Yonsei Med J.
2020 Jan;61(1):30-39. 10.3349/ymj.2020.61.1.30.
Immediate and Evolutionary Recovery of Left Ventricular Diastolic Function after Transcatheter Aortic Valve Replacement: Comparison with Surgery
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 2Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. GRHONG@yuhs.ac
- KMID: 2466333
- DOI: http://doi.org/10.3349/ymj.2020.61.1.30
Abstract
- PURPOSE
We aimed to compare the effect of transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (sAVR) on recovery of left ventricular (LV) diastolic function and afterload through serial echocardiographic examinations in patients with symptomatic high-risk severe aortic stenosis during early follow-up.
MATERIALS AND METHODS
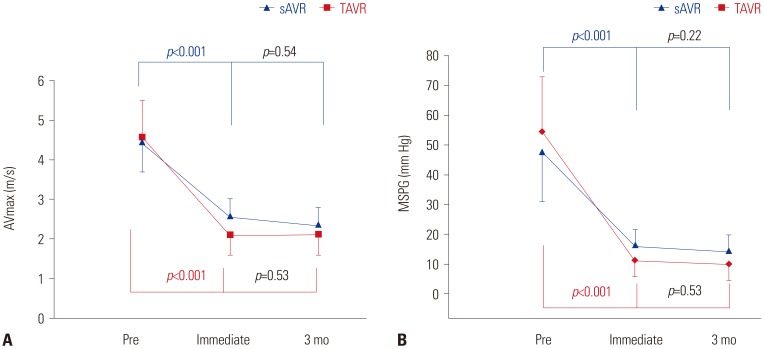
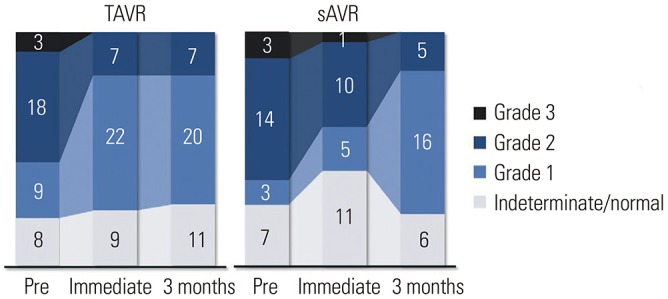
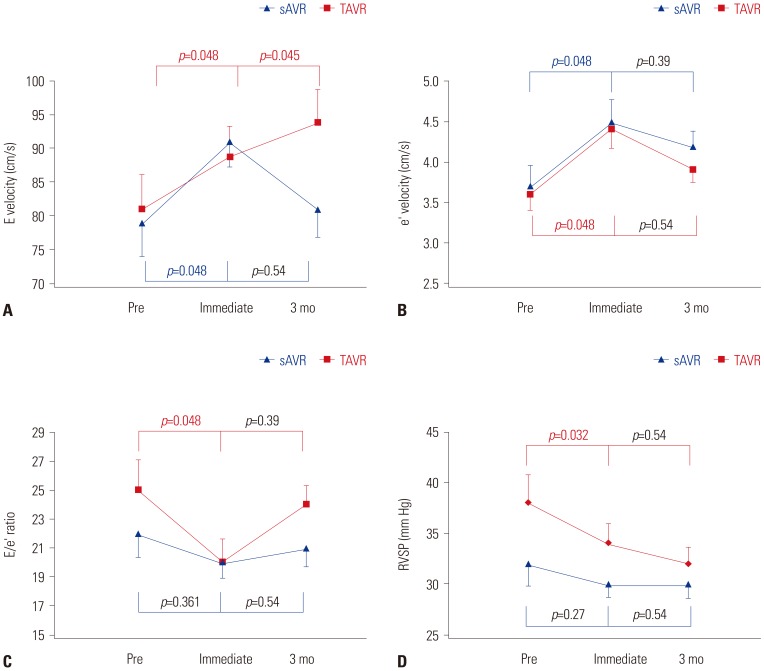
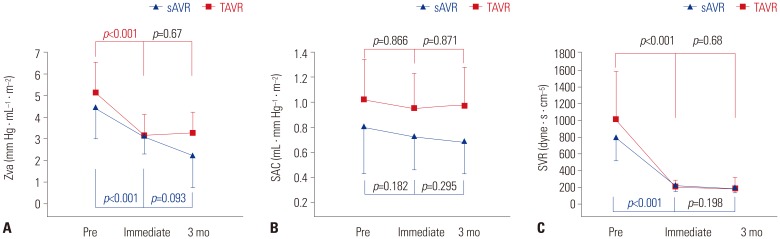
We included 38 patients undergoing TAVR (mean age, 80±6 years; male:female=18:20) and 27 patients undergoing sAVR (mean age, 78±3 years; male:female=12:15). We compared changes in the LV diastolic function and afterload before, immediately after, and 3 months after the procedure using serial transthoracic echocardiography.
