J Clin Neurol.
2019 Apr;15(2):235-242. 10.3988/jcn.2019.15.2.235.
A Multicenter, Randomized Clinical Trial to Assess the Efficacy of a Therapeutic Intervention Program for Caregivers of People with Dementia
- Affiliations
-
- 1Department of Neurology, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea. jjeong@ewha.ac.kr
- 2Department of Psychology, Hallym University, Chuncheon, Korea.
- 3Department of Neurology, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 4Department of Neurology, Keimyung University College of Medicine, Dongsan Medical Center, Daegu, Korea.
- 5Department of Neurology, Inha University School of Medicine, Incheon, Korea.
- 6Department of Neurology, Bobath Memorial Hospital, Seongnam, Korea.
- 7Department of Neurology, Hallym University Dongtan Sacred Heart Hospital, Hwaseong, Korea.
- 8Department of Psychiatry, Hallym University Chuncheon Sacred Heart Hospital, Chuncheon, Korea.
- 9Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2467738
- DOI: http://doi.org/10.3988/jcn.2019.15.2.235
Abstract
- BACKGROUND AND PURPOSE
Caregivers experience tremendous social, financial, physical, and psychological burdens in caring for people with dementia. This study aimed to determine the efficacy of a multicomponent therapeutic intervention program for the caregivers of people with dementia (CGPWD) through a multicenter clinical trial: the intervention program-caregivers of people with dementia study.
METHODS
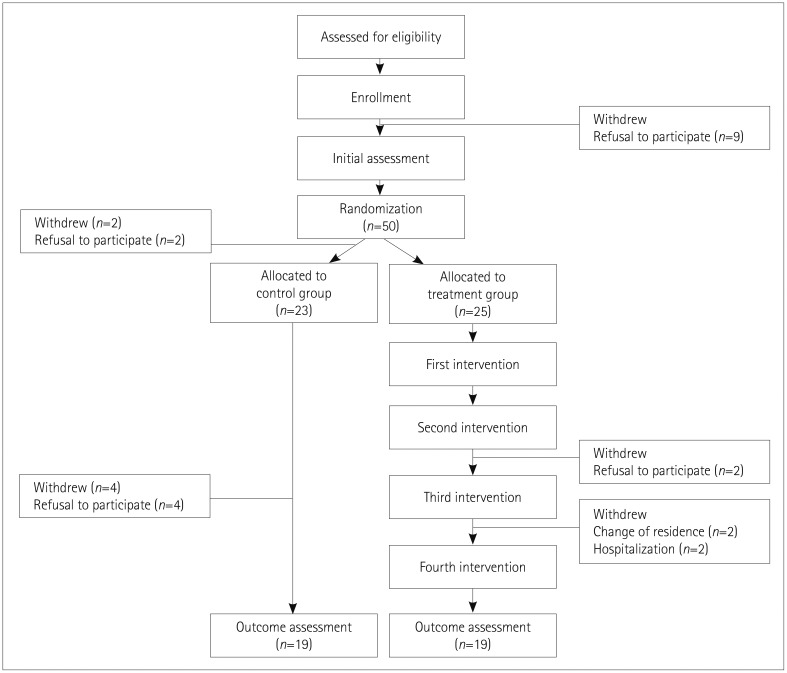
The 38 caregivers of dementia patients at 8 sites were randomized into 2 groups: treatment (n=19) and control (n=19). The treatment group received the intervention program for 8-10 weeks, including one group session for dementia education and three individual sessions (on cognitive behavioral therapy, coping with stress, and stress management) and single targeted training for daily activities. The Korean version of the Zarit Burden Interview (ZBI-K) and the Geriatric Depression Scale (GDS) were evaluated at pre- and postintervention as primary efficacy measures.
RESULTS
The treatment group displayed significant improvements in scores on the ZBI-K and GDS. The ZBI-K score at postintervention was significantly reduced in the treatment group compared to that in the control group [6.2-point decrease vs. 3.7-point increase, t(37)=−2.9, p<0.01]. There was a significant difference in the GDS score between the treatment and control groups [2.2-point decrease vs. 1.3-point increase, t(18)=2.5, p<0.05].
CONCLUSIONS
The findings of this study imply that a multicomponent therapeutic intervention program is effective in reducing the burden experienced by and depression among CGPWD. Further research is warranted to investigate the long-term effects of the intervention program for CGPWD.
Keyword
Figure
Reference
-
1. National Institute of Dementia (KR). National Institute of Dementia annual report 2017. Seongnam: National Institute of Dementia;2018.2. George LK, Gwyther LP. Caregiver well-being: a multidimensional examination of family caregivers of demented adults. Gerontologist. 1986; 26:253–259. PMID: 3721232.3. Dauphinot V, Delphin-Combe F, Mouchoux C, Dorey A, Bathsavanis A, Makaroff Z, et al. Risk factors of caregiver burden among patients with Alzheimer’s disease or related disorders: a cross-sectional study. J Alzheimers Dis. 2015; 44:907–916. PMID: 25374109.
