Ann Surg Treat Res.
2020 Jan;98(1):23-30. 10.4174/astr.2020.98.1.23.
Unplanned conversion during minimally invasive liver resection for hepatocellular carcinoma: risk factors and surgical outcomes
- Affiliations
-
- 1Division of Hepatobiliary and Pancreas Surgery, Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. choigh@yuhs.ac
- KMID: 2466560
- DOI: http://doi.org/10.4174/astr.2020.98.1.23
Abstract
- PURPOSE
Unplanned conversion is sometimes necessary during minimally invasive liver resection (MILR) of hepatocellular carcinoma (HCC). The aims of this study were to compare surgical outcomes of planned MILR and unplanned conversion and to investigate the risk factors after unplanned conversion.
METHODS
We retrospectively analyzed 286 patients who underwent MILR with HCC from January 2006 to December 2017. All patients were divided into a MILR group and an unplanned conversion group. The clinicopathologic characteristics and outcomes were compared between the 2 groups. In addition, surgical outcomes in the conversion group were compared with the planned open surgery group (n = 505). Risk factors for unplanned conversion were analyzed.
RESULTS
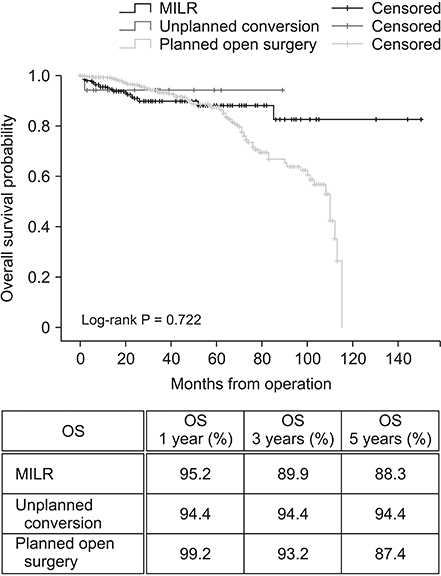
Of the 286 patients who underwent MILR, 18 patients (6.7%) had unplanned conversion during surgery. The unplanned conversion group showed statistically more blood loss, higher transfusion rate and postoperative complication rate, and longer hospital stay compared to the MILR group, whereas no such difference was observed in comparison with the planned open surgery group. There were no significant differences in overall and disease-free survival among 3 groups. The right-sided sectionectomy (right anterior and posterior sectionectomy), central bisectionectomy and tumor size were risk factors of unplanned conversion.
CONCLUSION
Unplanned conversion during MILR for HCC was associated with poor perioperative outcomes, but it did not affect long-term oncologic outcomes in our study. In addition, when planning right-sided sectionectomy or central bisectionectomy for a large tumor (more than 5 cm), we should recommend open surgery or MILR with an informed consent for unplanned open conversions.
MeSH Terms
Figure
Cited by 1 articles
-
A systematic review and meta-analysis of blood transfusion rates during liver resection by country
Seonju Kim, Yun Kyung Jung, Kyeong Geun Lee, Kyeong Sik Kim, Hanjun Kim, Dongho Choi, Sumi Lee, Boyoung Park
Ann Surg Treat Res. 2023;105(6):404-416. doi: 10.4174/astr.2023.105.6.404.
Reference
-
1. Han DH, Choi SH, Park EJ, Kang DR, Choi GH, Choi JS. Surgical outcomes after laparoscopic or robotic liver resection in hepatocellular carcinoma: a propensity-score matched analysis with conventional open liver resection. Int J Med Robot. 2016; 12:735–742.
Article2. Stiles ZE, Glazer ES, Deneve JL, Shibata D, Behrman SW, Dickson PV. Long-term implication of unplanned conversion during laparoscopic liver resection for hepatocellular carcinoma. Ann Surg Oncol. 2019; 26:282–289.3. Andreou A, Struecker B, Raschzok N, Krenzien F, Haber P, Wabitsch S, et al. Minimal-invasive versus open hepatectomy for hepatocellular carcinoma: comparison of postoperative outcomes and long-term survivals using propensity score matching analysis. Surg Oncol. 2018; 27:751–758.
