Korean J Radiol.
2017 Feb;18(1):173-179. 10.3348/kjr.2017.18.1.173.
New Radiofrequency Device to Reduce Bleeding after Core Needle Biopsy: Experimental Study in a Porcine Liver Model
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 06351, Korea. rhimhc@skku.edu
- 2Department of Radiology, Hanyang University Guri Hospital, Hanyang University School of Medicine, Guri 11923, Korea.
- KMID: 2468131
- DOI: http://doi.org/10.3348/kjr.2017.18.1.173
Abstract
OBJECTIVE
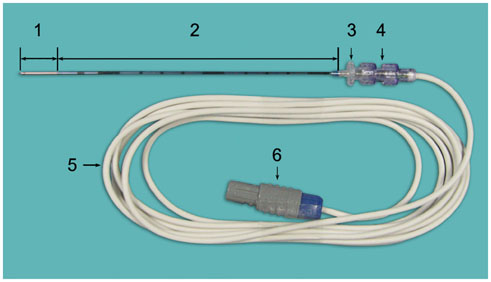
To evaluate the in vivo efficiency of the biopsy tract radiofrequency ablation for hemostasis after core biopsy of the liver in a porcine liver model, including situations with bleeding tendency and a larger (16-gauge) core needle.
MATERIALS AND METHODS
A preliminary study was performed using one pig to determine optimal ablation parameters. For the main experiment, four pigs were assigned to different groups according to heparinization use and biopsy needle caliber. In each pig, 14 control (without tract ablation) and 14 experimental (tract ablation) ultrasound-guided core biopsies were performed using either an 18- or 16-gauge needle. Post-biopsy bleeding amounts were measured by soaking up the blood for five minutes. The results were compared using the Mann-Whitney U test.
RESULTS
The optimal parameters for biopsy tract ablation were determined as a 2-cm active tip electrode set at 40-watt with a tip temperature of 70-80℃. The bleeding amounts in all experimental groups were smaller than those in the controls; however they were significant in the non-heparinized pig biopsied with an 18-gauge needle and in two heparinized pigs (p < 0.001). In the heparinized pigs, the mean blood loss in the experimental group was 3.5% and 13.5% of the controls biopsied with an 18- and 16-gauge needle, respectively.
CONCLUSION
Radiofrequency ablation of hepatic core biopsy tract ablation may reduce post-biopsy bleeding even under bleeding tendency and using a larger core needle, according to the result from in vivo porcine model experiments.
Keyword
MeSH Terms
Figure
Reference
-
1. Korean Liver Cancer Study Group (KLCSG). National Cancer Center, Korea (NCC). 2014 Korean Liver Cancer Study Group-National Cancer Center Korea practice guideline for the management of hepatocellular carcinoma. Korean J Radiol. 2015; 16:465–552.2. Ma X, Arellano RS, Gervais DA, Hahn PF, Mueller PR, Sahani DV. Success of image-guided biopsy for small (≤ 3 cm) focal liver lesions in cirrhotic and noncirrhotic individuals. J Vasc Interv Radiol. 2010; 21:1539–1547. quiz 1547.3. Sporea I, Gherhardt D, Popescu A, Sirli R, Cornianu M, Herman D, et al. Does the size of the needle influence the number of portal tracts obtained through percutaneous liver biopsy? Ann Hepatol. 2012; 11:691–695.4. McAfee JH, Keeffe EB, Lee RG, Rösch J. Transjugular liver biopsy. Hepatology. 1992; 15:726–732.5. Allison DJ, Adam A. Percutaneous liver biopsy and track embolization with steel coils. Radiology. 1988; 169:261–263.6. Falstrom JK, Moore MM, Caldwell SH, Matsumoto AH, Abbott RD, Spotnitz WD. Use of fibrin sealant to reduce bleeding after needle liver biopsy in an anticoagulated canine model: work in progress. J Vasc Interv Radiol. 1999; 10:457–462.7. Fandrich CA, Davies RP, Hall PM. Small gauge gelfoam plug liver biopsy in high risk patients: safety and diagnostic value. Australas Radiol. 