Cancer Res Treat.
2019 Apr;51(2):474-482. 10.4143/crt.2018.059.
Long-term Outcomes of One Stage Surgery Using Transanal Colorectal Tube for Acute Colorectal Obstruction of Stage II/III Distal Colon Cancer
- Affiliations
-
- 1Department of Gastroenterology and Metabolism, Nagoya City University Graduate School of Medical Sciences, Nogoya, Japan. tshimura@med.nagoya-cu.ac.jp
- 2Department of Gastroenterology, Kasugai Municipal Hospital, Kasugai, Japan.
- 3Department of Gastroenterology, Japanese Red Cross Nagoya Daini Hospital, Nogoya, Japan.
- 4Department of Surgery, Kasugai Municipal Hospital, Kasugai, Japan.
- 5Department of Surgery, Japanese Red Cross Nagoya Daini Hospital, Nogoya, Japan.
- KMID: 2464394
- DOI: http://doi.org/10.4143/crt.2018.059
Abstract
- PURPOSE
Since oncological outcomes of transanal colorectal tube (TCT) placement, an endoscopic treatment for colorectal cancer (CRC) with acute colorectal obstruction (ACO), remain unknown, this study analyzed long-term outcomes of TCT placement for stage II/III CRC with ACO.
MATERIALS AND METHODS
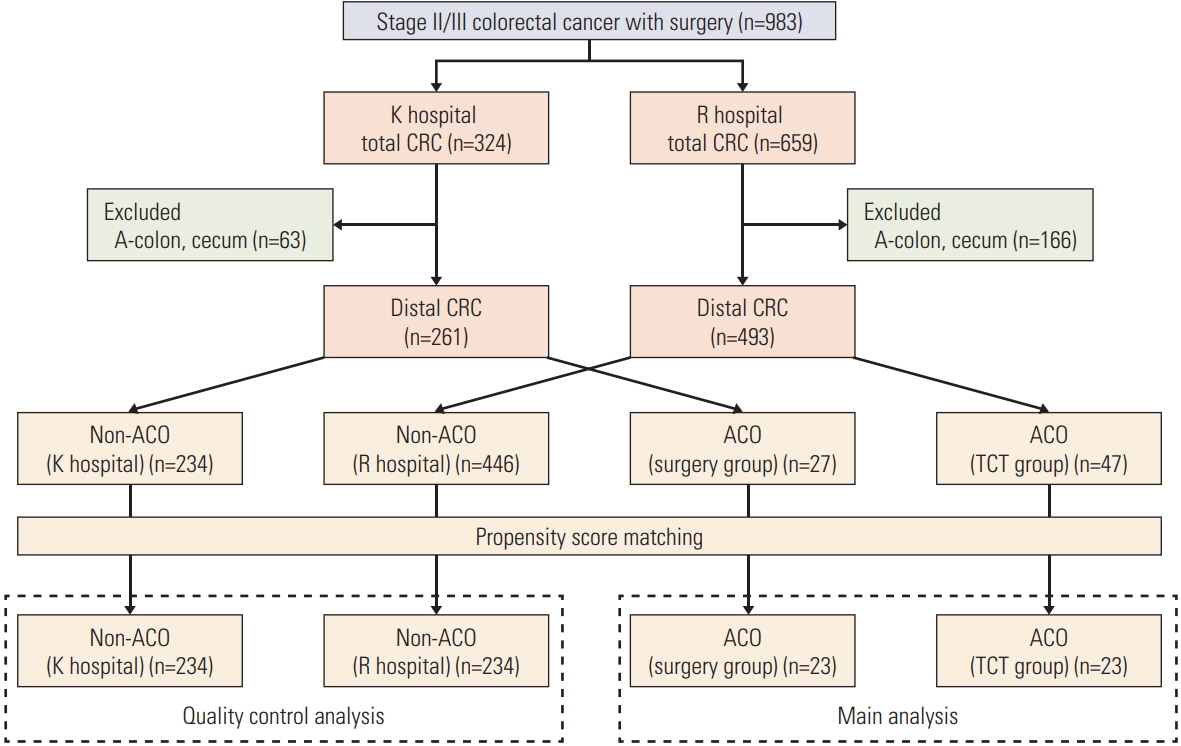
Data were retrospectively reviewed from consecutive patients with distal stage II/III CRC who underwent surgery between January 2007 and December 2011 at two Japanese hospitals. One hospital conducted emergency surgery and the other performed TCT placement as the standard treatment for all CRCs with ACO. Propensity score (PS) matching was used to adjust baseline characteristics between two groups.
RESULTS
Among 754 patients with distal stage II/III CRC, 680 did not have ACO (non-ACO group) and 74 had ACO (ACO group). The PS matching between both hospitals identified 234 pairs in the non-ACO group and 23 pairs in the ACO group. In the non-ACO group, the surgical quality was equivalent between the two institutions, with no significant differences in overall survival (OS) and disease-free survival (DFS). In the ACO group, the rate of primary resection/anastomosis was higher in the TCT group than in the surgery group (87.0% vs. 26.1%, p < 0.001). No significant differences were noted between the surgery and the TCT groups in OS (5-year OS, 61.9% vs. 51.5%; p=0.490) and DFS (5-year DFS, 45.9% vs. 38.3%; p=0.658).
