Diabetes Metab J.
2019 Dec;43(6):776-784. 10.4093/dmj.2018.0189.
Impact of Continuous Care on Health Outcomes and Cost for Type 2 Diabetes Mellitus: Analysis Using National Health Insurance Cohort Database
- Affiliations
-
- 1Department of Preventive Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. eshin@catholic.ac.kr
- 2School of Public Health, The Catholic University of Korea, Seoul, Korea.
- 3Korea Institute of Child Care and Education, Seoul, Korea.
- 4National Evidence-based Healthcare Collaborating Agency, Seoul, Korea.
- 5Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 6Department of Family Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 7Department of Family Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2466499
- DOI: http://doi.org/10.4093/dmj.2018.0189
Abstract
- BACKGROUND
The objective of the study was to determine the impact of continuous care on health outcomes and cost of type 2 diabetes mellitus (T2DM) in Korea.
METHODS
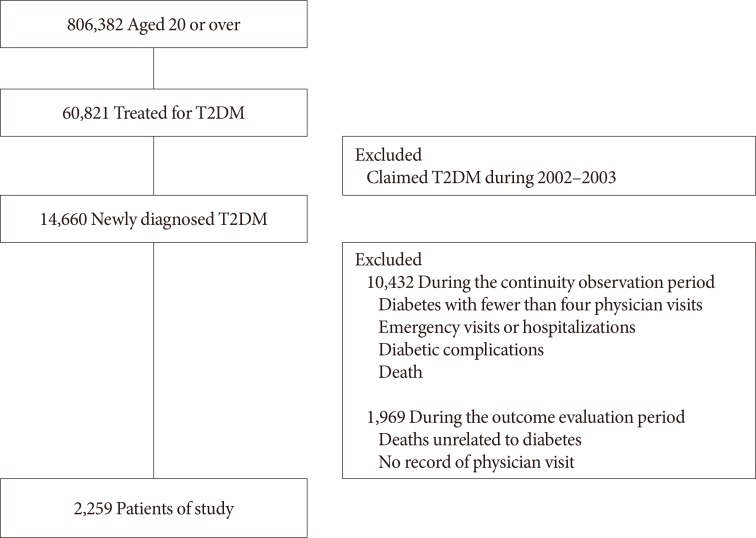
A nationwide retrospective, observational case-control study was conducted. Continuity of treatment was measured using Continuity of Care (COC) score. Information of all patients newly diagnosed with T2DM in 2004 was retrieved from the National Health Insurance database for the period of 2002 to 2013. The study examined 2,373 patients after applying exclusion criteria, such as for patients who died from conditions not related to T2DM. Statistical analyses were performed using frequency distribution, simple analysis (t-test and chi-squared test), and multi-method analysis (simple linear regression, logistic regression, and survival analysis).
RESULTS
The overall COC score was 0.8±0.24. The average incidence of diabetic complications was 0.39 per patient with a higher COC score, whereas it was 0.49 per patient with a lower COC score. In both survival and logistic analyses, patients who had high COC score were significantly less likely to have diabetic complications (hazard ratio, 0.69; 95% confidence interval, 0.54 to 0.88). The average medical cost was approximately 3,496 United States dollar (USD) per patient for patients with a higher COC score, whereas it was 3,973 USD per patient for patients with a lower COC score during the 2006 to 2013 period, with a difference of around 477 USD, which is statistically significant after adjusting for other factors (β=−0.152).
CONCLUSION
Continuity of care for diabetes significantly reduced health complications and medical costs from patients with T2DM.
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Study Using Healthcare Claims Database
Jin-Su Park, Chan Hee Lee
J Rheum Dis. 2021;28(3):119-125. doi: 10.4078/jrd.2021.28.3.119.
Reference
-
1. International Diabetes Federation. IDF diabetes atlas. 5th ed. Brussels: International Diabetes Federation;2011.2. International Diabetes Federation. IDF diabetes atlas. 4th ed. Brussels: International Diabetes Federation;2009.3. Ogurtsova K, da Rocha Fernandes JD, Huang Y, Linnenkamp U, Guariguata L, Cho NH, Cavan D, Shaw JE, Makaroff LE. IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017; 128:40–50. PMID: 28437734.
