J Korean Foot Ankle Soc.
2019 Dec;23(4):183-188. 10.14193/jkfas.2019.23.4.183.
Improvement of Pain according to Magnetic Resonance Imaging Classification in Bone Contusion around Foot and Ankle
- Affiliations
-
- 1Department of Orthopedic Surgery, Chonbuk National University Medical School, Jeonju, Korea. osdr2815@naver.com
- 2Department of Orthopedic Surgery, Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute, Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2465942
- DOI: http://doi.org/10.14193/jkfas.2019.23.4.183
Abstract
- PURPOSE
Bone contusion is usually treated with conservative therapy for 3 months. Bone contusion around knee and hip joints has been extensively reported on, but there are scant reports on this condition in foot and ankle joints. This study evaluated the nature, characteristics and location of bone contusion around foot and ankle joints to enlighten clinicians on how to better treat this disease entity.
MATERIALS AND METHODS
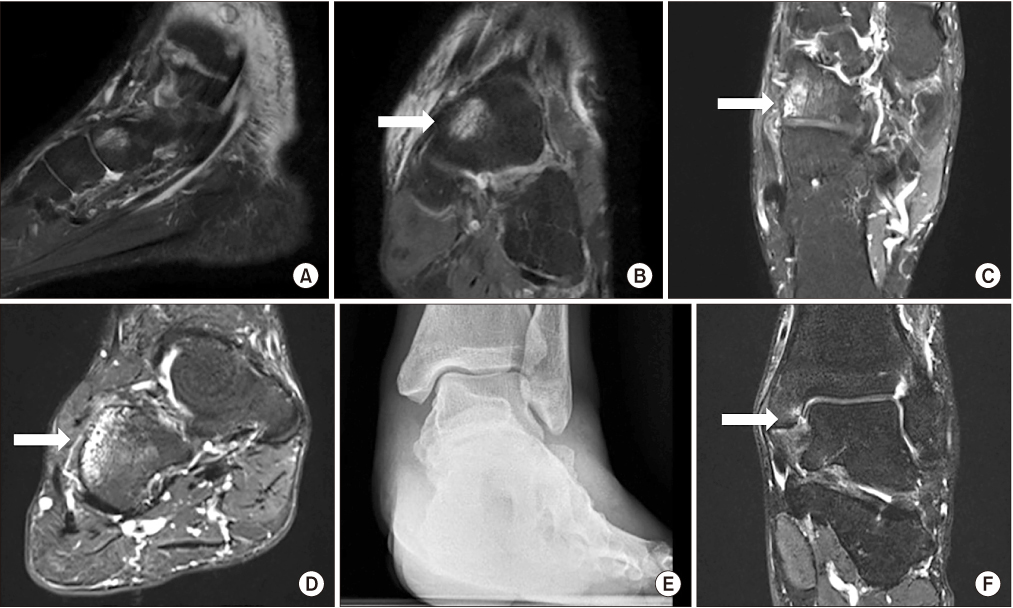
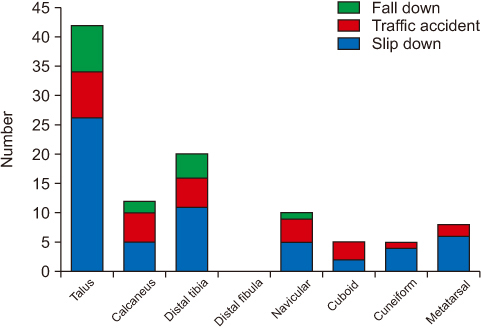
We classified bone contusion of the 76 patients into three types (102 sites; 47 ankle sprains, 18 traffic accidents, 11 falls) according to the Costa-Paz system with employing magnetic resonance imaging (MRI), and the study then analyzed the common sites and areas of occurrence according to the mechanism of injury and duration of pain after first conducting conservative therapy.
RESULTS
Of the 76 patients (102 sites) on the MRI, 43 case (42.2%) for talus, 19 cases for distal tibia, and 12 cases for calcaneus were involved. The classification, according to the Costa-Paz system, was Type I, 51 cases; Type II, 32 cases; and Type III, 19 cases. The duration of pain after conservative treatment was 12.15±2.17 weeks for Type I, 14.5±2.15 weeks for Type II, and 21.0±3.8 weeks for Type III.
CONCLUSION
The most common location of post-traumatic bone contusion around both the foot and ankle is the talus, distal tibia, and calcaneus. The most common type of injury noted on MRI is a diffuse signal with change of the medullary component (Type I), In cases of bone contusion extending to a subjacent articular surface or disruption or depression of the normal contour of the cortical surface (Types II, III), the patients' pain appears to last longer. Thus, it is necessary to consider a longer period of conservative treatment in cases of Types II and III bone contusion because the patients' pain may last longer than 3 months.
MeSH Terms
Figure
Reference
-
1. Kessler R, Campbell S, Wong D, Bui-Mansfield L. Magnetic resonance imaging of bone marrow: a review-part II. J Am Osteopath Coll Radiol. 2012; 1:13–24.2. Kaplan PA, Gehl RH, Dussault RG, Anderson MW, Diduch DR. Bone contusions of the posterior lip of the medial tibial plateau (contrecoup injury) and associated internal derangements of the knee at MR imaging. Radiology. 1999; 211:747–753. DOI: 10.1148/radiology.211.3.r99jn30747.
Article3. Bloem JL. Transient osteoporosis of the hip: MR imaging. Radiology. 1988; 167:753–755. DOI: 10.1148/radiology.167.3.3363135.
