J Clin Neurol.
2019 Oct;15(4):438-447. 10.3988/jcn.2019.15.4.438.
Altered Regional Cerebral Blood Flow Associated with Mood and Sleep in Shift Workers: Cerebral Perfusion Magnetic Resonance Imaging Study
- Affiliations
-
- 1Department of Neurology, Bundang Jesaeng General Hospital, Seongnam, Korea.
- 2Department Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. st7.kim@samsung.com
- 3Department of Nursing, Samsung Medical Center, Department of Clinical Nursing Science, Graduate School of Clinical Nursing Science, Sungkyunkwan University, Seoul, Korea.
- 4Department of Neurology, Neuroscience Center, Samsung Biomedical Research Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ejoo@skku.edu
- 5Department of Health Sciences and Technology, Samsung Advanced Institute for Health Sciences & Technology, Sungkyunkwan University, Seoul, Korea.
- KMID: 2467751
- DOI: http://doi.org/10.3988/jcn.2019.15.4.438
Abstract
- BACKGROUND AND PURPOSE
Shift work disrupts the body's circadian rhythms and increases the risk of health problems. Despite evidence of neuropsychological disturbances in shift workers (SW), the brain functional status as measured by brain perfusion in chronic shift work has not been evaluated previously. We investigated the regional cerebral blood flow (rCBF) in SW using perfusion MRI (pMRI) and evaluated the relationships between altered rCBF and sleep, mood, psychometric measures, and quality of life.
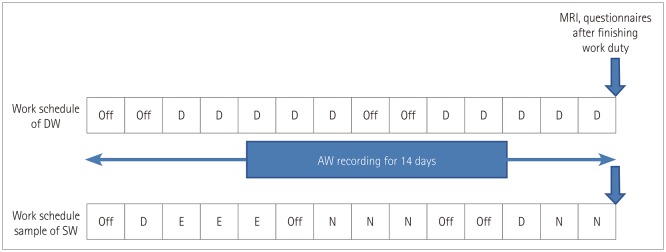
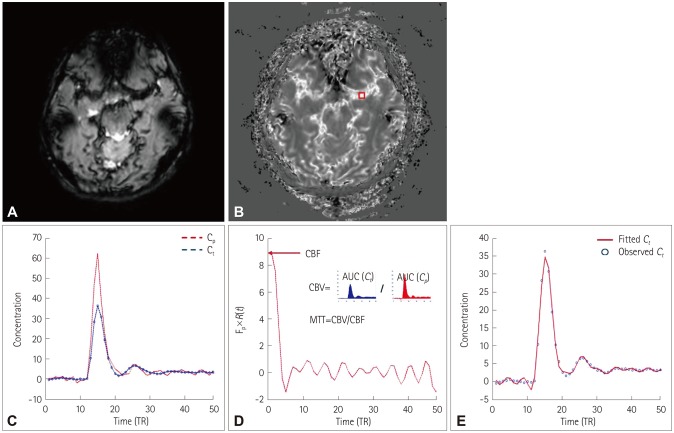
METHODS
Fifteen rotational SW and 15 day workers (DW) were enrolled. The participants were all female nurses working at a university-affiliated hospital. During 2 weeks of actigraphy they underwent pMRI scanning and psychometric testing on the last day immediately after working. Demographic characteristics, insomnia, daytime sleepiness, and mood were compared between the groups.
RESULTS
The participants were aged 35.3±2.9 years (mean±SD) and had been performing their current work for more than 2 years. The demographic characteristics did not differ between SW and DW, but the levels of insomnia, anxiety, depression, and hyperactivity-restlessness in psychometric measures were higher in SW than in DW. Cerebral perfusion in SW was significantly decreased in the cuneus, fusiform/parahippocampal gyri, and cerebellum of the right hemisphere, while it was increased in the inferior occipital gyrus of the left hemisphere. Perfusion changes in SW were significantly correlated with depression and insomnia severity. The onset and duration irregularity of sleep among SW were related to insomnia, mood, hyperactivity/ restlessness, and quality of life.
CONCLUSIONS
SW experience considerably more insomnia and mood disturbances than do DW, and this is significantly related to perfusion changes in multiple brain areas.
