Ann Surg Treat Res.
2020 Jan;98(1):7-14. 10.4174/astr.2020.98.1.7.
Short- and long-term outcomes of pancreaticoduodenectomy in elderly patients with periampullary cancer
- Affiliations
-
- 1Department of Surgery and Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 2Center for Liver and Pancreatobiliary Cancer, National Cancer Center, Goyang, Korea. sunkim@snu.ac.kr
- KMID: 2466558
- DOI: http://doi.org/10.4174/astr.2020.98.1.7
Abstract
- PURPOSE
Pancreaticoduodenectomy (PD) is recently performed in older cancer patients. The complication rate of PD is high. The present study was to compare the postoperative short- and long-term outcomes of PD in between older patients and younger patients.
METHODS
Between 2000 and 2014, patients who underwent PD due to periampullary cancers were enrolled. Patients aged 75 years or over were included in the older group.
RESULTS
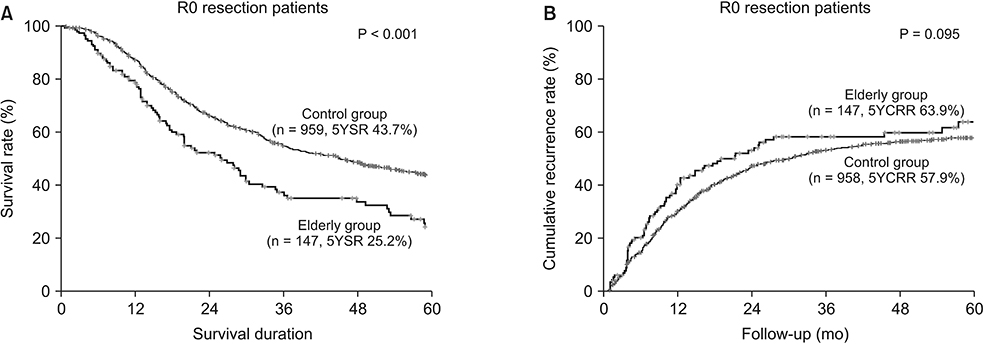
Total 1,249 patients were enrolled in this study and 168 patients (13.5%) were included in the older group. Postoperative complication rates, duration of postoperative hospital stay, and 30-day mortality were comparable between the 2 groups, although the admission rate of intensive care unit postoperatively was higher in the older adult group (20.8% vs. 10.5%, P < 0.001). In terms of long-term outcomes, 5-year overall survival rate was lower in the older group (23.4% vs. 41.8%, P < 0.001), and 5-year cumulative recurrence rate was higher in the older group without statistical significance (63.9% vs. 57.9%, P = 0.095). However, there were no statistical differences of cumulative recurrence in pancreatic cancer patients (81.5% vs. 82.5%, P = 0.805).
CONCLUSION
PD for periampullary cancer is a safe and feasible treatment in the older patients. The treatment modality for obtaining better survival outcomes will be investigated.
MeSH Terms
Figure
Cited by 1 articles
-
Surgical management for elderly patients with pancreatic cancer
Sun-Whe Kim
Ann Surg Treat Res. 2023;105(2):63-68. doi: 10.4174/astr.2023.105.2.63.
Reference
-
1. Eshuis WJ, van Eijck CH, Gerhards MF, Coene PP, de Hingh IH, Karsten TM, et al. Antecolic versus retrocolic route of the gastroenteric anastomosis after pancreatoduodenectomy: a randomized controlled trial. Ann Surg. 2014; 259:45–51.2. Casadei R, Zanini N, Morselli-Labate AM, Calculli L, Pezzilli R, Poti O, et al. Prognostic factors in periampullary and pancreatic tumor resection in elderly patients. World J Surg. 2006; 30:1992–2001.
Article3. Kang CM, Kim JY, Choi GH, Kim KS, Choi JS, Lee WJ, et al. Pancreaticoduodenectomy of pancreatic ductal adenocarcinoma in the elderly. Yonsei Med J. 2007; 48:488–494.
Article4. Katai H, Sasako M, Sano T, Maruyama K. The outcome of surgical treatment for gastric carcinoma in the elderly. Jpn J Clin Oncol. 1998; 28:112–115.
Article5. Kim DY, Joo JK, Ryu SY, Park YK, Kim YJ, Kim SK. Clinicopathologic characteristics of gastric carcinoma in elderly patients: a comparison with young patients. World J Gastroenterol. 2005; 11:22–26.
