Blood Res.
2019 Dec;54(4):269-273. 10.5045/br.2019.54.4.269.
The increasing trend of blood donation in Iran
- Affiliations
-
- 1HIV/STI Surveillance Research Center, WHO Collaborating Center for HIV Surveillance, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran. zolalafarzaneh@gmail.com
- 2Blood Transfusion Research Center, High Institute for Research and Education in Transfusion Medicine, Tehran, Iran.
- 3Modeling in Health Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran.
- KMID: 2466592
- DOI: http://doi.org/10.5045/br.2019.54.4.269
Abstract
- BACKGROUND
This is the first study on the blood donation trend in Iran at a national level. We report different characteristics of blood donation such as demographic status, donor type, donation trend, and geographical distribution of blood donation in Iran between 2003 and 2017.
METHODS
This study used data registered in the donor vigilance part of the Iranian Blood Transfusion Organization. Statistical analysis was conducted using SPSS (SPSS Inc., Chicago, IL, USA) and ArcMap GIS version 10.2 software. A P-value <0.05 was considered statistically significant.
RESULTS
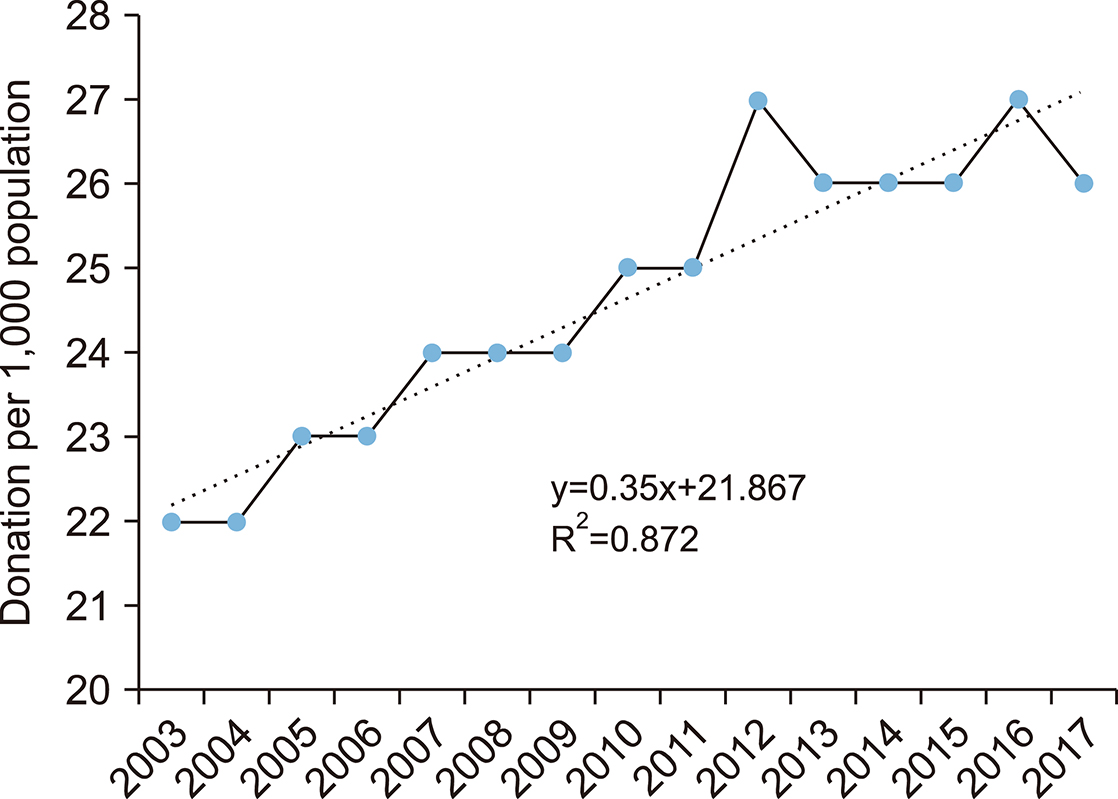
Based on the study results, blood donation in Iran reached >2 million units in 2017; moreover, it is predicted that Iran will achieve >29 donations per 1,000 population in 2022. The proportion of regular and repeated donors increased from 77% in 2013 to 87% in 2017. The average blood donation rate in seven provinces was higher than the national average, and the average growth rate of their blood donation per population was positive.
CONCLUSION
The results of the current study showed that there is a recent increasing trend toward blood donation in Iran. Furthermore, the largest share of donations is related to regular donors. The increasing proportion of regular and repeated donors has led to the improvement in the quality and consequently health level of donated blood.
Keyword
MeSH Terms
Figure
Reference
-
1. Cheraghali A. Overview of blood transfusion system of Iran: 2002-2011. Iran J Public Health. 2012; 41:89–93.2. Maghsudlu M, Nasizadeh S, Abolghasemi H, Ahmadyar S. Blood donation and donor recruitment in Iran from 1998 through 2007: ten years’ experience. Transfusion. 2009; 49:2346–2351.