Keyword
MeSH Terms
Figure
Reference
-
1. Vogel M, Braungardt T, Meyer W, Schneider W. The effects of shift work on physical and mental health. J Neural Transm (Vienna). 2012; 119:1121–1132. PMID: 22488445.
Article2. Logan RW, McClung CA. Rhythms of life: circadian disruption and brain disorders across the lifespan. Nat Rev Neurosci. 2019; 20:49–65. PMID: 30459365.
Article3. Benca R, Duncan MJ, Frank E, McClung C, Nelson RJ, Vicentic A. Biological rhythms, higher brain function, and behavior: gaps, opportunities, and challenges. Brain Res Rev. 2009; 62:57–70. PMID: 19766673.
Article4. Karatsoreos IN, Bhagat S, Bloss EB, Morrison JH, McEwen BS. Disruption of circadian clocks has ramifications for metabolism, brain, and behavior. Proc Natl Acad Sci U S A. 2011; 108:1657–1662. PMID: 21220317.
Article5. Kim JB, Kim JH. Regional gray matter changes in shift workers: a voxel-based morphometry study. Sleep Med. 2017; 30:185–188. PMID: 28215246.
Article6. Debernard L, Melzer TR, Alla S, Eagle J, Van Stockum S, Graham C, et al. Deep grey matter MRI abnormalities and cognitive function in relapsing-remitting multiple sclerosis. Psychiatry Res. 2015; 234:352–361. PMID: 26602610.
Article7. Poudel GR, Innes CR, Jones RD. Cerebral perfusion differences between drowsy and nondrowsy individuals after acute sleep restriction. Sleep. 2012; 35:1085–1096. PMID: 22851804.
Article8. Innes CR, Kelly PT, Hlavac M, Melzer TR, Jones RD. Decreased regional cerebral perfusion in moderate-severe obstructive sleep apnoea during wakefulness. Sleep. 2015; 38:699–706. PMID: 25669185.
Article9. Huang YC, Liu HL, Lee JD, Yang JT, Weng HH, Lee M, et al. Comparison of arterial spin labeling and dynamic susceptibility contrast perfusion MRI in patients with acute stroke. PLoS One. 2013; 8:e69085. PMID: 23874876.
Article10. Jahng GH, Li KL, Ostergaard L, Calamante F. Perfusion magnetic resonance imaging: a comprehensive update on principles and techniques. Korean J Radiol. 2014; 15:554–577. PMID: 25246817.
Article11. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991; 14:540–545. PMID: 1798888.
Article12. Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976; 4:97–110. PMID: 1027738.13. Morin CM. Insomnia: Psychological assessment and management. New York: Guilford Press;1994.14. World Health Organization. WHOQOL-BREF introduction, administration, scoring and generic version of the assessment. Field trial version. Geneva: World Health Organization;1996.15. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67:361–370. PMID: 6880820.
Article16. Conners CK, Erhardt D, Sparrow E. Conners adult ADHD rating scales (CAARS). New York: Multi Health Systems, Inc.;1999.17. Lee DH, Cho CH, Han C, Bok KN, Moon JH, Lee E, et al. Sleep irregularity in the previous week influences the first-night effect in polysomnographic studies. Psychiatry Investig. 2016; 13:203–209.
Article18. Warwick JM, Carey P, Jordaan GP, Dupont P, Stein DJ. Resting brain perfusion in social anxiety disorder: a voxel-wise whole brain comparison with healthy control subjects. Prog Neuropsychopharmacol Biol Psychiatry. 2008; 32:1251–1256. PMID: 18485554.
Article19. Ostergaard L, Sorensen AG, Kwong KK, Weisskoff RM, Gyldensted C, Rosen BR. High resolution measurement of cerebral blood flow using intravascular tracer bolus passages. Part II: experimental comparison and preliminary results. Magn Reson Med. 1996; 36:726–736. PMID: 8916023.20. Zöllner FG, Weisser G, Reich M, Kaiser S, Schoenberg SO, Sourbron SP, et al. UMMPerfusion: an open source software tool towards quantitative MRI perfusion analysis in clinical routine. J Digit Imaging. 2013; 26:344–352. PMID: 22832894.
