Korean J Radiol.
2020 Jan;21(1):68-76. 10.3348/kjr.2019.0010.
Using 2-mSv Appendiceal CT in Usual Practice for Adolescents and Young Adults: Willingness Survey of 579 Radiologists, Emergency Physicians, and Surgeons from 20 Hospitals
- Affiliations
-
- 1Department of Radiology, Daejin Medical Center, Bundang Jesaeng General Hospital, Seongnam, Korea.
- 2Department of Radiology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. kholeemail@gmail.com
- 3Program in Biomedical Radiation Sciences, Department of Transdisciplinary Studies, Graduate School of Convergence Science and Technology Seoul National University, Seoul, Korea.
- 4Department of Radiology, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 5Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea.
- 6Department of Radiology, Asan Medical Center, Seoul, Korea.
- KMID: 2467043
- DOI: http://doi.org/10.3348/kjr.2019.0010
Abstract
OBJECTIVE
To survey care providers' willingness to use 2-mSv computed tomography (CT) in their usual practice for adolescents and young adults with suspected appendicitis.
MATERIALS AND METHODS
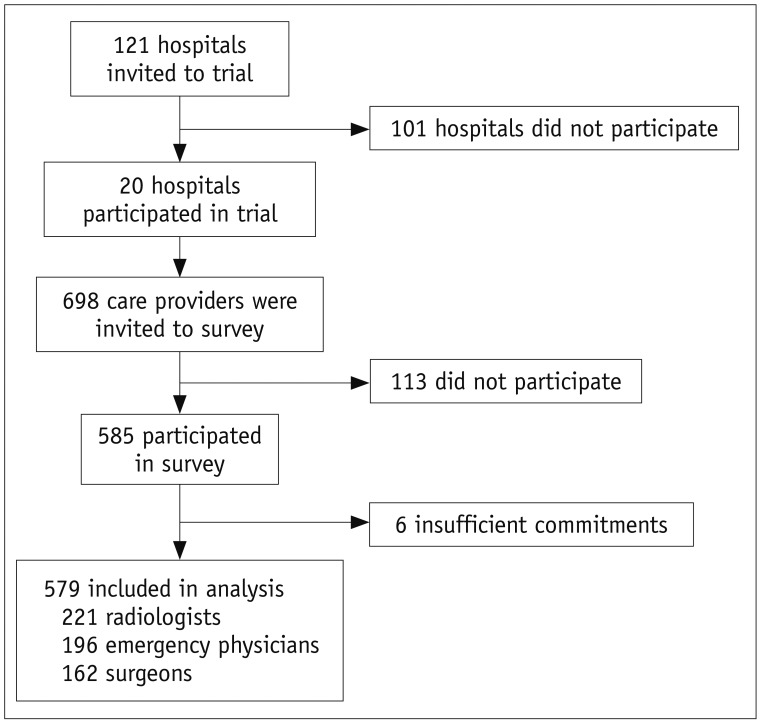
An ethical committee approved this prospective study. We introduced 2-mSv CT in 20 hospitals through a pragmatic clinical trial. At the final phase of the trial, we invited 698 potentially-involved care providers in the survey regarding their willingness to use 2-mSv CT. Multivariable logistic regression analyses were performed to identify factors associated with willingness. Nine months after the completion of the trial patient recruitment, we surveyed whether the hospitals were using 2-mSv CT in usual practice.
RESULTS
The analyses included responses from 579 participants (203 attendings and 376 trainees; 221 radiologists, 196 emergency physicians, and 162 surgeons). Regarding the willingness to immediately change their standard practice to 2-mSv CT, 158 (27.3%), 375 (64.8%), and 46 (7.9%) participants responded as "yes" (consistently), "partly" (selectively), and "no", respectively. Willingness varied considerably across the hospitals, but only slightly across the participants' departments or job titles. Willingness was significantly associated with attendings (p = 0.004), intention to maintain the dedicated appendiceal CT protocol (p < 0.001), belief in compelling evidence on the carcinogenic risk of conventional-dose CT radiation (p = 0.028), and hospitals having more than 1000 beds (p = 0.031). Fourteen of the 20 hospitals kept using 2-mSv appendiceal CT in usual practice after the trial.
CONCLUSION
Despite the extensive efforts over the years of this clinical trial, many care providers were willing to use 2-mSv CT selectively or not willing to use.
MeSH Terms
Figure
Reference
-
1. Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015; 386:1278–1287. PMID: 26460662.
Article2. Drake FT, Florence MG, Johnson MG, Jurkovich GJ, Kwon S, Schmidt Z, et al. SCOAP Collaborative. Progress in the diagnosis of appendicitis: a report from Washington State's Surgical Care and Outcomes Assessment Program. Ann Surg. 2012; 256:586–594. PMID: 22964731.3. Park JH. LOCAT Group. Diagnostic imaging utilization in cases of acute appendicitis: multi-center experience. J Korean Med Sci. 2014; 29:1308–1316. PMID: 25246752.
