Neurosurgery. 2005; 57:1–10.6. Bloor BC, Ward DS, Belleville JP, Maze M. Effects of intravenous dexmedetomidine in humans. II. Hemodynamic changes. Anesthesiology. 1992; 77:1134–1142.7. Yaksh TL, Pogrel JW, Lee YW, Chaplan SR. Reversal of nerve ligation-induced allodynia by spinal alpha-2 adrenoceptor agonists. J Pharmacol Exp Ther. 1995; 272:207–214.8. Busick T, Kussman M, Scheidt T, Tobias JD. Preliminary experience with dexmedetomidine for monitored anesthesia care during ENT surgical procedures. Am J Ther. 2008; 15:520–527.9. Precedex (dexmedetomidine hydrochloride) [package insert]. Lake Forest, IL: Hospira, Inc.;2008.10. Mester R, Easley RB, Brady KM, Chilson K, Tobias JD. Monitored anesthesia care with a combination of ketamine and dexmedetomidine during cardiac catheterization. Am J Ther. 2008; 15:24–30.11. Joo HS, Kapoor S, Rose DK, Naik VN. The intubating laryngeal mask airway after induction of general anesthesia versus awake fiberoptic intubation in patients with difficult airways. Anesth Analg. 2001; 92:1342–1346.12. Guo TZ, Jiang JY, Buttermann AE, Maze M. Dexmedetomidine injection into the locus ceruleus produces antinociception. Anesthesiology. 1996; 84:873–881.13. Arain SR, Ruehlow RM, Uhrich TD, Ebert TJ. The efficacy of dexmedetomidine versus morphine for postoperative analgesia after major inpatient surgery. Anesth Analg. 2004; 98:153–158.14. Lu J, Nelson LE, Franks N, Maze M, Chamberlin NL, Saper CB. Role of endogenous sleep-wake and analgesic systems in anesthesia. J Comp Neurol. 2008; 508:648–662.15. Rampil IJ. A primer for EEG signal processing in anesthesia. Anesthesiology. 1998; 89:980–1002.16. Farber NE, Poterack KA, Schmeling WT. Dexmedetomidine and halothane produce similar alterations in electroencephalographic and electromyographic activity in cats. Brain Res. 1997; 774:131–141.17. Chrysostomou C, Schmitt CG. Dexmedetomidine: sedation, analgesia and beyond. Expert Opin Drug Metab Toxicol. 2008; 4:619–627.18. Bürkle H, Dunbar S, Van Aken H. Remifentanil: a novel, short-acting, mu-opioid. Anesth Analg. 1996; 83:646–651.19. Tipps LB, Coplin WM, Murry KR, Rhoney DH. Safety and feasibility of continuous infusion of remifentanil in the neurosurgical intensive care unit. Neurosurgery. 2000; 46:596–601.20. Cavaliere F, Antonelli M, Arcangeli A, Conti G, Costa R, Pennisi MA, Proietti R. A low-dose remifentanil infusion is well tolerated for sedation in mechanically ventilated, critically-ill patients. Can J Anaesth. 2002; 49:1088–1094.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of an intraoperative infusion of dexmedetomidine or fentanyl for the perioperative hemodynamics, achieving hypnosis and sedation, and the postoperative pain control
- Postoperative nausea and vomiting after thyroidectomy: a comparison between dexmedetomidine and remifentanil as part of balanced anesthesia
- Dexmedetomidine intravenous sedation using a patient-controlled sedation infusion pump: a case report
- The effect of remifentanil and ketamine on intraoperative hemodynamics and postoperative pain in gastrectomy with sevoflurane based anesthesia
- Effect of perioperative infusion of lidocaine vs. dexmedetomidine on reduced consumption of postoperative analgesics after laparoscopic cholecystectomy