J Korean Foot Ankle Soc.
2019 Dec;23(4):173-182. 10.14193/jkfas.2019.23.4.173.
Anterior Talofibular Ligament and Superior Extensor Ankle Retinaculum Thicknesses: Relationship with Balance
- Affiliations
-
- 1Department of Physical Therapy, Waldron College of Health and Human Services, Radford University, Radford, VA, United States. aaron@radford.edu
- 2Department of Physical Therapy, Rueckert-Hartman College for Health Professions, Regis University, Denver, CO, United States.
- KMID: 2465941
- DOI: http://doi.org/10.14193/jkfas.2019.23.4.173
Abstract
- PURPOSE
This study determined if anterior talofibular ligament (ATFL)/superior extensor ankle retinaculum (SEAR) thicknesses are related to dynamic balance in individuals with chronic ankle instability (CAI).
MATERIALS AND METHODS
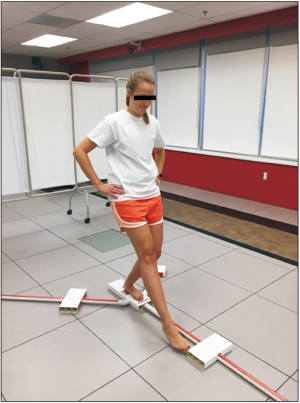
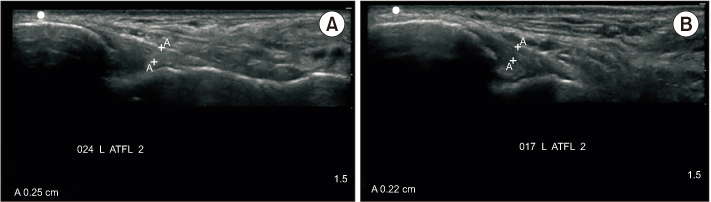
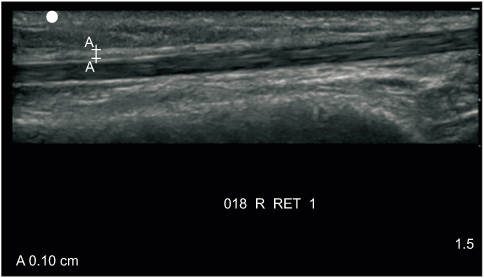
The subjects were 14 males and 15 females (age=24.52±3.46 years). Ankle instability was assessed using the Cumberland Ankle Instability Tool (CAIT) with a cut off score of 25 to define two groups. SonoSite MTurbo (Fugifilm Sonosite, Inc.) musculoskeletal ultrasound (MSKUS) unit was used to assess ATFL and SEAR thicknesses. Dynamic balance was measured with the Y Balance Test (YBT) and two NeuroCom balance tests.
RESULTS
There were no significant differences in the average ATFL thickness between stable and unstable ankles in those subjects with CAI (0.25±0.03 cm and 0.21±0.05 cm, respectively) or in the SEAR thickness (0.09±0.04 cm and 0.10±0.03 cm, respectively). There were also no significant differences in the right and left ATFL thicknesses (0.23±0.07 cm and 0.21±0.04 cm, respectively) or the SEAR thicknesses (0.09±0.01 cm and 0.09±0.01 cm, respectively) in those without CAI. There were no differences between limbs in composite scores on YBT in those with CAI (p=0.35) and those without CAI (p=0.33). There was a moderate correlation between the left SEAR thickness and the large forward/backward perturbations on the NeuroCom (Natus) motor control test (r=0.51, p=0.006 and r=0.54, p=0.003, respectively).
CONCLUSION
There were no differences in the ATFL/SEAR thicknesses or balance measures between or within the groups, likely because CAI is multi-factorial and related to mechanisms other than tissue changes alone. More sensitive technology and a better definition of the measurement process may provide more definitive results.
MeSH Terms
Figure
Reference
-
1. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010; 92:2279–2284. DOI: 10.2106/JBJS.I.01537.
Article2. Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland ankle instability tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006; 87:1235–1241. DOI: 10.1016/j.apmr.2006.05.022.
Article3. Wright CJ, Arnold BL, Ross SE, Linens SW. Recalibration and validation of the Cumberland Ankle Instability Tool cutoff score for individuals with chronic ankle instability. Arch Phys Med Rehabil. 2014; 95:1853–1859. DOI: 10.1016/j.apmr.2014.04.017.
Article4. Madsen LP, Hall EA, Docherty CL. Assessing outcomes in people with chronic ankle instability: the ability of functional performance tests to measure deficits in physical function and perceived instability. J Orthop Sports Phys Ther. 2018; 48:372–380. DOI: 10.2519/jospt.2018.7514.
