Anat Cell Biol.
2019 Dec;52(4):390-396. 10.5115/acb.19.142.
The best vein to be accessed based on descriptive study of dorsal metacarpal vein
- Affiliations
-
- 1Department of Basic Medical Science, Faculty of Medicine, Al Balqa Applied University, Al Salt, Jordan.
- 2Department of Anatomy and Histology, Faculty of Medicine, University of Jordan, Amman, Jordan. a.shatarat@ju.edu.jo
- 3Dean of the Faculty of Medicine, Hashemite University, Zarqa, Jordan.
- 4Department of General Surgery, Faculty of Medicine, University of Jordan, Amman, Jordan.
- 5Department of Anesthesia and Intensive Care, Faculty of Medicine, University of Jordan, Amman, Jordan.
- KMID: 2466691
- DOI: http://doi.org/10.5115/acb.19.142
Abstract
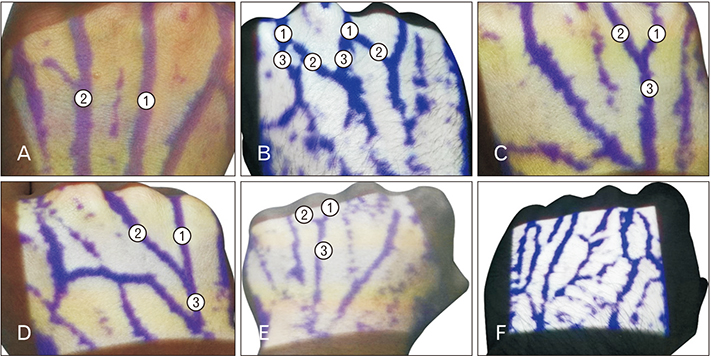
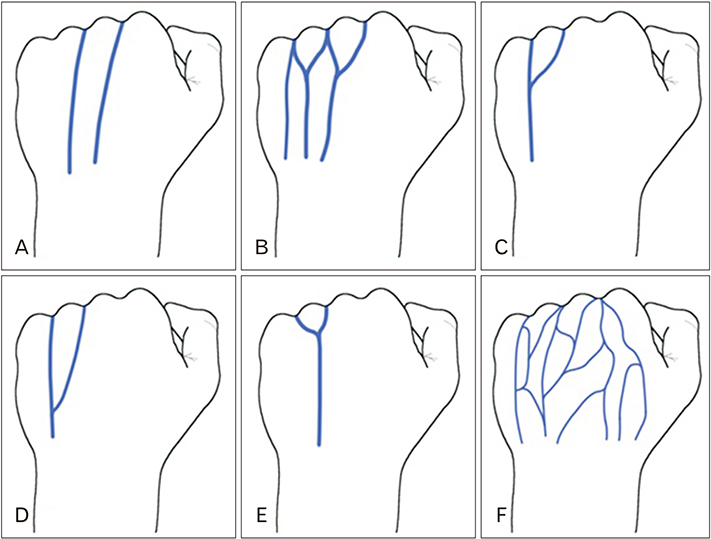
- It is well known that the most common sites for venous access are the superficial veins of the upper limb, particularly dorsal metacarpal veins and median cubital vein. Although dorsal metacarpal veins are the first choice for venous cannulation, there is scarce information about their anatomic variation. Hence, detailed anatomical information about these veins will improve the anatomic knowledge of the health care providers. Subsequently, this study was designed to study the dorsal metacarpal veins and to determine the most prominent dorsal metacarpal vein. A cross sectional study of 402 subjects (804 hands), was prepared to study the superficial veins on the dorsum of the hand among Jordanian students and staff of one of the major governmental medical colleges in Jordan, by using infrared illumination system. The obtained data was analyzed according to sex, sidedness, and handedness. Six locations of the most prominent dorsal metacarpal veins were identified. There was a significant relation between both females and males and the most prominent dorsal metacarpal vein (P=0.01). For the first time this study identified the most common location of the most prominent dorsal metacarpal vein in the fourth intermetacarpal space.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee SH, Chun KJ, Lee DS, Lee SY, Hwang J, Chon MK, Hwang KW, Kim JS, Park YH, Kim JH. Right cardiac catheterization using the antecubital fossa vein in Korean patients. Korean Circ J. 2016; 46:207–212.2. Scales K. Vascular access in the acute care setting. In : Dougherty L, Lamb J, editors. Intravenous Therapy in Nursing Practice. Oxford: Blackwell Publishing;2008. p. 261–299.3. Ortega R, Sekhar P, Song M, Hansen CJ, Peterson L. Videos in clinical medicine. Peripheral intravenous cannulation. N Engl J Med. 2008; 359:e26.4. Mbamalu D, Banerjee A. Methods of obtaining peripheral venous access in difficult situations. Postgrad Med J. 1999; 75:459–462.5. Cheung E, Baerlocher MO, Asch M, Myers A. Venous access: a practical review for 2009. Can Fam Physician. 