Article4. Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012; 380:499–505. PMID: 22681860.
Article5. Yoon HM, Suh CH, Cho YA, Kim JR, Lee JS, Jung AY, et al. The diagnostic performance of reduced-dose CT for suspected appendicitis in paediatric and adult patients: a systematic review and diagnostic meta-analysis. Eur Radiol. 2018; 28:2537–2548. PMID: 29327290.
Article6. Yun SJ, Ryu CW, Choi NY, Kim HC, Oh JY, Yang DM. Comparison of low- and standard-dose CT for the diagnosis of acute appendicitis: a meta-analysis. AJR Am J Roentgenol. 2017; 208:W198–W207. PMID: 28301209.
Article7. Kim SY, Lee KH, Kim K, Kim TY, Lee HS, Hwang SS, et al. Acute appendicitis in young adults: low-versus standard-radiation-dose contrast-enhanced abdominal CT for diagnosis. Radiology. 2011; 260:437–445. PMID: 21633052.8. Seo H, Lee KH, Kim HJ, Kim K, Kang SB, Kim SY, et al. Diagnosis of acute appendicitis with sliding slab ray-sum interpretation of low-dose unenhanced CT and standard-dose i.v. contrast-enhanced CT scans. AJR Am J Roentgenol. 2009; 193:96–105. PMID: 19542400.
Article9. Kim K, Kim YH, Kim SY, Kim S, Lee YJ, Kim KP, et al. Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med. 2012; 366:1596–1605. PMID: 22533576.
Article10. LOCAT Group. Low-dose CT for the diagnosis of appendicitis in adolescents and young adults (LOCAT): a pragmatic, multicentre, randomised controlled non-inferiority trial. Lancet Gastroenterol Hepatol. 2017; 2:793–804. PMID: 28919126.11. Weisenthal K, Karthik P, Shaw M, Sengupta D, Bhargavan-Chatfield M, Burleson J, et al. Evaluation of kidney stones with reduced-radiation dose CT: progress from 2011-2012 to 2015-2016-Not there yet. Radiology. 2018; 286:581–589. PMID: 28858562.
Article12. Ahn S. LOCAT group. LOCAT (low-dose computed tomography for appendicitis trial) comparing clinical outcomes following low- vs standard-dose computed tomography as the first-line imaging test in adolescents and young adults with suspected acute appendicitis: study protocol for a randomized controlled trial. Trials. 2014; 15:28. PMID: 24438500.
Article13. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010; 17:553–560. PMID: 20536812.
Article14. Dixon AK, Goldstone KE. Abdominal CT and the Euratom Directive. Eur Radiol. 2002; 12:1567–1570. PMID: 12042969.
Article15. United Nations. Report of the United Nations Scientific Committee on the effects of atomic radiation: sixtyfifth session. United Nations;2018. Accessed August 2, 2018. Available at: https://documents-dds-ny.un.org/doc/UNDOC/GEN/V08/558/99/PDF/V0855899.pdf?OpenElement.16. Motulsky H. Graphing continous data. In : Motulsky H, editor. Intuitive biostatistics: a nonmathematical guide to statistical thinking. 4th ed. New York, NY: Oxford University Press;2018. p. 63–74.17. Motulsky H. Multiple regression. In : Motulsky H, editor. Intuitive biostatistics: a nonmathematical guide to statistical thinking. 4th ed. New York, NY: Oxford University Press;2018. p. 378–394.18. Park JH, Kim B, Kim MS, Kim HJ, Ko Y, Ahn S, et al. Comparison of filtered back projection and iterative reconstruction in diagnosing appendicitis at 2-mSv CT. Abdom Radiol (NY). 2016; 41:1227–1236. PMID: 27315093.
Article19. Park SB, Kim MJ, Ko Y, Sim JY, Kim HJ, Lee KH. LOCAT Group. Structured reporting versus free-text reporting for appendiceal computed tomography in adolescents and young adults: preference survey of 594 referring physicians, surgeons, and radiologists from 20 hospitals. Korean J Radiol. 2019; 20:246–255. PMID: 30672164.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Structured Reporting versus Free-Text Reporting for Appendiceal Computed Tomography in Adolescents and Young Adults: Preference Survey of 594 Referring Physicians, Surgeons, and Radiologists from 20 Hospitals
- Appendiceal Visualization on 2-mSv CT vs. Conventional-Dose CT in Adolescents and Young Adults with Suspected Appendicitis: An Analysis of Large Pragmatic Randomized Trial Data
- Radiation Exposure to Physicians in the Emergency Department
- Analysis of factors affecting the unbalanced distribution of physicians’ working regions in South Korea
- Added Value of Coronal Reformations for Duty Radiologists and for Referring Physicians or Surgeons in the CT Diagnosis of Acute Appendicitis