Anesth Pain Med.
2019 Oct;14(4):393-400. 10.17085/apm.2019.14.4.393.
Optic nerve sheath diameter changes during gynecologic surgery in the Trendelenburg position: comparison of propofol-based total intravenous anesthesia and sevoflurane anesthesia
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Ewha Womans University College of Medicine, Seoul, Korea. leehee@ewha.ac.kr
- KMID: 2465335
- DOI: http://doi.org/10.17085/apm.2019.14.4.393
Abstract
- BACKGROUND
Elevated intracranial pressure (ICP), a disadvantage of laparoscopic or robotic surgery, is caused by the steep angle of the Trendelenburg position and the COâ‚‚ pneumoperitoneum. Recently, sonographically measured optic nerve sheath diameter (ONSD) was suggested as a simple and non-invasive method for detecting increased ICP. This study aimed to explore the changes in ONSD in relation to different anesthetic agents used in gynecologic surgery.
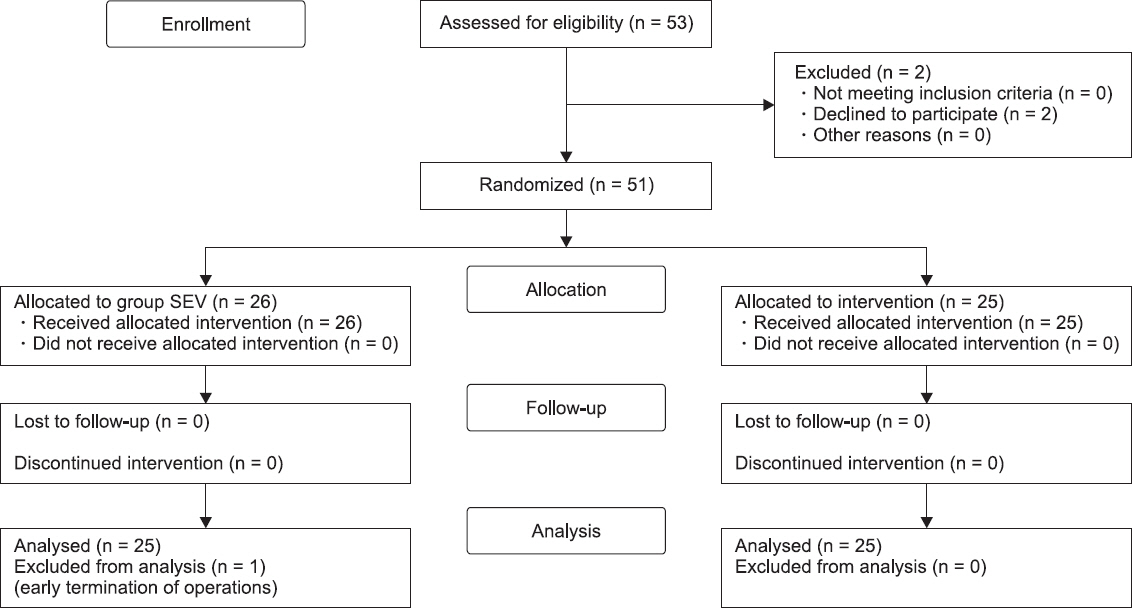
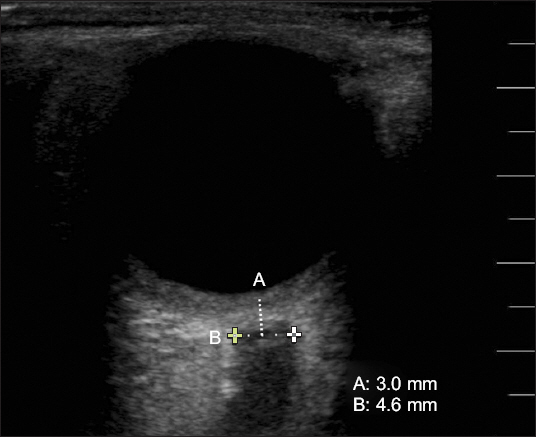
METHODS
Fifty patients were randomly allocated to two groups, sevoflurane (group SEV, n = 25) and propofol-based total intravenous anesthesia (TIVA) group (group TIVA, n = 25). The ONSD was measured at five time points (T0-T4): T0 was measured 5 min after induction of anesthesia in the supine position; T1, T2, and T3 were measured at 5, 15, and 30 min after COâ‚‚ pneumoperitoneum induction in the Trendelenburg position; and T4 was measured at 5 min after discontinuation of COâ‚‚ pneumoperitoneum in the supine position. Respiratory and hemodynamic variables were also recorded.