Article6. Lee CR, Lim JH, Kim SH, Ahn SH, Park YN, Choi GH, et al. A comparative analysis of hepatocellular carcinoma after hepatic resection in young versus elderly patients. J Gastrointest Surg. 2012; 16:1736–1743.
Article7. Gerstenhaber F, Grossman J, Lubezky N, Itzkowitz E, Nachmany I, Sever R, et al. Pancreaticoduodenectomy in elderly adults: is it justified in terms of mortality, long-term morbidity, and quality of life? J Am Geriatr Soc. 2013; 61:1351–1357.
Article8. Kim SY, Fink MA, Perini M, Houli N, Weinberg L, Muralidharan V, et al. Age 80 years and over is not associated with increased morbidity and mortality following pancreaticoduodenectomy. ANZ J Surg. 2018; 88:E445–E450.
Article9. Casadei R, Taffurelli G, Silvestri S, Ricci C, Campra D, Minni F. Is age a barrier to pancreaticoduodenectomy? An Italian dual-institution study. Updates Surg. 2015; 67:439–447.
Article10. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.11. Makary MA, Winter JM, Cameron JL, Campbell KA, Chang D, Cunningham SC, et al. Pancreaticoduodenectomy in the very elderly. J Gastrointest Surg. 2006; 10:347–356.
Article12. Lee MK, Dinorcia J, Reavey PL, Holden MM, Genkinger JM, Lee JA, et al. Pancreaticoduodenectomy can be performed safely in patients aged 80 years and older. J Gastrointest Surg. 2010; 14:1838–1846.
Article13. Wagner M, Redaelli C, Lietz M, Seiler CA, Friess H, Buchler MW. Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br J Surg. 2004; 91:586–594.
Article14. Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang DC, Coleman J, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg. 2006; 10:1199–1210.
Article15. DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007; 245:755–762.16. Jang JY, Kim SW, Park DJ, Ahn YJ, Yoon YS, Choi MG, et al. Actual long-term outcome of extrahepatic bile duct cancer after surgical resection. Ann Surg. 2005; 241:77–84.
Article17. Howe JR, Klimstra DS, Moccia RD, Conlon KC, Brennan MF. Factors predictive of survival in ampullary carcinoma. Ann Surg. 1998; 228:87–94.
Article18. Bakaeen FG, Murr MM, Sarr MG, Thompson GB, Farnell MB, Nagorney DM, et al. What prognostic factors are important in duodenal adenocarcinoma? Arch Surg. 2000; 135:635–641.
Article19. Sho M, Murakami Y, Kawai M, Motoi F, Satoi S, Matsumoto I, et al. Prognosis after surgical treatment for pancreatic cancer in patients aged 80 years or older: a multicenter study. J Hepatobiliary Pancreat Sci. 2016; 23:188–197.20. Aparicio T, Jouve JL, Teillet L, Gargot D, Subtil F, Le Brun-Ly V, et al. Geriatric factors predict chemotherapy feasibility: ancillary results of FFCD 2001-02 phase III study in first-line chemotherapy for metastatic colorectal cancer in elderly patients. J Clin Oncol. 2013; 31:1464–1470.
Article21. Kinoshita S, Sho M, Yanagimoto H, Satoi S, Akahori T, Nagai M, et al. Potential role of surgical resection for pancreatic cancer in the very elderly. Pancreatology. 2015; 15:240–246.
Article22. Langer CJ, Manola J, Bernardo P, Kugler JW, Bonomi P, Cella D, et al. Cisplatin-based therapy for elderly patients with advanced non-small-cell lung cancer: implications of Eastern Cooperative Oncology Group 5592, a randomized trial. J Natl Cancer Inst. 2002; 94:173–181.
Article23. Giordano SH, Duan Z, Kuo YF, Hortobagyi GN, Goodwin JS. Use and outcomes of adjuvant chemotherapy in older women with breast cancer. J Clin Oncol. 2006; 24:2750–2756.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perimpullary Carcinoma: A Study on Prognostic Factors Influencing long Term Survival After Pancreaticoduodenectomy
- Clinical analysis of the effect of pancreaticoduodenectomy in periampullary cancer
- Pancreaticoduodenectomy with superior mesenteric artery first-approach combined total meso-pancreas excision for periampullary malignancies: A high-volume single-center experience with short-term outcomes
- Survival Analysis according to the Treatment Modalities of the Periampullary Carcinoma
- One hundred sixty pancreaticoduodenectomies for periampullary cancers in a growing-volume setting: a single-institution and a single-surgeon's experience