Article21. Ma N, Li L, Shu N, Liu J, Gong G, He Z, et al. White matter abnormalities in first-episode, treatment-naive young adults with major depressive disorder. Am J Psychiatry. 2007; 164:823–826. PMID: 17475743.
Article22. Kroes MC, Rugg MD, Whalley MG, Brewin CR. Structural brain abnormalities common to posttraumatic stress disorder and depression. J Psychiatry Neurosci. 2011; 36:256–265. PMID: 21418787.
Article23. Harvey PO, Pruessner J, Czechowska Y, Lepage M. Individual differences in trait anhedonia: a structural and functional magnetic resonance imaging study in non-clinical subjects. Mol Psychiatry. 2007; 12:703767–775. PMID: 17505465.
Article24. Schmahmann JD. The role of the cerebellum in cognition and emotion: personal reflections since 1982 on the dysmetria of thought hypothesis, and its historical evolution from theory to therapy. Neuropsychol Rev. 2010; 20:236–260. PMID: 20821056.
Article25. Stoodley CJ, Schmahmann JD. Evidence for topographic organization in the cerebellum of motor control versus cognitive and affective processing. Cortex. 2010; 46:831–844. PMID: 20152963.
Article26. Xu LY, Xu FC, Liu C, Ji YF, Wu JM, Wang Y, et al. Relationship between cerebellar structure and emotional memory in depression. Brain Behav. 2017; 7:e00738. PMID: 28729943.
Article27. Lui S, Parkes LM, Huang X, Zou K, Chan RC, Yang H, et al. Depressive disorders: focally altered cerebral perfusion measured with arterial spin-labeling MR imaging. Radiology. 2009; 251:476–484. PMID: 19401575.
Article28. Surguladze S, Brammer MJ, Keedwell P, Giampietro V, Young AW, Travis MJ, et al. A differential pattern of neural response toward sad versus happy facial expressions in major depressive disorder. Biol Psychiatry. 2005; 57:201–209. PMID: 15691520.
Article29. Kay DB, Buysse DJ. Hyperarousal and beyond: new insights to the pathophysiology of insomnia disorder through functional neuroimaging studies. Brain Sci. 2017; 7:E23. PMID: 28241468.
Article30. Huang X, Li SH, Zhou FQ, Zhang Y, Zhong YL, Cai FQ, et al. Altered intrinsic regional brain spontaneous activity in patients with comitant strabismus: a resting-state functional MRI study. Neuropsychiatr Dis Treat. 2016; 12:1303–1308. PMID: 27350747.31. Kay DB, Karim HT, Soehner AM, Hasler BP, Wilckens KA, James JA, et al. Sleep-wake differences in relative regional cerebral metabolic rate for glucose among patients with insomnia compared with good sleepers. Sleep. 2016; 39:1779–1794. PMID: 27568812.
Article32. Wang Y, Zhong S, Jia Y, Zhou Z, Wang B, Pan J, et al. Interhemispheric resting state functional connectivity abnormalities in unipolar depression and bipolar depression. Bipolar Disord. 2015; 17:486–495. PMID: 26241359.
Article33. Medeiros AL, Mendes DB, Lima PF, Araujo JF. The relationships between sleep-wake cycle and academic performance in medical students. Biol Rhythm Res. 2001; 32:263–270.
Article34. Santhi N, Lazar AS, McCabe PJ, Lo JC, Groeger JA, Dijk DJ. Sex differences in the circadian regulation of sleep and waking cognition in humans. Proc Natl Acad Sci U S A. 2016; 113:E2730–E2739. PMID: 27091961.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of regional cerebral blood flow (rCBF) in ischemic stroke using Tc-99m HMPAO SPECT: comparison with CT and MR findings
- The Usefulness of Perfusion CT in Acute Cerebral Ischemic Infarction
- Measurements of Cerebral Blood Flow in Delayed Carbon Monoxide Sequelae Using Xenon lnhalation CT Scan
- Measurement of Regional Cerebral Blood Volume in Normal Rabbits on Perfusion-weighted MR Image
- Hyperperfusion in DWI Abnormality in a Patient with Acute Symptomatic Hypoglycemic Encephalopathy