J Clin Neurol.
2019 Apr;15(2):205-210. 10.3988/jcn.2019.15.2.205.
Effect of Food Intake on Hemodynamic Parameters during the Tilt-Table Test in Patients with Postural Orthostatic Tachycardia Syndrome
- Affiliations
-
- 1Department of Neurology, School of Medicine, University of Zagreb, Zagreb, Croatia. mhabek@mef.hr
- 2Department of Neurology, University Hospital Center Zagreb, Referral Center for Autonomic Nervous System Disorders, Zagreb, Croatia.
- KMID: 2467734
- DOI: http://doi.org/10.3988/jcn.2019.15.2.205
Abstract
- BACKGROUND AND PURPOSE
The aim of this study was to determine the effect of food intake on the heart rate (HR) in postural orthostatic tachycardia syndrome (POTS).
METHODS
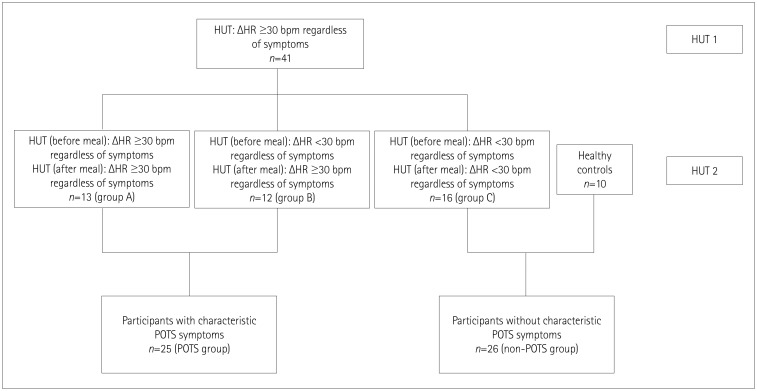
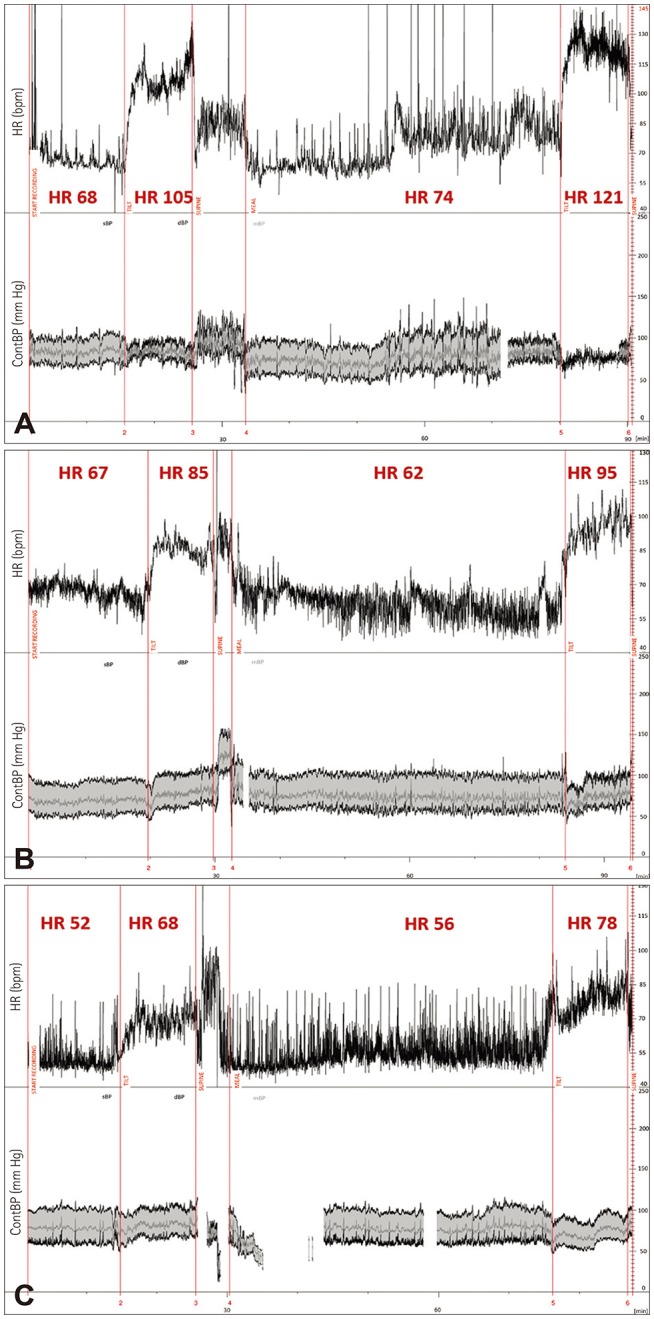
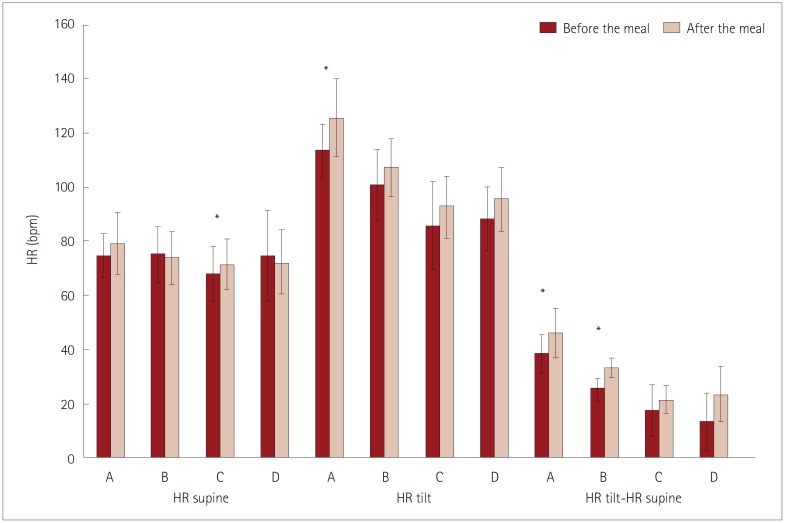
The following five-phase protocol was applied to 41 subjects who had a sustained HR increment of ≥30 beats/min within 10 min of standing in an initial tilt-table test: 1) 10-min supine phase, 2) 10-min 70°-tilted phase, 3) ingestion of 400 mL of Nutridrink Multi Fibre®, 4) 45-min supine phase, and 5) 10-min 70°-tilted phase. Subjects were divided into four groups: A) difference in HR for standing vs. supine (ΔHR) before the meal of ≥30 beats/min (n=13), B) ΔHR <30 beats/min before the meal but ≥30 beats/min after the meal (n=12), and C) ΔHR <30 beats/min both before and after the meal (n=16). Group D consisted of 10 healthy subjects.