Article5. Arnold BL, Linens SW, de la Motte SJ, Ross SE. Concentric evertor strength differences and functional ankle instability: a meta-analysis. J Athl Train. 2009; 44:653–662. DOI: 10.4085/1062-6050-44.6.653.
Article6. Maurer C, Mergner T, Bolha B, Hlavacka F. Vestibular, visual, and somatosensory contributions to human control of upright stance. Neurosci Lett. 2000; 281:99–102. DOI: 10.1016/s0304-3940(00)00814-4.
Article7. Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport. 2010; 13:2–12. DOI: 10.1016/j.jsams.2009.03.004.
Article8. Akbari M, Karimi H, Farahini H, Faghihzadeh S. Balance problems after unilateral lateral ankle sprains. J Rehabil Res Dev. 2006; 43:819–824.
Article9. Stecco A, Stecco C, Macchi V, Porzionato A, Ferraro C, Masiero S, et al. RMI study and clinical correlations of ankle retinacula damage and outcomes of ankle sprain. Surg Radiol Anat. 2011; 33:881–890. DOI: 10.1007/s00276-011-0784-z.
Article10. Stecco C, Macchi V, Porzionato A, Morra A, Parenti A, Stecco A, et al. The ankle retinacula: morphological evidence of the proprioceptive role of the fascial system. Cells Tissues Organs. 2010; 192:200–210. DOI: 10.1159/000290225.
Article11. Martin RL, Davenport TE, Paulseth S, Wukich DK, Godges JJ. Orthopaedic Section American Physical Therapy Association. Ankle stability and movement coordination impairments: ankle ligament sprains. J Orthop Sports Phys Ther. 2013; 43:A1–A40. DOI: 10.2519/jospt.2013.0305.
Article12. Liu K, Gustavsen G, Kaminski TW. Increased frequency of ankle sprain does not lead to an increase in ligament laxity. Clin J Sport Med. 2013; 23:483–487. DOI: 10.1097/JSM.0b013e31829afc03.
Article13. Liu K, Gustavsen G, Royer T, Wikstrom EA, Glutting J, Kaminski TW. Increased ligament thickness in previously sprained ankles as measured by musculoskeletal ultrasound. J Athl Train. 2015; 50:193–198. DOI: 10.4085/1062-6050-49.3.77.
Article14. Kemmochi M, Sasaki S, Fujisaki K, Oguri Y, Kotani A, Ichimura S. A new classification of anterior talofibular ligament injuries based on ultrasonography findings. J Orthop Sci. 2016; 21:770–778. DOI: 10.1016/j.jos.2016.06.011.
Article15. Hua Y, Yang Y, Chen S, Cai Y. Ultrasound examination for the diagnosis of chronic anterior talofibular ligament injury. Acta Radiol. 2012; 53:1142–1145. DOI: 10.1258/ar.2012.120171.
Article16. Natus. NeuroCom: clinical integration seminar lecture manual. Clackamas: NeuroCom;2010.17. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39:175–191. DOI: 10.3758/BF03193146.
Article18. Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, Elkins B. The reliability of an instrumented device for measuring components of the star excursion balance test. N Am J Sports Phys Ther. 2009; 4:92–99.19. Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh JH, Naugle KE, Borsa PA. Self-assessed disability and functional performance in individuals with and without ankle instability: a case control study. J Orthop Sports Phys Ther. 2009; 39:458–467. DOI: 10.2519/jospt.2009.2989.
Article20. Nakagawa L, Hoffman M. Performance in static, dynamic, and clinical tests of postural control in individuals with recurrent ankle sprains. J Sport Rehabil. 2004; 13:255–268. DOI: 10.1123/jsr.13.3.255.
Article21. McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part I: can deficits be detected with instrumented testing. J Athl Train. 2008; 43:293–304. DOI: 10.4085/1062-6050-43.3.293.
Article22. Hiller CE, Nightingale EJ, Lin CW, Coughlan GF, Caulfield B, Delahunt E. Characteristics of people with recurrent ankle sprains: a systematic review with meta-analysis. Br J Sports Med. 2011; 45:660–672. DOI: 10.1136/bjsm.2010.077404.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Reconstruction of Lateral Capsule-ligament Complex with Reinforcement by Periosteal Flap of Distal Fibula and Inferior Extensor Retinaculum for Chronic Lateral Ankle Instability
- Arthrography of the ankle sprains
- Ankle Sprains: Epidemiology, Anatomy and Injury Mechanism
- Mid-foot retinaculum: an unrecognized entity
- Avulsion Fracture of the Talar Attachment of the Anterior Talofibular Ligament in Pediatric Patient: A Case Report