1996; 40:230–234.8. Paulson EK, Stephenson GR, Neal MC, Rossin V, Lawson JH. Use of fibrin sealant as a hemostatic agent after liver biopsy in swine. J Vasc Interv Radiol. 2000; 11:905–911.9. Smith TP, McDermott VG, Ayoub DM, Suhocki PV, Stackhouse DJ. Percutaneous transhepatic liver biopsy with tract embolization. Radiology. 1996; 198:769–774.10. Zins M, Vilgrain V, Gayno S, Rolland Y, Arrivé L, Denninger MH, et al. US-guided percutaneous liver biopsy with plugging of the needle track: a prospective study in 72 high-risk patients. Radiology. 1992; 184:841–843.11. Bruners P, Penzkofer T, Isfort P, Pfeffer J, Schmitz-Rode T, Günther RW, et al. A trucut biopsy needle for bipolar radiofrequency ablation of needle tract: a proof-of-concept experiment. Eur Radiol. 2010; 20:2000–2004.12. Laeseke PF, Winter TC 3rd, Davis CL, Stevens KR, Johnson CD, Fronczak FJ, et al. Postbiopsy bleeding in a porcine model: reduction with radio-frequency ablation--preliminary results. Radiology. 2003; 227:493–499.13. Pritchard WF, Wray-Cahen D, Karanian JW, Hilbert S, Wood BJ. Radiofrequency cauterization with biopsy introducer needle. J Vasc Interv Radiol. 2004; 15(2 Pt 1):183–187.14. Choi SH, Lee JM, Lee KH, Kim SH, Lee JY, Han JK, et al. Postbiopsy splenic bleeding in a dog model: comparison of cauterization, embolization, and plugging of the needle tract. AJR Am J Roentgenol. 2005; 185:878–884.15. Kang TW, Lim HK, Lee MW, Kim YS, Choi D, Rhim H. First-line radiofrequency ablation with or without artificial ascites for hepatocellular carcinomas in a subcapsular location: local control rate and risk of peritoneal seeding at long-term follow-up. Clin Radiol. 2013; 68:e641–e651.16. Nahum Goldberg S, Dupuy DE. Image-guided radiofrequency tumor ablation: challenges and opportunities--part I. J Vasc Interv Radiol. 2001; 12:1021–1032.17. McGhana JP, Dodd GD 3rd. Radiofrequency ablation of the liver: current status. AJR Am J Roentgenol. 2001; 176:3–16.18. Zervas NT, Kuwayama A. Pathological characteristics of experimental thermal lesions. Comparison of induction heating and radiofrequency electrocoagulation. J Neurosurg. 1972; 37:418–422.19. Chan SL, Wong AM, Lee K, Wong N, Chan AK. Personalized therapy for hepatocellular carcinoma: where are we now? Cancer Treat Rev. 2016; 45:77–86.20. Zhang B, Finn RS. Personalized clinical trials in hepatocellular carcinoma based on biomarker selection. Liver Cancer. 2016; 5:221–232.21. Chang S, Kim SH, Lim HK, Kim SH, Lee WJ, Choi D, et al. Needle tract implantation after percutaneous interventional procedures in hepatocellular carcinomas: lessons learned from a 10-year experience. Korean J Radiol. 2008; 9:268–274.22. Kim JW, Shin SS, Heo SH, Hong JH, Lim HS, Seon HJ, et al. Ultrasound-guided percutaneous radiofrequency ablation of liver tumors: how we do it safely and completely. Korean J Radiol. 2015; 16:1226–1239.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Management of Bleeding from the Superior Thyroid Artery after Core Needle Biopsy
- Pseudoaneurysm of the Breast after Core Needle Biopsy: A Case Report
- Track Seeding in a Breast Cancer Patient after a 14-Gauge Core Needle Biopsy: A Case Report
- Thyroid Nodules with Nondiagnostic FNA Results: Role of Core Needle Biopsy
- Radiofrequency Thermal Ablation of Benign Cystic Lesion:An Experimental Pilot Study in a Porcine Gallbladder Model