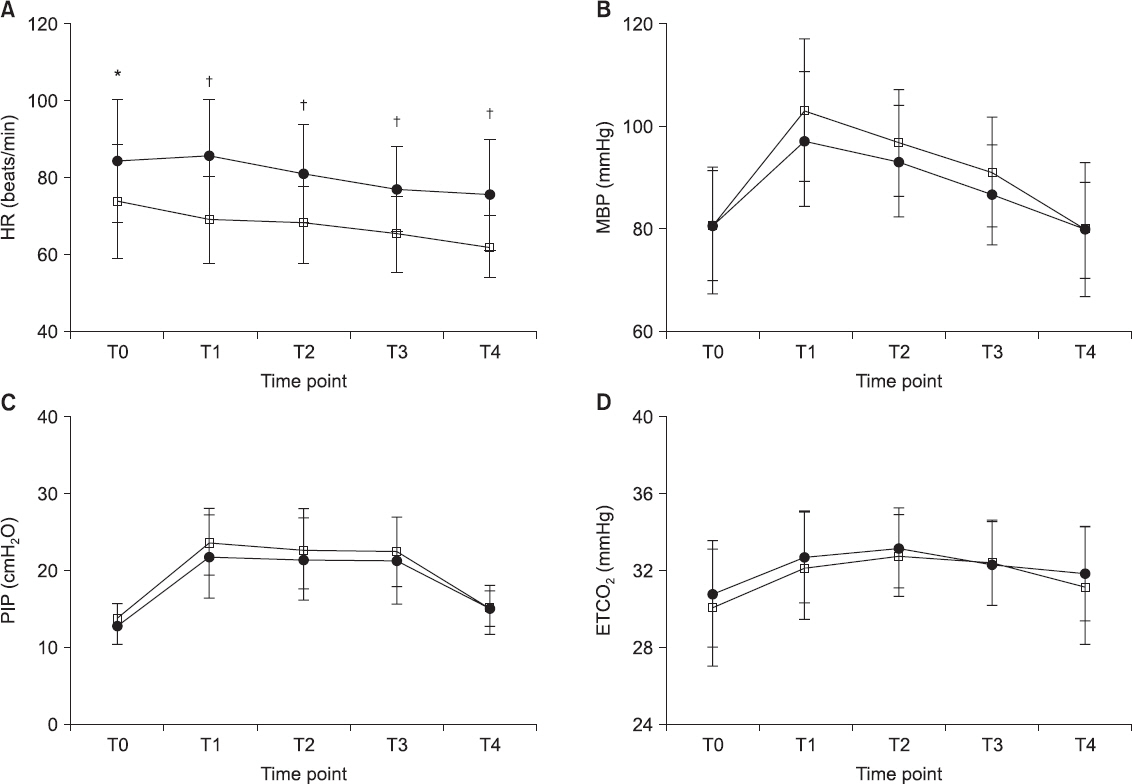
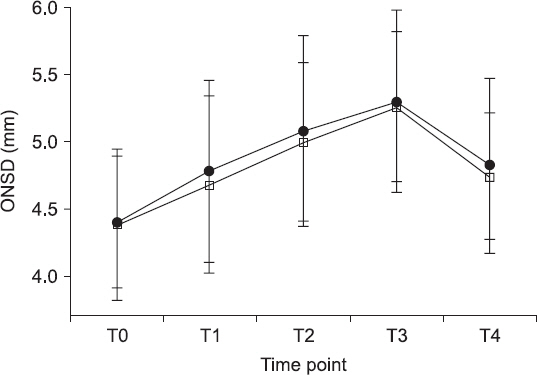
RESULTS
The intra-group changes in mean ONSD in the Trendelenburg position were significantly increased in both groups. However, inter-group changes in mean ONSD were not significantly different at T0, T1, T2, T3, and T4. Heart rates in group TIVA were significantly lower than those in group SEV at points T1-T4.
CONCLUSIONS
There was no significant difference in the ONSD between the two groups until 30 min into the gynecologic surgery with COâ‚‚ pneumoperitoneum in the Trendelenburg position. This study suggests that there is no difference in the ONSD between the two anesthetic methods.
