J Pathol Transl Med.
2019 Mar;53(2):119-124. 10.4132/jptm.2018.10.18.
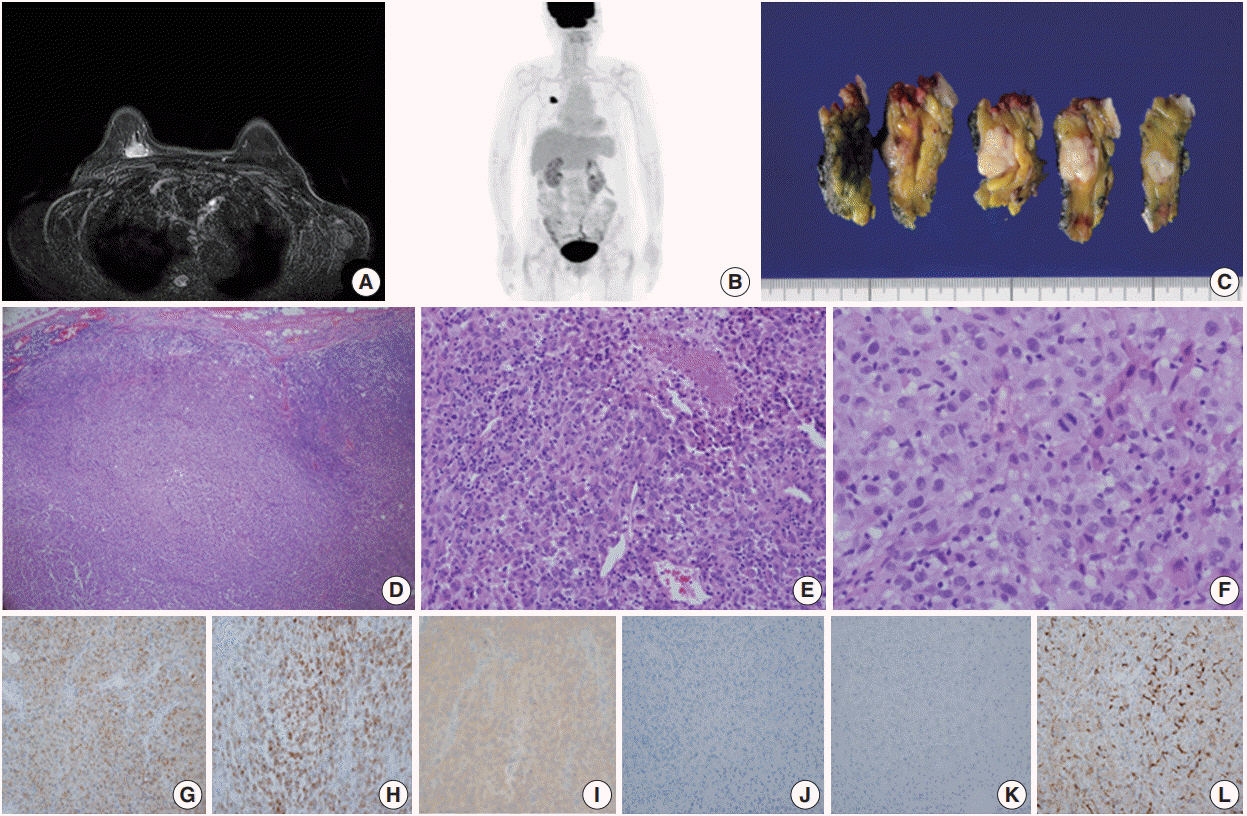
Primary Malignant Melanoma of the Breast: A Report of Two Cases
- Affiliations
-
- 1Department of Pathology, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Pathology, National Cancer Center, Goyang, Korea. ymk@ncc.re.kr
- 3Center for Breast Cancer, National Cancer Center, Goyang, Korea.
- 4Center for Specific Organs Center, National Cancer Center, Goyang, Korea.
