Korean Circ J.
2020 Feb;50(2):120-129. 10.4070/kcj.2019.0166.
Clopidogrel versus Aspirin after Dual Antiplatelet Therapy in Acute Myocardial Infarction Patients Undergoing Drug-Eluting Stenting
- Affiliations
-
- 1Department of Cardiovascular Medicine, Chonnam National University Hospital, Gwangju, Korea. myungho@chollian.net
- 2Department of Cardiology, Seoul National University Hospital, Seoul, Korea.
- 3Department of Cardiology, Samsung Medical Center, Sungkyunkwan University, Seoul, Korea.
- 4Department of Cardiology, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 5Cardiovascular Center, Korea University Guro Hospital, Seoul, Korea.
- 6Department of Cardiology, Kyungpook National University Hospital, Daegu, Korea.
- 7Department of Cardiology, Kyung Hee University Hospital at Gangdong, Seoul, Korea.
- 8Department of Cardiology, Pusan National University Hospital, Busan, Korea.
- 9Division of Cardiology, Yeungnam University Hospital, Daegu, Korea.
- 10Division of Cardiology, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 11Department of Cardiology, Chunbuk National University Hospital, Jeonju, Korea.
- 12Department of Cardiology, Jeju National University Hospital, Jeju, Korea.
- 13Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea.
- 14Department of Cardiology, Keimyung University Dongsan Medical Center, Daegu, Korea.
- 15Department of Cardiology, Chungnam National University Hospital, Daejeon, Korea.
- 16Department of Cardiology, Chungbuk National University Hospital, Cheongju, Korea.
- 17Department of Cardiology, Inje University Haeundae Paik Hospital, Busan, Korea.
- 18Department of Cardiology, Wonkwang University Hospital, Iksan, Korea.
- 19Department of Cardiology, Gachon University Gil Medical Center, Incheon, Korea.
- 20Department of Cardiology, Kyungsang National University Hospital, Jinju, Korea.
- KMID: 2468037
- DOI: http://doi.org/10.4070/kcj.2019.0166
Abstract
- BACKGROUND AND OBJECTIVES
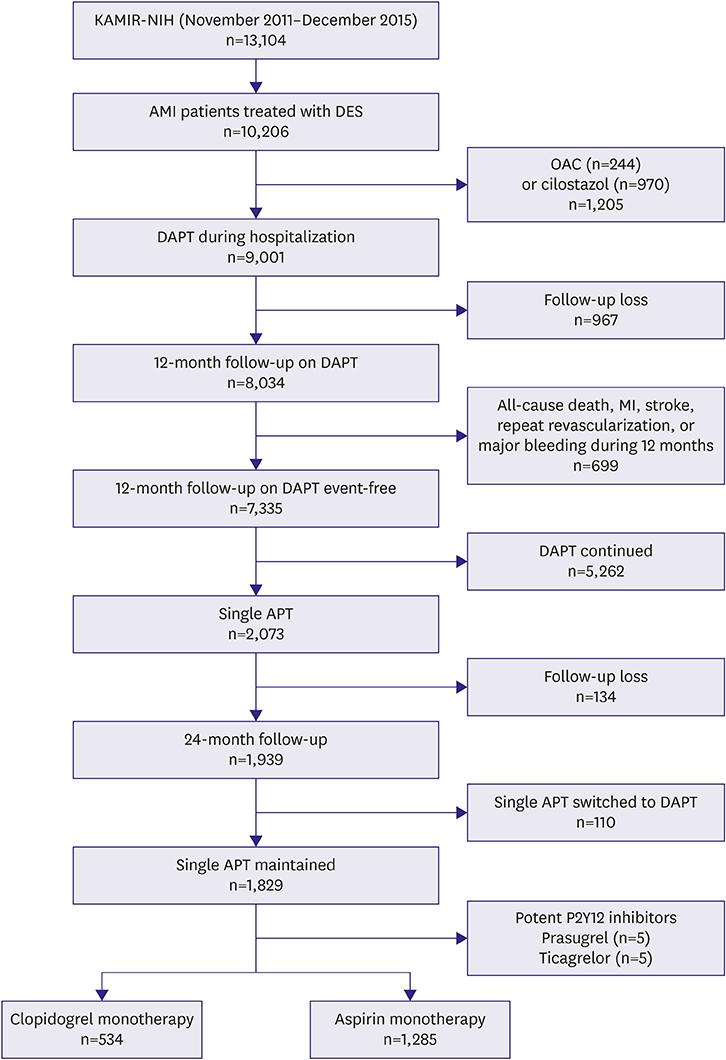
There is a paucity of data regarding the benefit of clopidogrel monotherapy after dual antiplatelet therapy (DAPT) in patients treated with drug-eluting stents (DES). This study compared outcome between clopidogrel versus aspirin as monotherapy after DES for acute myocardial infarction (MI).
