J Endocr Surg.
2019 Dec;19(4):151-153. 10.16956/jes.2019.19.4.151.
Venous Thromboembolism Following Thyroid Surgery
- Affiliations
-
- 1Division of Endocrine Surgery, Department of General Surgery, Ege University Hospital, Izmir, Turkey. ozer.makay@ege.edu.tr
- 2Division of Thyroid Surgery, Jilin Provincial Key Laboratory of Surgical Translational Medicine, China Japan Union Hospital of Jilin University, Changchun, China.
- 3Division for Endocrine and Minimally Invasive Surgery, Department of Human Pathology in Adulthood and Childhood “G. Barresiâ€, University Hospital G. Martino, University of Messina, Messina, Italy.
- 4Department of Human Pathology in Adulthood and Childhood “G. Barresiâ€, University Hospital G. Martino, University of Messina, Messina, Italy.
- KMID: 2466241
- DOI: http://doi.org/10.16956/jes.2019.19.4.151
Abstract
- Venous thromboembolism is viewed as a serious health care issue. Patients who experience venous thromboembolism often have an detoriorated quality of life after the event that may require anticoagulation. This results to the risks of spontaneous bleeding. Bleeding after thyroid surgery can present acutely and can lead to airway compromise and death if not recognized and treated appropriately. Whether prophylaxis in a low-risk patient puts the patient at a greater risk of developing a bleeding complication is not well documented. The literature is scarce regarding the prevalence of venous thromboembolism following thyroid and parathyroid surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Macht R, Gardner I, Talutis S, Rosenkranz P, Doherty G, McAneny D. Evaluation of a standardized risk-based venous thromboembolism prophylaxis protocol in the setting of thyroid and parathyroid surgery. J Am Coll Surg. 2017; 224:1029–1035.
Article2. Dralle H. Risk-based thromboembolism prophylaxis in thyroid surgeries. Chirurg. 2017; 88:973.3. Bahl V, Shuman AG, Hu HM, Jackson CR, Pannucci CJ, Alaniz C, et al. Chemoprophylaxis for venous thromboembolism in otolaryngology. JAMA Otolaryngol Head Neck Surg. 2014; 140:999–1005.
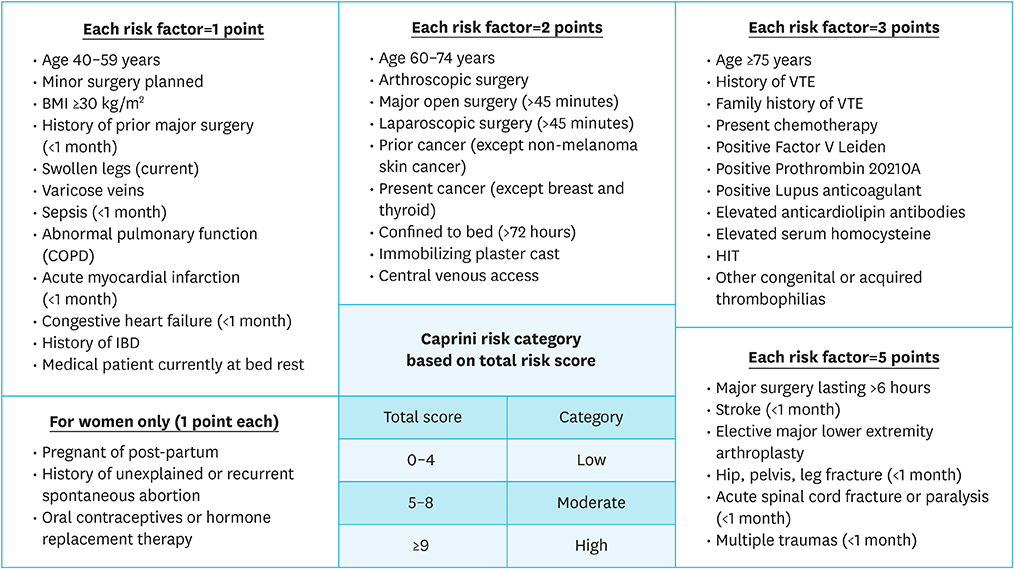
Article4. Pannucci CJ, Swistun L, MacDonald JK, Henke PK, Brooke BS. Individualized venous thromboembolism risk stratification using the 2005 Caprini score to identify the benefits and harms of chemoprophylaxis in surgical patients: a meta-analysis. Ann Surg. 2017; 265:1094–1103.
Article5. Hachey KJ, Sterbling H, Choi DS, Pinjic E, Hewes PD, Munoz J, et al. Prevention of postoperative venous thromboembolism in thoracic surgical patients: implementation and evaluation of a Caprini risk assessment protocol. J Am Coll Surg. 2016; 222:1019–1027.
Article6. Cassidy MR, Macht RD, Rosenkranz P, Caprini JA, McAneny D. Patterns of failure of a standardized perioperative venous thromboembolism prophylaxis protocol. J Am Coll Surg. 2016; 222:1074–1080.
Article7. Mowery A, Light T, Clayburgh D. Venous thromboembolism incidence in head and neck surgery patients: analysis of the Veterans Affairs Surgical Quality Improvement Program (VASQIP) database. Oral Oncol. 2018; 77:22–28.
Article8. Horacek J, Maly J, Svilias I, Smolej L, Cepkova J, Vizda J, et al. Prothrombotic changes due to an increase in thyroid hormone levels. Eur J Endocrinol. 2015; 172:537–542.
Article