Article4. Hogan P, Dall T, Nikolov P. American Diabetes Association. Economic costs of diabetes in the US in 2002. Diabetes Care. 2003; 26:917–932. PMID: 12610059.5. Brandle M, Zhou H, Smith BR, Marriott D, Burke R, Tabaei BP, Brown MB, Herman WH. The direct medical cost of type 2 diabetes. Diabetes Care. 2003; 26:2300–2304. PMID: 12882852.
Article6. Clarke P, Gray A, Legood R, Briggs A, Holman R. The impact of diabetes-related complications on healthcare costs: results from the United Kingdom Prospective Diabetes Study (UKPDS Study No. 65). Diabet Med. 2003; 20:442–450. PMID: 12786677.
Article7. Williams R, Van Gaal L, Lucioni C. CODE-2 Advisory Board. Assessing the impact of complications on the costs of type II diabetes. Diabetologia. 2002; 45:S13–S17.
Article8. Zhuo X, Zhang P, Hoerger TJ. Lifetime direct medical costs of treating type 2 diabetes and diabetic complications. Am J Prev Med. 2013; 45:253–261. PMID: 23953350.
Article9. Centers for Disease Control and Prevention: National diabetes statistics report, 2014. cited 2019 Aug 30. Available from: https://www.cdc.gov/diabetes/pdfs/data/2014-report-estimates-of-diabetes-and-its-burden-in-the-united-states.pdf.10. Centers for Disease Control and Prevention: National diabetes statistics report, 2017. cited 2019 Aug 30. Available from: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf.11. Kim SA. The selection of the medical institutions by severity of disease [dissertation]. Seoul: Yonsei University;2011.12. Kim JY. The selection of the medical institutions by motivation of medical service utilization. J Digit Converg. 2015; 13:217–230.
Article13. Park EJ, Jeon JA, Kim DE, Song ES, Choi SJ, Shim BR. Healthcare service utilization among Korean patients with chronic disease: focusing on hypertension and type 2 diabetes mellitus. Sejong: Korea Institute for Health and Social Affairs;2016.14. Lin W, Huang IC, Wang SL, Yang MC, Yaung CL. Continuity of diabetes care is associated with avoidable hospitalizations: evidence from Taiwan’s National Health Insurance scheme. Int J Qual Health Care. 2010; 22:3–8. PMID: 20007170.
Article15. Worrall G, Knight J. Continuity of care is good for elderly people with diabetes: retrospective cohort study of mortality and hospitalization. Can Fam Physician. 2011; 57:e16–e20. PMID: 21252120.16. Hanafi NS, Abdullah A, Lee PY, Liew SM, Chia YC, Khoo EM. Personal continuity of care in a university-based primary care practice: impact on blood pressure control. PLoS One. 2015; 10:e0134030. PMID: 26214304.
Article17. Tsai HY, Chou YJ, Pu C. Continuity of care trajectories and emergency room use among patients with diabetes. Int J Public Health. 2015; 60:505–513. PMID: 25779687.
Article18. Chen CC, Chen SH. Better continuity of care reduces costs for diabetic patients. Am J Manag Care. 2011; 17:420–427. PMID: 21756012.19. Tom JO, Tseng CW, Davis J, Solomon C, Zhou C, Mangione-Smith R. Missed well-child care visits, low continuity of care, and risk of ambulatory care-sensitive hospitalizations in young children. Arch Pediatr Adolesc Med. 2010; 164:1052–1058. PMID: 21041598.
Article20. Litaker D, Ritter C, Ober S, Aron D. Continuity of care and cardiovascular risk factor management: does care by a single clinician add to informational continuity provided by electronic medical records? Am J Manag Care. 2005; 11:689–696. PMID: 16268752.21. Younge R, Jani B, Rosenthal D, Lin SX. Does continuity of care have an effect on diabetes quality measures in a teaching practice in an urban underserved community? J Health Care Poor Underserved. 2012; 23:1558–1565. PMID: 23698670.
Article22. Bice TW, Boxerman SB. A quantitative measure of continuity of care. Med Care. 1977; 15:347–349. PMID: 859364.
Article23. Shortell SM. Continuity of medical care: conceptualization and measurement. Med Care. 1976; 14:377–391. PMID: 1271879.24. Saultz JW. Defining and measuring interpersonal continuity of care. Ann Fam Med. 2003; 1:134–143. PMID: 15043374.
Article25. Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin Diabetes. 2008; 26:77–82.