METHODS
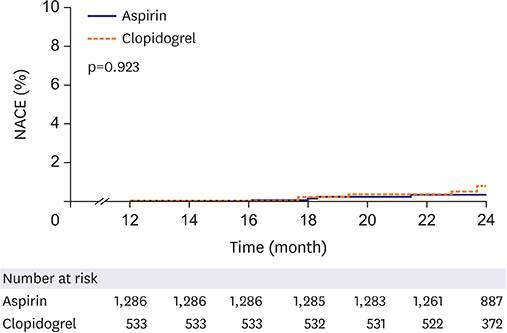
From Korea Acute Myocardial Infarction Registry-National Institute of Health database, 1,819 patients treated with DES who were switched to monotherapy with clopidogrel (n=534) or aspirin (n=1,285) after uneventful 12-month DAPT were analyzed. The primary endpoint was net adverse clinical events (NACE), defined as a composite of death from any cause, MI, repeat percutaneous coronary intervention (PCI), stent thrombosis, ischemic stroke, or major bleeding during the period from 12 to 24 months.
RESULTS
After adjustment using inverse probability of treatment weighting, patients who received clopidogrel, compared with those treated with aspirin, had a similar incidence of NACE (0.7% and 0.7%; hazard ratio, 1.06; 95% confidence interval, 0.31-3.60; p=0.923). The 2 groups had similar rates of death from any cause (0.1% in each group, p=0.789), MI (0.3% and 0.1%, respectively; p=0.226), repeat PCI (0.1% and 0.3%, respectively; p=0.548), stent thrombosis (0.1% and 0%, respectively; p=0.121), major bleeding (0.2% in each group, p=0.974), and major adverse cardiovascular and cerebrovascular events (0.5% in each group, p=0.924).
CONCLUSIONS
Monotherapy with clopidogrel, compared to aspirin, after DAPT showed similar clinical outcomes in patients with acute MI treated with DES.
MeSH Terms
Figure
Cited by 2 articles
-
Aspirin Monotherapy beyond 12 Months of Dual Antiplatelet Therapy in Patients with Acute Myocardial Infarction: Oldies But Goodies?
Jung-Won Suh
Korean Circ J. 2020;50(2):130-132. doi: 10.4070/kcj.2019.0390.Implementation of National Health Policy for the Prevention and Control of Cardiovascular Disease in South Korea: Regional-Local Cardio-Cerebrovascular Center and Nationwide Registry
Ju Mee Wang, Byung Ok Kim, Jang-Whan Bae, Dong-Jin Oh
Korean Circ J. 2021;51(5):383-398. doi: 10.4070/kcj.2021.0001.
Reference
-
1. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2016; 68:1082–1115.2. Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the task force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018; 39:213–260.3. CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee. Lancet. 1996; 348:1329–1339.4. Kim JH, Chae SC, Oh DJ, et al. Multicenter cohort study of acute myocardial infarction in Korea - interim analysis of the Korea acute myocardial infarction registry-national institutes of health registry. Circ J. 2016; 80:1427–1436.5. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013; 61:e78–140.6. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014; 64:e139–e228.7. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019; 40:237–269.
Article8. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009; 361:1045–1057.9. Mauri L, Hsieh WH, Massaro JM, Ho KK, D'Agostino R, Cutlip DE. Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med. 2007; 356:1020–1029.
Article10. Rao AK, Pratt C, Berke A, et al. Thrombolysis in Myocardial Infarction (TIMI) trial--phase I: hemorrhagic manifestations and changes in plasma fibrinogen and the fibrinolytic system in patients treated with recombinant tissue plasminogen activator and streptokinase. J Am Coll Cardiol. 1988; 11:1–11.
Article11. Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015; 34:3661–3679.
Article12. Lunceford JK, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effects: a comparative study. Stat Med. 2004; 23:2937–2960.
Article13. Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008; 168:656–664.
Article14. Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. 2014; 33:1242–1258.
Article15. Costa F, van Klaveren D, James S, et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet. 2017; 389:1025–1034.
Article16. Yeh RW, Secemsky EA, Kereiakes DJ, et al. Development and validation of a prediction rule for benefit and harm of dual antiplatelet therapy beyond 1 year after percutaneous coronary intervention. JAMA. 2016; 315:1735–1749.
Article17. Antithrombotic Trialists' Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002; 324:71–86.18. Berger JS, Brown DL, Becker RC. Low-dose aspirin in patients with stable cardiovascular disease: a meta-analysis. Am J Med. 2008; 121:43–49.
Article19. Park TK, Song YB, Ahn J, et al. Clopidogrel versus aspirin as an antiplatelet monotherapy after 12-month dual-antiplatelet therapy in the era of drug-eluting stents. Circ Cardiovasc Interv. 2016; 9:e002816.
Article20. Hankey GJ, Sudlow CL, Dunbabin DW. Thienopyridine derivatives (ticlopidine, clopidogrel) versus aspirin for preventing stroke and other serious vascular events in high vascular risk patients. Cochrane Database Syst Rev. 2000; CD001246.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aspirin and Clopidogrel Resistance in Drug Eluting Stent Era
- Management of Perioperative Antiplatelet Therapy
- A Case of Ticagrelor Rescue Therapy in a Patient with Subacute Stent Thrombosis
- Very Late Stent Thrombosis after Drug-Eluting Stent Implantation in a Patient without Aspirin and Clopidogrel Resistance
- The Effect of Cilostazol on Stent Thrombosis After Drug-Eluting Stent Implantation