MeSH Terms
Figure
Reference
-
1. Molloy BL. Implications for postoperative visual loss:steep Trendelenburg position and effects on intraocular pressure. AANA J. 2011; 79:115–21. PMID: 21560974.2. Halverson A, Buchanan R, Jacobs L, Shayani V, Hunt T, Riedel C, et al. Evaluation of mechanism of increased intracranial pressure with insufflation. Surg Endosc. 1998; 12:266–9. DOI: 10.1007/s004649900648. PMID: 9502709.3. Weber ED, Colyer MH, Lesser RL, Subramanian PS. Posterior ischemic optic neuropathy after minimally invasive prostatectomy. J Neuroophthalmol. 2007; 27:285–7. DOI: 10.1097/WNO.0b013e31815b9f67. PMID: 18090562.4. Mayer SA, Chong JY. Critical care management of increased intracranial pressure. J Intensive Care Med. 2002; 17:55–67. DOI: 10.1177/088506660201700201.5. Kristiansson H, Nissborg E, Bartek J Jr, Andresen M, Reinstrup P, Romner B. Measuring elevated intracranial pressure through noninvasive methods:a review of the literature. J Neurosurg Anesthesiol. 2013; 25:372–85. DOI: 10.1097/ANA.0b013e31829795ce. PMID: 23715045.6. Geeraerts T, Merceron S, Benhamou D, Vigué B, Duranteau J. Non-invasive assessment of intracranial pressure using ocular sonography in neurocritical care patients. Intensive Care Med. 2008; 34:2062–7. DOI: 10.1007/s00134-008-1149-x. PMID: 18509619.7. Chin JH, Seo H, Lee EH, Lee J, Hong JH, Hwang JH, et al. Sonographic optic nerve sheath diameter as a surrogate measure for intracranial pressure in anesthetized patients in the Trendelenburg position. BMC Anesthesiol. 2015; 15:43. DOI: 10.1186/s12871-015-0025-9. PMID: 25861241. PMCID: PMC4389861.8. Kim SH, Kim HJ, Jung KT. Position does not affect the optic nerve sheath diameter during laparoscopy. Korean J Anesthesiol. 2015; 68:358–63. DOI: 10.4097/kjae.2015.68.4.358. PMID: 26257848. PMCID: PMC4524934.9. Verdonck P, Kalmar AF, Suy K, Geeraerts T, Vercauteren M, Mot-trie A, et al. Optic nerve sheath diameter remains constant during robot assisted laparoscopic radical prostatectomy. PLoS One. 2014; 9:111916. DOI: 10.1371/journal.pone.0111916. PMID: 25369152. PMCID: PMC4219812.10. Kaur G, Sharma M, Kalra P, Purohit S, Chauhan K. Intraocular pressure changes during laparoscopic surgery in Trendelenburg position in patients anesthetized with propofol-based total intravenous anesthesia compared to sevoflurane anesthesia:a comparative study. Anesth Essays Res. 2018; 12:67–72. DOI: 10.4103/aer.AER_177_17. PMID: 29628557. PMCID: PMC5872896.11. Yoo YC, Shin S, Choi EK, Kim CY, Choi YD, Bai SJ. Increase in intraocular pressure is less with propofol than with sevoflurane during laparoscopic surgery in the steep Trendelenburg position. Can J Anaesth. 2014; 61:322–9. DOI: 10.1007/s12630-014-0112-2. PMID: 24500661.12. Kimberly HH, Shah S, Marill K, Noble V. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad Emerg Med. 2008; 15:201–4. DOI: 10.1111/j.1553-2712.2007.00031.x. PMID: 18275454.13. Girisgin AS, Kalkan E, Kocak S, Cander B, Gul M, Semiz M. The role of optic nerve ultrasonography in the diagnosis of elevated intracranial pressure. Emerg Med J. 2007; 24:251–4. DOI: 10.1136/emj.2006.040931. PMID: 17384377. PMCID: PMC2658229.14. Amini A, Eghtesadi R, Feizi AM, Mansouri B, Kariman H, Dola-tabadi AA, et al. Sonographic optic nerve sheath diameter as a screening tool for detection of elevated intracranial pressure. Emerg (Tehran). 2013; 1:15–9. PMID: 26495330. PMCID: PMC4614555.15. Tayal VS, Neulander M, Norton HJ, Foster T, Saunders T, Blaivas M. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med. 2007; 49:508–14. DOI: 10.1016/j.annemergmed.2006.06.040. PMID: 16997419.16. Moretti R, Pizzi B. Optic nerve ultrasound for detection of intracranial hypertension in intracranial hemorrhage patients:confirmation of previous findings in a different patient population. J Neurosurg Anesthesiol. 