Article4. Garand L, Dew MA, Eazor LR, DeKosky ST, Reynolds CF 3rd. Caregiving burden and psychiatric morbidity in spouses of persons with mild cognitive impairment. Int J Geriatr Psychiatry. 2005; 20:512–522. PMID: 15920711.
Article5. Epstein-Lubow G. Family caregiver health: what to do when a spouse or child needs help. Med Health R I. 2009; 92:106–107. PMID: 19385387.6. Youn GH. Cultural differences in psychological burden and caregiving obligation of primary caregivers for senile dementia patients. J Korean Geriatr Soc. 1998; 18:75–90.7. Steinberg M, Tschanz JT, Corcoran C, Steffens DC, Norton MC, Lyketsos CG, et al. The persistence of neuropsychiatric symptoms in dementia: the Cache County Study. Int J Geriatr Psychiatry. 2004; 19:19–26. PMID: 14716695.
Article8. Aalten P, De Vugt ME, Jaspers N, Jolles J, Verhey FR. The course of neuropsychiatric symptoms in dementia. Part I: findings from the two-year longitudinal Maasbed study. Int J Geriatr Psychiatry. 2005; 20:523–530. PMID: 15920712.9. Luppa M, Luck T, Brähler E, König HH, Riedel-Heller SG. Prediction of institutionalisation in dementia. A systematic review. Dement Geriatr Cogn Disord. 2008; 26:65–78. PMID: 18617737.10. Gaugler JE, Kane RL, Kane RA, Newcomer R. Early community-based service utilization and its effects on institutionalization in dementia caregiving. Gerontologist. 2005; 45:177–185. PMID: 15799982.
Article11. Kwon OY, Ahn HS, Kim HJ, Park KW. Effectiveness of cognitive behavioral therapy for caregivers of people with dementia: a systematic review and meta-analysis. J Clin Neurol. 2017; 13:394–404. PMID: 29057632.
Article12. Yeom J, Yoo R, Bae S, Kang Y, Kim GH, Na HR, et al. Recent updates of therapeutic intervention programs for caregivers of patient with dementia: proposal of hospital-based individual therapy. Dement Neurocognitive Disord. 2016; 15:29–36.
Article13. Morris JC. The clinical dementia rating (CDR): current version and scoring rules. Neurology. 1993; 43:2412–2414.14. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997; 15:300–308.15. Elliott AF, Burgio LD, Decoster J. Enhancing caregiver health: findings from the resources for enhancing Alzheimer’s caregiver health II intervention. J Am Geriatr Soc. 2010; 58:30–37. PMID: 20122038.
Article16. Lee HS, Kim DK, Ko HJ, Ku HM, Kwon EJ, Kim JH. Measurement of stress in the caregivers of dementia patients: reliability and validity of the revised-memory and behavior problem checklist and the burden interview. Korean J Clin Psychol. 2004; 23:1029–1050.17. Park M, Park MH, Kim HH. Effects of a multimodal psychoeducational program on burden, depression, and problem coping behaviors in family caregivers of patients with dementia. J Korean Gerontol Nurs. 2015; 17:10–19.
Article18. Cho MJ, Bae JN, Suh GH, Hahm BJ, Kim JK, Lee DW, et al. Validation of geriatric depression scale, Korean version(GDS) in the assessment of DSM-III-R major depression. J Korean Neuropsychiatr Assoc. 1999; 38:48–63.19. Ryu K, Kim JH, Kang YW, Rie JI. A validation study of the Korean version of Philadelphia Geriatric Center for Morale Scale. J Korean Geriatr Soc. 2012; 32:207–222.20. Kang SJ, Choi SH, Lee BH, Jeong Y, Hahm DS, Han IW, et al. Caregiver-administered neuropsychiatric inventory (CGA-NPI). J Geriatr Psychiatry Neurol. 2004; 17:32–35. PMID: 15018695.
Article21. Lee HH, Kim EJ, Lee MK. A validation study of Korea positive and negative affect schedule: the PANAS scales. Korean J Clin Psychol. 2003; 22:935–946.22. Heo JH, Choi MS, Jin HJ. Study on the reliability and validity of Korean translated Acceptance-Action Questionnaire-II. Korean J Couns Psychother. 2009; 21:861–878.23. Kim KE, Yi GD, Cho YR, Chai SH, Lee WK. The validation study of the Korean version of the Self-Compassion Scale. Korean J Health Psychol. 2008; 13:1023–1044.24. Choi JY, Jeong H, Park JY, Kim TH, Lee DY, Lee DW, et al. Factors associated with the attitudes toward dementia in community caregivers: results from the nationwide survey on dementia care in Korea. J Korean Geriatr Psychiatry. 2015; 19:24–31.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Updates of Therapeutic Intervention Programs for Caregivers of Patient with Dementia: Proposal of Hospital-Based Individual Therapy
- The Effects of Emotion-focused Individual Intervention for Family Caregivers of People with Early Stages of Dementia
- Effects of Korean Dementia Simulation Program for Caregivers of the Elderly with Dementia : A Pilot Study
- Factors Affecting On Caregiving Self-efficacy among Dementia Caregivers
- Effects of a Dementia Family Education Program for Dementia Recognition, Burden, and Depression in Caregivers of Elders with Dementia