J Korean Foot Ankle Soc.
2019 Dec;23(4):208-211. 10.14193/jkfas.2019.23.4.208.
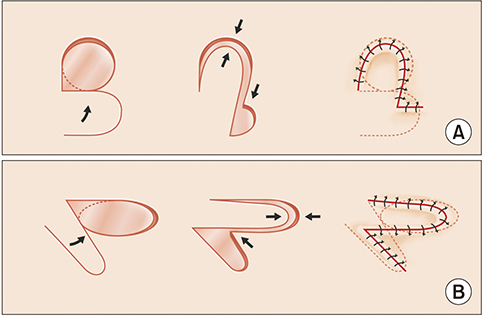
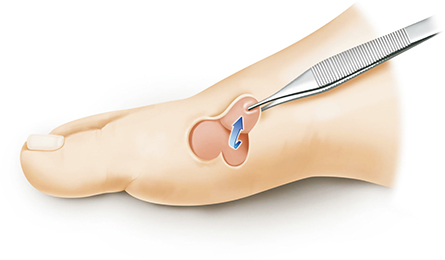
Treatment Using a Single-Lobed Rotation Flap in Diabetic Forefoot Ulceration: Five Case Reports
- Affiliations
-
- 1Department of Orthopedic Surgery, Daejeon Sun Hospital, Daejeon, Korea. kjb9290@hanmail.net
- KMID: 2465946
- DOI: http://doi.org/10.14193/jkfas.2019.23.4.208
Abstract
- Diabetic foot ulcers can progress to the point where amputation is needed, and so these ulcers require active treatment. Skin grafts or flaps can be performed for coverage of this type of ulcer. Local flap surgery is relatively easy to perform and good results have been previously reported. We performed single-lobed rotation flap on 5 cases of forefoot ulcer around the site of weight bearing. The location of the foot ulcers was the medial part of the first metatarsophalangeal joint in all the patients. The mean size of the defect was 4.70 cm2. Managing of ulcers, controlling of diabetes and infection, and improving of peripheral blood flow were performed before surgery. In two cases, infection progressed to the articular cartilage and so metatarsophalangeal joint fusions were performed simultaneously. All the cases were completely transplanted. There was no recurrence of the ulcers, and all the patients were able to walk.
Keyword
MeSH Terms
Figure
Reference
-
1. Seo DK, Lee HS. Management of diabetic foot ulcer. J Korean Foot Ankle Soc. 2014; 18:1–7. DOI: 10.14193/jkfas.2014.18.1.1.
Article2. Kwon DJ, Lee YB, Ahn HC. Use of acellular allograft dermal matrix (Alloderm®) and split-thickness skin graft for treatment of diabetic foot ulcer. J Korean Musculoskelet Transplant Soc. 2007; 7:86–91.3. Wagner FW. A classification and treatment program for diabetics, neuropathic and dysvascular foot problems. Instr Course Lect. 1979; 28:143–165.4. Schrudde J, Petrovici V. The use of slide-swing plasty in closing skin defects: a clinical study based on 1,308 cases. Plast Reconstr Surg. 1981; 67:467–481. DOI: 10.1097/00006534-198104000-00008.5. Kim JM, Kim DY, Woo JT, Kim SW, Yang IM, Kim JW, et al. A clinical study on the diabetic foot lesions. J Korean Diabetes Assoc. 1993; 17:387–394.6. Song JY, Kim KS, Ko SH, Choi YS, Chung YR, Kim HD, et al. Reconstruction of diabetic foot ulcers by regional flap surgery. J Korean Orthop Assoc. 2003; 38:301–304. DOI: 10.4055/jkoa.2003.38.3.301.
Article7. Kadukammakal J, Yau S, Urbas W. Assessment of partial first-ray resections and their tendency to progress to transmetatarsal amputations: a retrospective study. J Am Podiatr Med Assoc. 2012; 102:412–416. DOI: 10.7547/1020412.
Article8. Steed DL, Donohoe D, Webster MW, Lindsley L. Effect of extensive debridement and treatment on the healing of diabetic foot ulcers Diabetic Ulcer Study Group. J Am Coll Surg. 1996; 183:61–64.9. Randon C, Vermassen F, Jacobs B, De Ryck F, Van Landuyt K, Taes Y. Outcome of arterial reconstruction and free-flap coverage in diabetic foot ulcers: long-term results. World J Surg. 2010; 34:177–184. DOI: 10.1007/s00268-009-0250-9.
Article10. Laing PW, Cogley DI, Klenerman L. Neuropathic foot ulceration treated by total contact casts. J Bone Joint Surg Br. 1992; 74:133–136. DOI: 10.1302/0301-620X.74B1.1732242.
Article11. Nam SC, Han SH, Lim SH, Hong YS, Won JH, Bae JI, et al. Factors affecting the validity of ankle-brachial index in the diagnosis of peripheral arterial obstructive disease. Angiology. 2010; 61:392–396. DOI: 10.1177/0003319709348295.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fillet Flap Coverage for Closure of Diabetic Foot Amputation
- Heel Pad Reconstruction using Doresalis Pedis Free Flap or Rotation Flap
- Operative Treatment for Neuropathic Diabetic Foot Ulcer: Usefulness of V-Y Advancement Flap for Unhealing Plantar Ulcer
- Rotation Fasciocutaneous Flap with Z - Plasty: Clinical Applications for Reconstruction of the Lower Leg
- Reconstruction of Forefoot Degloving Injury with Innervated Anterolateral Thigh Free Flap