Article4. Choi GH, Chong JU, Han DH, Choi JS, Lee WJ. Robotic hepatectomy: the Korean experience and perspective. Hepatobiliary Surg Nutr. 2017; 6:230–238.
Article5. Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015; 261:619–629.6. Stiles ZE, Behrman SW, Glazer ES, Deneve JL, Dong L, Wan JY, et al. Predictors and implications of unplanned conversion during minimally invasive hepatectomy: an analysis of the ACS-NSQIP database. HPB (Oxford). 2017; 19:957–965.
Article7. Troisi RI, Montalti R, Van Limmen JG, Cavaniglia D, Reyntjens K, Rogiers X, et al. Risk factors and management of conversions to an open approach in laparoscopic liver resection: analysis of 265 consecutive cases. HPB (Oxford). 2014; 16:75–82.
Article8. Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009; 250:831–841.
Article9. Silva JP, Berger NG, Yin Z, Liu Y, Tsai S, Christians KK, et al. Minimally invasive hepatectomy conversions: an analysis of risk factors and outcomes. HPB (Oxford). 2018; 20:132–139.
Article10. Vigano L, Laurent A, Tayar C, Tomatis M, Ponti A, Cherqui D. The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg. 2009; 250:772–782.11. Cauchy F, Fuks D, Nomi T, Schwarz L, Barbier L, Dokmak S, et al. Risk factors and consequences of conversion in laparoscopic major liver resection. Br J Surg. 2015; 102:785–795.
Article12. Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg. 2009; 250:825–830.13. Choi SH, Choi GH, Han DH, Choi JS. Laparoscopic liver resection using a rubber band retraction technique: usefulness and perioperative outcome in 100 consecutive cases. Surg Endosc. 2015; 29:387–397.
Article14. Choi GH, Choi SH, Kim SH, Hwang HK, Kang CM, Choi JS, et al. Robotic liver resection: technique and results of 30 consecutive procedures. Surg Endosc. 2012; 26:2247–2258.
Article15. Morise Z, Wakabayashi G. First quarter century of laparoscopic liver resection. World J Gastroenterol. 2017; 23:3581–3588.
Article16. Gagner M, Rheault M, Dubuc J. Laparoscopic partial hepatectomy for liver tumors. Surg Endosc. 1992; 6:97–98.17. Gupta R, Fuks D, Bourdeaux C, Radkani P, Nomi T, Lamer C, et al. Impact of intraoperative blood loss on the short-term outcomes of laparoscopic liver resection. Surg Endosc. 2017; 31:4451–4457.
Article18. Halls MC, Cipriani F, Berardi G, Barkhatov L, Lainas P, Alzoubi M, et al. Conversion for unfavorable intraoperative events results in significantly worse outcomes during laparoscopic liver resection: lessons learned from a multicenter review of 2861 cases. Ann Surg. 2018; 268:1051–1057.19. Costi R, Scatton O, Haddad L, Randone B, Andraus W, Massault PP, et al. Lessons learned from the first 100 laparoscopic liver resections: not delaying conversion may allow reduced blood loss and operative time. J Laparoendosc Adv Surg Tech A. 2012; 22:425–431.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk factors and long-term implications of unplanned conversion during laparoscopic liver resection for hepatoc cellular carcinoma located in anterolateral liver segment
- How to minimize conversion to open surgery during laparoscopic liver resection: the point of view of hemostasis
- Surgical Perspectives of Hepatocellular Carcinoma beyond the Barcelona Clinical Liver Cancer Guideline; Focusing on Liver Resection
- Minimally invasive surgery for maximally invasive tumors—pelvic exenterations for rectal cancers: are we prepared?
- Liver Transplantation in Mixed Hepatocellular Carcinoma and Cholangiocarcinoma