Article26. Park CM, Jang SM, Jang SH, Lee HJ. Healthcare cost and outcome affected by continuity of care (hypertension and diabetes). Seoul: Health Insurance Review and Assessment Service;2011.27. Hodgson TA, Meiners MR. Cost-of-illness methodology: a guide to current practices and procedures. Milbank Mem Fund Q Health Soc. 1982; 60:429–462. PMID: 6923138.
Article28. Hong JS, Kim JY. Study on continuity of primary care for Korean elderly. Seoul: Health Insurance Review and Assessment Service;2007.29. Chen CC, Tseng CH, Cheng SH. Continuity of care, medication adherence, and health care outcomes among patients with newly diagnosed type 2 diabetes: a longitudinal analysis. Med Care. 2013; 51:231–237. PMID: 23269110.30. Cho KH, Lee SG, Jun B, Jung BY, Kim JH, Park EC. Effects of continuity of care on hospital admission in patients with type 2 diabetes: analysis of nationwide insurance data. BMC Health Serv Res. 2015; 15:107. PMID: 25879858.
Article31. Mainous AG 3rd, Koopman RJ, Gill JM, Baker R, Pearson WS. Relationship between continuity of care and diabetes control: evidence from the third National Health and Nutrition Examination Survey. Am J Public Health. 2004; 94:66–70. PMID: 14713700.
Article32. American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2003; 26:S33–S50. PMID: 12502618.33. Vijan S, Stevens DL, Herman WH, Funnell MM, Standiford CJ. Screening, prevention, counseling, and treatment for the complications of type II diabetes mellitus. Putting evidence into practice. J Gen Intern Med. 1997; 12:567–580. PMID: 9294791.34. Krolewski AS, Czyzyk A, Janeczko D, Kopczynski J. Mortality from cardiovascular diseases among diabetics. Diabetologia. 1977; 13:345–350. PMID: 913925.
Article35. Panzram G. Mortality and survival in type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia. 1987; 30:123–131. PMID: 3556287.
Article36. O'Malley AS, Mandelblatt J, Gold K, Cagney KA, Kerner J. Continuity of care and the use of breast and cervical cancer screening services in a multiethnic community. Arch Intern Med. 1997; 157:1462–1470. PMID: 9224225.37. Sweeney KG, Gray DP. Patients who do not receive continuity of care from their general practitioner: are they a vulnerable group? Br J Gen Pract. 1995; 45:133–135. PMID: 7772390.38. Parchman ML, Pugh JA, Noel PH, Larme AC. Continuity of care, self-management behaviors, and glucose control in patients with type 2 diabetes. Med Care. 2002; 40:137–144. PMID: 11802086.
Article39. Raddish M, Horn SD, Sharkey PD. Continuity of care: is it cost effective. Am J Manag Care. 1999; 5:727–734. PMID: 10538452.40. Weiss LJ, Blustein J. Faithful patients: the effect of long-term physician-patient relationships on the costs and use of health care by older Americans. Am J Public Health. 1996; 86:1742–1747. PMID: 9003131.
Article41. Kim J, Kim H, Kim H, Min KW, Park SW, Park IB, Park JH, Baik SH, Son HS, Ahn CW, Oh JY, Lee S, Lee J, Chung CH, Choi KM, Choi I, Kim DJ. Current status of the continuity of ambulatory diabetes care and its impact on health outcomes and medical cost in Korea using National Health Insurance Database. J Korean Diabetes Assoc. 2006; 30:377–387.
Article42. Kim YM, Chang DM, Kim SS, Park IS, Kang SH. A study on factors of management of diabetes mellitus using data mining. J Korea Acad Ind Coop Soc. 2009; 10:1100–1108.
Article43. Ji EJ. Factors associated with hemoglobin a1c among patient aged 40 years over with diabetes mellitus: 2012 Korea Health and Nutrition Examination Survey. J Korean Acad Fundam Nurs. 2015; 22:433–441.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Continuity of Care for Elderly Patients with Diabetes Mellitus, Hypertension, Asthma, and Chronic Obstructive Pulmonary Disease in Korea
- Epidemiologic Characteristics of Diabetes Mellitus in Korea: Current Status of Diabetic Patients Using Korean Health Insurance Database
- Introducing big data analysis using data from National Health Insurance Service
- The Benefits Of Continuous Glucose Monitoring In Pregnancy
- A Study of Total Medical Cost and Hospitalization Risk of Patients with Schizophrenia and Type 1 Diabetes Mellitus