Article4. Vande Berg BC, Malghem JJ, Lecouvet FE, Jamart J, Maldague BE. Idiopathic bone marrow edema lesions of the femoral head: predictive value of MR imaging findings. Radiology. 1999; 212:527–535. DOI: 10.1148/radiology.212.2.r99au03527.
Article5. Costa-Paz M, Muscolo DL, Ayerza M, Makino A, Aponte-Tinao L. Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy. 2001; 17:445–449. DOI: 10.1053/jars.2001.23581.
Article6. Fernandez-Canton G, Casado O, Capelastegui A, Astigarraga E, Larena JA, Merino A. Bone marrow edema syndrome of the foot: one year follow-up with MR imaging. Skeletal Radiol. 2003; 32:273–278. DOI: 10.1007/s00256-003-0622-4.
Article7. Hofmann S. The painful bone marrow edema syndrome of the hip joint. Wien Klin Wochenschr. 2005; 117:111–120. DOI: 10.1007/s00508-005-0322-2.
Article8. Korompilias AV, Karantanas AH, Lykissas MG, Beris AE. Bone marrow edema syndrome. Skeletal Radiol. 2009; 38:425–436. DOI: 10.1007/s00256-008-0529-1.
Article9. Terzidis IP, Christodoulou AG, Ploumis AL, Metsovitis SR, Koimtzis M, Givissis P. The appearance of kissing contusion in the acutely injured knee in the athletes. Br J Sports Med. 2004; 38:592–596. DOI: 10.1136/bjsm.2003.006718.
Article10. Sahoo K, Garg A, Saha P, Dodia JV, Raj VR, Bhairagond SJ. Study of imaging pattern in bone marrow oedema in MRI in recent knee injuries and its correlation with type of knee injury. J Clin Diagn Res. 2016; 10:TC06–TC11. DOI: 10.7860/JCDR/2016/18843.7704.
Article11. Pinar H, Akseki D, Kovanlikaya I, Araç S, Bozkurt M. Bone bruises detected by magnetic resonance imaging following lateral ankle sprains. Knee Surg Sports Traumatol Arthrosc. 1997; 5:113–117. DOI: 10.1007/s001670050036.
Article12. Alanen V, Taimela S, Kinnunen J, Koskinen SK, Karaharju E. Incidence and clinical significance of bone bruises after supination injury of the ankle. A double-blind, prospective study. J Bone Joint Surg Br. 1998; 80:513–515. DOI: 10.1302/0301-620x.80b3.8404.13. Singh D, Ferrero A, Rose B, Goldberg A, Cullen N. Bone marrow edema syndrome of the foot and ankle: mid- to long-term follow-up in 18 patients. Foot Ankle Spec. 2016; 9:218–226. DOI: 10.1177/1938640015609986.14. Hagga JR, Gilkeson RC, Lanzieri CF. CT and MR imaging of the whole body. 5th ed. St. Louis (MO): Mosby;2009. p. 2152.15. Boks SS, Vroegindeweij D, Koes BW, Bernsen RM, Hunink MG, Bierma-Zeinstra SM. MRI follow-up of posttraumatic bone bruises of the knee in general practice. AJR Am J Roentgenol. 2007; 189:556–562. DOI: 10.2214/AJR.07.2276.
Article16. Dienst M, Blauth M. Bone bruise of the calcaneus. A case report. Clin Orthop Relat Res. 2000; (378):202–205. DOI: 10.1097/00003086-200009000-00030.17. Wright RW, Phaneuf MA, Limbird TJ, Spindler KP. Clinical outcome of isolated subcortical trabecular fractures (bone bruise) detected on magnetic resonance imaging in knees. Am J Sports Med. 2000; 28:663–667. DOI: 10.1177/03635465000280050701.
Article18. Mandalia V, Henson JH. Traumatic bone bruising--a review article. Eur J Radiol. 2008; 67:54–61. DOI: 10.1016/j.ejrad.2008.01.060.
Article19. Nishimura G, Yamato M, Togawa M. Trabecular trauma of the talus and medial malleolus concurrent with lateral collateral ligamentous injuries of the ankle: evaluation with MR imaging. Skeletal Radiol. 1996; 25:49–54. DOI: 10.1007/s002560050031.
Article20. Taga I, Shino K, Inoue M, Nakata K, Maeda A. Articular cartilage lesions in ankles with lateral ligament injury. An arthroscopic study. Am J Sports Med. 1993; 21:120–126. discussion 126–7. DOI: 10.1177/036354659302100120.
Article21. Lynch TC, Crues JV 3rd, Morgan FW, Sheehan WE, Harter LP, Ryu R. Bone abnormalities of the knee: prevalence and significance at MR imaging. Radiology. 1989; 171:761–766. DOI: 10.1148/radiology.171.3.2717748.
Article22. Graf BK, Cook DA, De Smet AA, Keene JS. "Bone bruises" on magnetic resonance imaging evaluation of anterior cruciate ligament injuries. Am J Sports Med. 1993; 21:220–223. DOI: 10.1177/036354659302100210.
Article23. Bartl C, Imhoff A, Bartl R. Treatment of bone marrow edema syndrome with intravenous ibandronate. Arch Orthop Trauma Surg. 2012; 132:1781–1788. DOI: 10.1007/s00402-012-1617-1.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of Ultrasonography for Foot and Ankle Sports Injuries
- Recurred Macrodystrophia Lipomatosa of the Foot: A Case Report
- Bone SPECT/CT of the Foot and Ankle: Potential Clinical Application for Chronic Foot Pain
- Are Magnetic Resonance Imaging Findings of Ankle Instability Always Correlated with Operative and Physical Examination Findings?
- Incidence of Tarsal Coalition: An Institutional Magnetic Resonance Imaging Analysis