RESULTS
Immediately after the procedure, 16 (42%) and 3 (11%) patients in the TAVR and sAVR groups, respectively, showed rapid improvement in diastolic filling patterns. E wave to e"² ratio (E/e"²) and right ventricular systolic pressure (RVSP) decreased significantly in the TAVR group (E/e"²: TAVR, from 24.6±12.9 to 20±9.5, p=0.048 vs. sAVR, from 21.5±9.4 to 20.64±6.4, p=0.361; RVSP: TAVR, 38.4±17.2 vs. 34±12.4, p=0.032 vs. sAVR, 32.2±11.7 vs. 30±6.8, p=0.27). After 3 months, diastolic grade distribution, E/e"², and RVSP were similar. Valvuloarterial impedance significantly decreased immediately after the procedure in both groups (TAVR, from 5.1±1.4 to 3.1±1.0 vs. sAVR, from 4.5±1.5 to 3.1±0.8 mm Hg · mL⻹· m⻲, p=0.001), but after 3 months, decreases were greater in the sAVR group (from 3.1±0.8 to 2.2±1.5 mm Hg · mL⻹· m⻲, p=0.093).
CONCLUSION
LV diastolic function improved more rapidly and earlier in patients treatment with TAVR than in patients treated with sAVR. These results might explicate the remarkable clinical improvement in improvements in advanced diastolic dysfunction immediately after the TAVR procedure than sAVR.
MeSH Terms
Figure
Reference
-
1. Bax JJ, Delgado V, Bapat V, Baumgartner H, Collet JP, Erbel R, et al. Open issues in transcatheter aortic valve implantation. Part 1: patient selection and treatment strategy for transcatheter aortic valve implantation. Eur Heart J. 2014; 35:2627–2638. PMID: 25062952.
Article2. Gonçalves A, Marcos-Alberca P, Almeria C, Feltes G, Rodríguez E, Hernández-Antolín RA, et al. Acute left ventricle diastolic function improvement after transcatheter aortic valve implantation. Eur J Echocardiogr. 2011; 12:790–797. PMID: 21865229.3. Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010; 363:1597–1607. PMID: 20961243.
Article4. Kodali SK, Williams MR, Smith CR, Svensson LG, Webb JG, Makkar RR, et al. Two-year outcomes after transcatheter or surgical aorticvalve replacement. N Engl J Med. 2012; 366:1686–1695. PMID: 22443479.
Article5. Kapadia SR, Tuzcu EM, Makkar RR, Svensson LG, Agarwal S, Kodali S, et al. Long-term outcomes of inoperable patients with aortic stenosis randomly assigned to transcatheter aortic valve replacement or standard therapy. Circulation. 2014; 130:1483–1492. PMID: 25205802.
Article6. Gotzmann M, Lindstaedt M, Bojara W, Mügge A, Germing A. Hemodynamic results and changes in myocardial function after transcatheter aortic valve implantation. Am Heart J. 2010; 159:926–932. PMID: 20435207.
Article7. Spethmann S, Dreger H, Baldenhofer G, Stüer K, Saghabalyan D, Müller E, et al. Short-term effects of transcatheter aortic valve implantation on left atrial mechanics and left ventricular diastolic function. J Am Soc Echocardiogr. 2013; 26:64–71. PMID: 23140843.
Article8. Vizzardi E, D'Aloia A, Fiorina C, Bugatti S, Parrinello G, De Carlo M, et al. Early regression of left ventricular mass associated with diastolic improvement after transcatheter aortic valve implantation. J Am Soc Echocardiogr. 2012; 25:1091–1098. PMID: 22819229.
Article9. Bonow RO, Carabello BA, Chatterjee K, de Leon AC Jr, Faxon DP, Freed MD, et al. 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2008; 118:e523–e661. PMID: 18820172.
Article10. Hahn RT, Abraham T, Adams MS, Bruce CJ, Glas KE, Lang RM, et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013; 26:921–964. PMID: 23998692.
Article11. Zoghbi WA, Chambers JB, Dumesnil JG, Foster E, Gottdiener JS, Grayburn PA, et al. Recommendations for evaluation of prosthetic valves with echocardiography and doppler ultrasound: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Task Force on Prosthetic Valves, developed in conjunction with the American College of Cardiology Cardiovascular Imaging Committee, Cardiac Imaging Committee of the American Heart Association, the European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography and the Canadian Society of Echocardiography, endorsed by the American College of Cardiology Foundation, American Heart Association, European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography, and Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2009; 22:975–1014. PMID: 19733789.12. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39. PMID: 25559473.