Article3. Gharehbaghian A. Introduction of a program for voluntary blood donations in Iran (blood transfusion status in Iran). ISBT Sci Ser. 2012; 7:183–187.
Article4. Rigas AS, Pedersen OB, Erikstrup C, Hjalgrim H, Ullum H. Blood donation and iron deficiency. ISBT Sci Ser. 2017; 12:142–147.
Article5. Abolghasemi H, Amid A, Zeinali S, et al. Thalassemia in Iran: epidemiology, prevention, and management. J Pediatr Hematol Oncol. 2007; 29:233–238.6. Soodejani M, Shirani Faradonbeh R, Hashemi S, Zahedi A, Dehghani A. Epidemiology of accidents and injuries in the city of Lordegan in 2012: a short report. J Rafsanjan Univ Med Sci. 2015; 13:917–922.7. The WHO Global Database on Blood Safety (GDBS). Blood safety and availability. Geneva, Switzerland: World Health Organization. 2015. Accessed June 30, 2019. at https://www.who.int/news-room/fact-sheets/detail/blood-safety-and-availability.8. Ugwu AO, Madu AJ, Efobi CC, Ibegbulam OG. Pattern of blood donation and characteristics of blood donors in Enugu, Southeast Nigeria. Niger J Clin Pract. 2018; 21:1438–1443.9. Hâţu G, Brumboiu MI, Czernichow P, Bocşan IS. The risk for hepatitis C infection in blood donors in Cluj County, Romania. Transfus Clin Biol. 2014; 21:94–97.
Article10. Tessema B, Yismaw G, Kassu A, et al. Seroprevalence of HIV, HBV, HCV and syphilis infections among blood donors at Gondar University Teaching Hospital, Northwest Ethiopia: declining trends over a period of five years. BMC Infect Dis. 2010; 10:111.
Article11. Mooij SH, Hogema BM, Tulen AD, et al. Risk factors for hepatitis E virus seropositivity in Dutch blood donors. BMC Infect Dis. 2018; 18:173.
Article12. Liu Y, Zeng P, Wang J, et al. Hepatitis B virus infection in a cohort of HIV infected blood donors and AIDS patients in Sichuan, China. J Transl Med. 2014; 12:164.
Article13. Al-Rubaye A, Tariq Z, Alrubaiy L. Prevalence of hepatitis B seromarkers and hepatitis C antibodies in blood donors in Basra, Iraq. BMJ Open Gastroenterol. 2016; 3:e000067.
Article14. Nasrallah GK, Al Absi ES, Ghandour R, et al. Seroprevalence of hepatitis E virus among blood donors in Qatar (2013-2016). Transfusion. 2017; 57:1801–1807.
Article15. Arslan O. Whole blood donor deferral rate and characteristics of the Turkish population. Transfus Med. 2007; 17:379–383.
Article16. Tagny CT, Nguefack-Tsague G, Fopa D, et al. Risk factors for human immunodeficiency virus among blood donors in Cameroon: evidence for the design of an Africa-specific donor history questionnaire. Transfusion. 2017; 57:1912–1921.
Article17. Javadzadeh Shahshahani H. Why don't women volunteer to give blood? A study of knowledge, attitude and practice of women about blood donation, Yazd, Iran, 2005. Transfus Med. 2007; 17:451–454.
Article18. Rao C, Shetty J. Frequency of ABO and rhesus (D) blood groups in dakshina kannada district of karnataka - a study from rural tertiary care teaching hospital in South India. Nitte Univ J Health Sci. 2014; 4:57–60.
Article19. Tesfaye K, Petros Y, Andargie M. Frequency distribution of ABO and Rh (D) blood group alleles in Silte Zone, Ethiopia. Egypt J Med Hum Genet. 2015; 16:71–76.
Article20. Hassan FM. Frequency of ABO, subgroup ABO and Rh(D) blood groups in major sudanese ethnic groups. Pak J Med Res. 2010; 49:21–24.21. Jaff MS. ABO and rhesus blood group distribution in Kurds. J Blood Med. 2010; 1:143–146.
Article22. Mcarthur N, Penrose LS. World frequencies of the O, A and B blood group genes. Ann Eugen. 1951; 15:302–305.23. Birjandi F, Gharehbaghian A, Delavari A, Rezaie N, Maghsudlu M. Blood donor deferral pattern in Iran. Arch Iran Med. 2013; 16:657–660.24. Kasraian L, Negarestani N. Rates and reasons for blood donor deferral, Shiraz, Iran. A retrospective study. Sao Paulo Med J. 2015; 133:36–42.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study about the Directed blood donation program
- A Study on the Relationship between the Awareness of Blood Program and the Blood Donation Experience
- Factors Affecting Blood Donation Intentions of Nursing College Students
- Need for Patient Blood Management to Prepare for an Unstable Blood Supply Crisis
- Factors Affecting Blood Donation in University Students