2009; 55:494–496.6. King C, Henretig FM. Textbook of pediatric emergency procedures. Philadelphia, PA: Lippincott Williams & Wilkins;2008.7. Loukas M, Tubbs RS, Feldman J. Netter's introduction to clinical procedures. Philadelphia, PA: Elsevier Health Sciences;2016.8. Tan PC, Mackeen A, Khong SY, Omar SZ, Noor Azmi MA. Peripheral intravenous catheterisation in obstetric patients in the hand or forearm vein: a randomised trial. Sci Rep. 2016; 6:23223.9. Malamed SF. Sedation: a guide to patient management. 6th ed. St. Louis, MO: Elsevier;2017.10. Varma NR, Sahane SD, Thankre SS. Infrared VeinViewer. Int J Eng Educ Technol. 2014; 2:1–6.11. Kim MJ, Park JM, Rhee N, Je SM, Hong SH, Lee YM, Chung SP, Kim SH. Efficacy of VeinViewer in pediatric peripheral intravenous access: a randomized controlled trial. Eur J Pediatr. 2012; 171:1121–1125.12. Hess HA. A biomedical device to improve pediatric vascular access success. Pediatr Nurs. 2010; 36:259–263.13. Ukoha UU, Oranusi CK, Okafor JI, Ogugua PC, Obiaduo AO. Patterns of superficial venous arrangement in the cubital fossa of adult Nigerians. Niger J Clin Pract. 2013; 16:104–109.14. Hamzah AA, Ramasamy S, Adnan AS, Khan AH. Pattern of superficial venous of the cubital fossa among volunteers in a tertiary hospital. Trop Med Surg. 2014; 2:1000164.15. Elmegarhi SS, Amarin JZ, Hadidi MT, Badran DH, Massad IM, Bani-Hani AM, Shatarat AT. Dorsal metacarpal veins: anatomic variation and potential clinical implications. Anat Sci Int. 2018; 93:238–243.16. Dougherty L, Lamb J. Intravenous therapy in nursing practice. 2nd ed. Oxford: Blackwell Publishing;2008.17. Zhang SX, Schmidt HM. Clinical anatomy of the subcutaneous veins in the dorsum of the hand. Ann Anat. 1993; 175:381–384.18. Robson AJ, See MS, Ellis H. Applied anatomy of the superficial branch of the radial nerve. Clin Anat. 2008; 21:38–45.19. Samarakoon LB, Lakmal KC, Thillainathan S, Bataduwaarachchi VR, Anthony DJ, Jayasekara RW. Anatomical relations of the superficial sensory branches of the radial nerve: a cadaveric study with clinical implications. Patient Saf Surg. 2011; 5:28.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rupture of the communicating vein between superficial and deep dorsal vein of the penis during sexual intercourse: a case report
- A case of rupture of the communicating vein between deep dorsal and superficial dorsal vein of the penis during sexual intercouse
- Superficial Dorsal Vein Rupture Imitating Penile Fracture
- A Case of Hypervascularization of the Glans after Epigastrico-dorsal Vein Anastomosis
- Blood flow volume difference (P-SS) between the portal vein and thesum of splenic vein and superior mesenteric vein in portal hypertension