2009; 21:16–20. DOI: 10.1097/ANA.0b013e318185996a. PMID: 19098619.17. Rajajee V, Vanaman M, Fletcher JJ, Jacobs TL. Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocrit Care. 2011; 15:506–15. DOI: 10.1007/s12028-011-9606-8. PMID: 21769456.18. Kim MS, Bai SJ, Lee JR, Choi YD, Kim YJ, Choi SH. Increase in intracranial pressure during carbon dioxide pneumoperitoneum with steep Trendelenburg positioning proven by ultrasonographic measurement of optic nerve sheath diameter. J Endourol. 2014; 28:801–6. DOI: 10.1089/end.2014.0019. PMID: 24517270.19. Grubb RL Jr, Raichle ME, Eichling JO, Ter-Pogossian MM. The effects of changes in PaCO2 on cerebral blood volume, blood flow, and vascular mean transit time. Stroke. 1974; 5:630–9. DOI: 10.1161/01.STR.5.5.630. PMID: 4472361.20. Mowafi HA, Al-Ghamdi A, Rushood A. Intraocular pressure changes during laparoscopy in patients anesthetized with propofol total intravenous anesthesia versus isoflurane inhaled anesthesia. Anesth Analg. 2003; 97:471–4. DOI: 10.1213/01.ANE.0000067532.56354.58. PMID: 12873937.21. Hansen HC, Helmke K. The subarachnoid space surrounding the optic nerves An ultrasound study of the optic nerve sheath. Surg Radiol Anat. 1996; 18:323–8. DOI: 10.1007/BF01627611. PMID: 8983112.22. Eklund A, Smielewski P, Chambers I, Alperin N, Malm J, Czosny-ka M, et al. Assessment of cerebrospinal fluid outflow resistance. Med Biol Eng Comput. 2007; 45:719–35. DOI: 10.1007/s11517-007-0199-5. PMID: 17634761.23. Munis JR, Lozada LJ. Giraffes, siphons, and starling resistors. Cerebral perfusion pressure revisited. J Neurosurg Anesthesiol. 2000; 12:290–6. DOI: 10.1097/00008506-200007000-00029. PMID: 10905578.24. Yu J, Hong JH, Park JY, Hwang JH, Cho SS, Kim YK. Propofol attenuates the increase of sonographic optic nerve sheath diameter during robot-assisted laparoscopic prostatectomy:a randomized clinical trial. BMC Anesthesiol. 2018; 18:72. DOI: 10.1186/s12871-018-0523-7. PMID: 29925316. PMCID: PMC6011519.25. Choi ES, Jeon YT, Sohn HM, Kim DW, Choi SJ, In CB. Comparison of the effects of desflurane and total intravenous anesthesia on the optic nerve sheath diameter in robot assisted laparoscopic radical prostatectomy:a randomized controlled trial. Medicine (Baltimore). 2018; 97:12772. DOI: 10.1097/MD.0000000000012772. PMID: 30313092. PMCID: PMC6203556.26. Rehberg B, Bouillon T, Zinserling J, Hoeft A. Comparative pharmacodynamics modeling of the electroencephalography-slowing effect of isoflurane, sevoflurane, and desflurane. Anesthesiology. 1999; 91:397–405. DOI: 10.1097/00000542-199908000-00013. PMID: 10443602.27. Chui J, Mariappan R, Mehta J, Manninen P, Venkatraghavan L. Comparison of propofol and volatile agents for maintenance of anesthesia during elective craniotomy procedures:systematic review and meta-analysis. Can J Anaesth. 2014; 61:347–56. DOI: 10.1007/s12630-014-0118-9. PMID: 24482247.28. Blecha S, Harth M, Schlachetzki F, Zeman F, Blecha C, Flora P, et al. Changes in intraocular pressure and optic nerve sheath diameter in patients undergoing robotic-assisted laparoscopic prostatectomy in steep 45°Trendelenburg position. BMC Anesthesiol. 2017; 17:40. DOI: 10.1186/s12871-017-0333-3. PMID: 28284189. PMCID: PMC5351936.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison of the Effects of Propofol and Sevoflurane Anesthesias on Intraocular Pressure during Laparoscopic Hysterectomy
- Comparison of the effects of normal and low blood pressure regulation on the optic nerve sheath diameter in robot assisted laparoscopic radical prostatectomy
- Position does not affect the optic nerve sheath diameter during laparoscopy
- Postoperative Nausea and Vomiting after Strabismus Surgery in Pediatrics: A Comparison between VIMA with Sevoflurane and TIVA with Propofol
- A Comparative Study of the RecoveryCharacteristics for the Use of Propofol-Remifentanil Anesthesia or Sevoflurane-Remifentanil Anesthesia under Bispectral Index Guidance