RESULTS
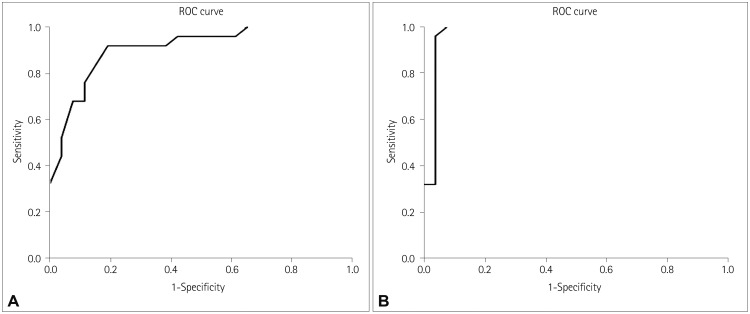
Before the meal, ΔHR was significantly higher in group A than in all of the other groups, and in group B than in group D (p<0.001). After the meal, ΔHR was significantly higher in groups A and B (p<0.001 and p<0.0001, respectively). When we pooled patients (according to their symptoms) from group A and B into a POTS group and from group C and D into a non-POTS group, an increase in HR of 25 beats/min before the meal had a sensitivity of 92.0% and a specificity of 80.8%. After the meal, an increase in HR of 30 beats/min had a sensitivity of 96.0% and a specificity of 96.2%.
CONCLUSIONS
Food intake can significantly alter the results of the tilt-table test and so should be taken into account when diagnosing POTS.
MeSH Terms
Figure
Reference
-
1. Garland EM, Celedonio JE, Raj SR. Postural tachycardia syndrome: beyond orthostatic intolerance. Curr Neurol Neurosci Rep. 2015; 15:60. PMID: 26198889.
Article2. Raj SR. Postural tachycardia syndrome (POTS). Circulation. 2013; 127:2336–2342. PMID: 23753844.
Article3. Robertson D. The epidemic of orthostatic tachycardia and orthostatic intolerance. Am J Med Sci. 1999; 317:75–77. PMID: 10037110.