Article13. Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. Eur J Echocardiogr. 2009; 10:1–25. PMID: 19065003.
Article14. Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003; 16:777–802. PMID: 12835667.
Article15. Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016; 29:277–314. PMID: 27037982.
Article16. Stefanadis C, Stratos C, Boudoulas H, Kourouklis C, Toutouzas P. Distensibility of the ascending aorta: comparison of invasive and non-invasive techniques in healthy men and in men with coronary artery disease. Eur Heart J. 1990; 11:990–996. PMID: 2282929.
Article17. Chemla D, Hébert JL, Coirault C, Zamani K, Suard I, Colin P, et al. Total arterial compliance estimated by stroke volume-to-aortic pulse pressure ratio in humans. Am J Physiol. 1998; 274:H500–H505. PMID: 9486253.
Article18. Briand M, Dumesnil JG, Kadem L, Tongue AG, Rieu R, Garcia D, et al. Reduced systemic arterial compliance impacts significantly on left ventricular afterload and function in aortic stenosis: implications for diagnosis and treatment. J Am Coll Cardiol. 2005; 46:291–298. PMID: 16022957.19. Ikonomidis I, Tsoukas A, Parthenakis F, Gournizakis A, Kassimatis A, Rallidis L, et al. Four year follow up of aortic valve replacement for isolated aortic stenosis: a link between reduction in pressure overload, regression of left ventricular hypertrophy, and diastolic function. Heart. 2001; 86:309–316. PMID: 11514485.
Article20. Orsinelli DA, Aurigemma GP, Battista S, Krendel S, Gaasch WH. Left ventricular hypertrophy and mortality after aortic valve replacement for aortic stenosis. A high risk subgroup identified by preoperative relative wall thickness. J Am Coll Cardiol. 1993; 22:1679–1683. PMID: 8227838.21. Douglas PS, Berko B, Lesh M, Reichek N. Alterations in diastolic function in response to progressive left ventricular hypertrophy. J Am Coll Cardiol. 1989; 13:461–467. PMID: 2521506.
Article22. Guarracino F, Talini E, Landoni G, Petronio S, Giannini C, Di Bello V. Effect of aortic valve surgery on left ventricular diastole assessed by echocardiography and neuroendocrine response: percutaneous versus surgical approach. J Cardiothorac Vasc Anesth. 2010; 24:25–29. PMID: 19944626.
Article23. Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009; 22:107–133. PMID: 19187853.
Article24. Villari B, Vassalli G, Monrad ES, Chiariello M, Turina M, Hess OM. Normalization of diastolic dysfunction in aortic stenosis late after valve replacement. Circulation. 1995; 91:2353–2358. PMID: 7729021.
Article25. Kempny A, Diller GP, Kaleschke G, Orwat S, Funke A, Schmidt R, et al. Impact of transcatheter aortic valve implantation or surgical aortic valve replacement on right ventricular function. Heart. 2012; 98:1299–1304. PMID: 22689711.
Article26. Covello RD, Maj G, Landoni G, Maisano F, Michev I, Guarracino F, et al. Anesthetic management of percutaneous aortic valve implantation: focus on challenges encountered and proposed solutions. J Cardiothorac Vasc Anesth. 2009; 23:280–285. PMID: 19231242.
Article27. Lund O, Erlandsen M. Changes in left ventricular function and mass during serial investigations after valve replacement for aortic stenosis. J Heart Valve Dis. 2000; 9:583–593. PMID: 10947054.28. Fairbairn TA, Steadman CD, Mather AN, Motwani M, Blackman DJ, Plein S, et al. Assessment of valve haemodynamics, reverse ventricular remodelling and myocardial fibrosis following transcatheter aortic valve implantation compared to surgical aortic valve replacement: a cardiovascular magnetic resonance study. Heart. 2013; 99:1185–1191. PMID: 23749779.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expanding transcatheter aortic valve replacement into uncharted indications
- Comparison of Postoperative LV Function after Mitral Valve Replacement and Predictor of Postoperative LV Function in Chronic Mitral Regurgitation
- Aortic Valve Replacement with Pulmonary Autograft in Patient with Congenital Aortic Stenosis : Ross Procedure without Homograft: one case report
- Regression of Left Ventricular Mass after Aortic Valve Replacement in Isolated Aortic Regurgitation
- Successful Transcatheter Aortic Valve Replacement for Severe Aortic Regurgitation after CARVAR Operation