- KMID: 2465451
- DOI: http://doi.org/10.4132/jptm.2018.10.18
Abstract
- Primary malignant melanoma of the breast (PMMB) is a rare tumor with only a few case reports available in the literature. We report two cases of PMMB, one derived from the breast parenchyma and the other from the breast skin. The first case consisted of atypical epithelioid cells without overt melanocytic differentiation like melanin pigments. The tumor cells showed diffuse positivity for S100 protein, tyrosinase, and BRAF V600E. However, the tumor cells were negative for cytokeratin, epithelial membrane antigen, and HMB-45. The second case showed atypical melanocytic proliferation with heavy melanin pigmentation. The tumor cells were positive for S100 protein, HMB-45, tyrosinase, and BRAF V600E. These two cases represent two distinct presentations of PMMB in terms of skin involvement, melanin pigmentation, and HMB-45 positivity. Although PMMB is very rare, the possibility of this entity should be considered in malignant epithelioid neoplasms in the breast parenchyma.
Keyword
MeSH Terms
Figure
Reference
-
1. Hussein MR. Extracutaneous malignant melanomas. Cancer Invest. 2008; 26:516–34.
Article2. McLaughlin CC, Wu XC, Jemal A, Martin HJ, Roche LM, Chen VW. Incidence of noncutaneous melanomas in the U.S. Cancer. 2005; 103:1000–7.
Article3. Kurul S, Tas F, Buyukbabani N, Mudun A, Baykal C, Camlica H. Different manifestations of malignant melanoma in the breast: a report of 12 cases and a review of the literature. Jpn J Clin Oncol. 2005; 35:202–6.
Article4. Drueppel D, Schultheis B, Solass W, Ergonenc H, Tempfer CB. Primary malignant melanoma of the breast: case report and review of the literature. Anticancer Res. 2015; 35:1709–13.5. Rassouli M, Voutsadakis IA. Primary noncutaneous malignant melanoma of the breast. Breast J. 2016; 22:688–91.
Article6. Alzaraa A, Sharma N. Primary cutaneous melanoma of the breast: a case report. Cases J. 2008; 1:212.
Article7. Williams SA, Ehlers RA 2nd, Hunt KK, et al. Metastases to the breast from nonbreast solid neoplasms: presentation and determinants of survival. Cancer. 2007; 110:731–7.8. Oh YL, Ko YH. Fine needle aspiration cytology of metastatic melanoma in the breast: a case report. Korean J Cytopathol. 1998; 9:111–6.9. Bendic A, Bozic M, Durdov MG. Metaplastic breast carcinoma with melanocytic differentiation. Pathol Int. 2009; 59:676–80.
Article10. Liu D, Rudland PS, Sibson DR, Platt-Higgins A, Barraclough R. Expression of calcium-binding protein S100A2 in breast lesions. Br J Cancer. 2000; 83:1473–9.
Article11. Blessing K, Sanders DS, Grant JJ. Comparison of immunohistochemical staining of the novel antibody melan-A with S100 protein and HMB-45 in malignant melanoma and melanoma variants. Histopathology. 1998; 32:139–46.
Article12. Ohsie SJ, Sarantopoulos GP, Cochran AJ, Binder SW. Immunohistochemical characteristics of melanoma. J Cutan Pathol. 2008; 35:433–44.
Article13. Yang L, Chen Y, Cui T, et al. Identification of biomarkers to distinguish clear cell sarcoma from malignant melanoma. Hum Pathol. 2012; 43:1463–70.
Article14. Long GV, Wilmott JS, Capper D, et al. Immunohistochemistry is highly sensitive and specific for the detection of V600E BRAF mutation in melanoma. Am J Surg Pathol. 2013; 37:61–5.
Article15. Petersson F, Ivan D, Kazakov DV, Michal M, Prieto VG. Pigmented Paget disease: a diagnostic pitfall mimicking melanoma. Am J Dermatopathol. 2009; 31:223–6.16. Bernardo MM, Mascarenhas MJ, Lopes DP. Primary malignant melanoma of the breast. Acta Med Port. 1980; 2:39–43.17. Roy S, Dhingra K, Mandal S, Khurana N. Unusual presentation of metastatic amelanotic melanoma of unknown primary origin as a solitary breast lump. Melanoma Res. 2008; 18:447–50.
Article18. Biswas A, Goyal S, Jain A, et al. Primary amelanotic melanoma of the breast: combating a rare cancer. Breast Cancer. 2014; 21:236–40.
Article19. He Y, Mou J, Luo D, Gao B, Wen Y. Primary malignant melanoma of the breast: a case report and review of the literature. Oncol Lett. 2014; 8:238–40.
Article