Article4. Adamec I, Lovrić M, Žaper D, Barušić AK, Bach I, Junaković A, et al. Postural orthostatic tachycardia syndrome associated with multiple sclerosis. Auton Neurosci. 2013; 173:65–68. PMID: 23246200.
Article5. Agarwal AK, Garg R, Ritch A, Sarkar P. Postural orthostatic tachycardia syndrome. Postgrad Med J. 2007; 83:478–480. PMID: 17621618.
Article6. Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res. 2011; 21:69–72. PMID: 21431947.
Article7. Trahair LG, Horowitz M, Jones KL. Postprandial hypotension: a systematic review. J Am Med Dir Assoc. 2014; 15:394–409. PMID: 24630686.
Article8. Masuda Y, Kawamura A. Role of the autonomic nervous system in postprandial hypotension in elderly persons. J Cardiovasc Pharmacol. 2003; 42(Suppl 1):S23–S26. PMID: 14871024.
Article9. Fagius J, Ellerfelt K, Lithell H, Berne C. Increase in muscle nerve sympathetic activity after glucose intake is blunted in the elderly. Clin Auton Res. 1996; 6:195–203. PMID: 8902315.
Article10. Pavelić A, Krbot Skorić M, Crnošija L, Habek M. Postprandial hypotension in neurological disorders: systematic review and meta-analysis. Clin Auton Res. 2017; 27:263–271. PMID: 28647892.
Article11. Tani H, Singer W, McPhee BR, Opfer-Gehrking TL, Haruma K, Kajiyama G, et al. Splanchnic-mesenteric capacitance bed in the postural tachycardia syndrome (POTS). Auton Neurosci. 2000; 86:107–113. PMID: 11269915.
Article12. Crnošija L, Krbot Skorić M, Adamec I, Lovrić M, Junaković A, Mišmaš A, et al. Hemodynamic profile and heart rate variability in hyperadrenergic versus non-hyperadrenergic postural orthostatic tachycardia syndrome. Clin Neurophysiol. 2016; 127:1639–1644. PMID: 26386646.
Article13. Seligman WH, Low DA, Asahina M, Mathias CJ. Abnormal gastric myoelectrical activity in postural tachycardia syndrome. Clin Auton Res. 2013; 23:73–80. PMID: 23212662.
Article14. Pitt MS, Hainsworth R. Contrasting effects of carbohydrate and water on blood pressure responses to postural maneuvers in patients with posturally related (vasovagal) syncope. Clin Auton Res. 2004; 14:249–254. PMID: 15316842.
Article15. Imai C, Muratani H, Kimura Y, Kanzato N, Takishita S, Fukiyama K. Effects of meal ingestion and active standing on blood pressure in patients ≥60 years of age. Am J Cardiol. 1998; 81:1310–1314. PMID: 9631968.
Article16. Puisieux F, Boumbar Y, Bulckaen H, Bonnin E, Houssin F, Dewailly P. Intraindividual variability in orthostatic blood pressure changes among older adults: the influence of meals. J Am Geriatr Soc. 1999; 47:1332–1336. PMID: 10573442.
Article17. Rowell LB. Regulation of splanchnic blood flow in man. Physiologist. 1973; 16:127–142. PMID: 4713808.18. Fujimura J, Camilleri M, Low PA, Novak V, Novak P, Opfer-Gehrking TL. Effect of perturbations and a meal on superior mesenteric artery flow in patients with orthostatic hypotension. J Auton Nerv Syst. 1997; 67:15–23. PMID: 9470140.
Article19. Chaudhuri KR, Thomaides T, Hernandez P, Alam M, Mathias CJ. Noninvasive quantification of superior mesenteric artery blood flow during sympathoneural activation in normal subjects. Clin Auton Res. 1991; 1:37–42. PMID: 1821664.
Article20. Mathias CJ, Mallipeddi R, Bleasdale-Barr K. Symptoms associated with orthostatic hypotension in pure autonomic failure and multiple system atrophy. J Neurol. 1999; 246:893–898. PMID: 10552235.
Article21. Z'Graggen WJ, Hess CW, Humm AM. Acute fluid ingestion in the treatment of orthostatic intolerance - important implications for daily practice. Eur J Neurol. 2010; 17:1370–1376. PMID: 20412295.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Adrenergic Function: Tilt-Table and Valsalva Test
- Orthostatic Intolerance Syndrome
- Orthostatic symptoms does not always manifest during tilt-table test in pediatric postural orthostatic tachycardia syndrome patients
- Clinical Significance and Update of Postural Orthostatic Tachycardia Syndrome
- Diagnostic approach of orthostatic dizziness/vertigo