CONCLUSION
TCT placement can achieve similar long-term outcomes to emergency surgery, with a high rate of primary resection/anastomosis for distal stage II/III colon cancer with ACO.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015; 136:E359–86.
Article2. De Salvo GL, Gava C, Pucciarelli S, Lise M. Curative surgery for obstruction from primary left colorectal carcinoma: primary or staged resection? Cochrane Database Syst Rev. 2004; (2):CD002101.
Article3. McArdle CS, McMillan DC, Hole DJ. The impact of blood loss, obstruction and perforation on survival in patients undergoing curative resection for colon cancer. Br J Surg. 2006; 93:483–8.
Article4. Biondo S, Pares D, Frago R, Marti-Rague J, Kreisler E, De Oca J, et al. Large bowel obstruction: predictive factors for postoperative mortality. Dis Colon Rectum. 2004; 47:1889–97.
Article5. Katoh H, Yamashita K, Wang G, Sato T, Nakamura T, Watanabe M. Prognostic significance of preoperative bowel obstruction in stage III colorectal cancer. Ann Surg Oncol. 2011; 18:2432–41.
Article6. Shimura T, Joh T. Evidence-based clinical management of acute malignant colorectal obstruction. J Clin Gastroenterol. 2016; 50:273–85.
Article7. Sjo OH, Larsen S, Lunde OC, Nesbakken A. Short term outcome after emergency and elective surgery for colon cancer. Colorectal Dis. 2009; 11:733–9.
Article8. Lee YM, Law WL, Chu KW, Poon RT. Emergency surgery for obstructing colorectal cancers: a comparison between right-sided and left-sided lesions. J Am Coll Surg. 2001; 192:719–25.9. Tan KK, Sim R. Surgery for obstructed colorectal malignancy in an Asian population: predictors of morbidity and comparison between left- and right-sided cancers. J Gastrointest Surg. 2010; 14:295–302.
Article10. Ng KC, Law WL, Lee YM, Choi HK, Seto CL, Ho JW. Self-expanding metallic stent as a bridge to surgery versus emergency resection for obstructing left-sided colorectal cancer: a case-matched study. J Gastrointest Surg. 2006; 10:798–803.
Article11. Martinez-Santos C, Lobato RF, Fradejas JM, Pinto I, Ortega-Deballon P, Moreno-Azcoita M. Self-expandable stent before elective surgery vs. emergency surgery for the treatment of malignant colorectal obstructions: comparison of primary anastomosis and morbidity rates. Dis Colon Rectum. 2002; 45:401–6.12. Tan CJ, Dasari BV, Gardiner K. Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg. 2012; 99:469–76.13. Ye GY, Cui Z, Chen L, Zhong M. Colonic stenting vs emergent surgery for acute left-sided malignant colonic obstruction: a systematic review and meta-analysis. World J Gastroenterol. 2012; 18:5608–15.14. Huang X, Lv B, Zhang S, Meng L. Preoperative colonic stents versus emergency surgery for acute left-sided malignant colonic obstruction: a meta-analysis. J Gastrointest Surg. 2014; 18:584–91.
Article15. Alcantara M, Serra-Aracil X, Falco J, Mora L, Bombardo J, Navarro S. Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement in obstructive left-sided colonic cancer. World J Surg. 2011; 35:1904–10.
Article16. Ghazal AH, El-Shazly WG, Bessa SS, El-Riwini MT, Hussein AM. Colonic endolumenal stenting devices and elective surgery versus emergency subtotal/total colectomy in the management of malignant obstructed left colon carcinoma. J Gastrointest Surg. 2013; 17:1123–9.
Article17. Sloothaak DA, van den Berg MW, Dijkgraaf MG, Fockens P, Tanis PJ, van Hooft JE, et al. Oncological outcome of malignant colonic obstruction in the Dutch Stent-In 2 trial. Br J Surg. 2014; 101:1751–7.18. van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RG, DeWitt JM, Donnellan F, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2014; 46:990–1053.
Article19. Yamada T, Shimura T, Sakamoto E, Kurumiya Y, Komatsu S, Iwasaki H, et al. Preoperative drainage using a transanal tube enables elective laparoscopic colectomy for obstructive distal colorectal cancer. Endoscopy. 2013; 45:265–71.
Article20. Horiuchi A, Nakayama Y, Tanaka N, Kajiyama M, Fujii H, Yokoyama T, et al. Acute colorectal obstruction treated by means of transanal drainage tube: effectiveness before surgery and stenting. Am J Gastroenterol. 2005; 100:2765–70.
Article21. Araki Y, Isomoto H, Matsumoto A, Kaibara A, Yasunaga M, Hayashi K, et al. Endoscopic decompression procedure in acute obstructing colorectal cancer. Endoscopy. 2000; 32:641–3.
Article22. Horiuchi A, Maeyama H, Ochi Y, Morikawa A, Miyazawa K. Usefulness of Dennis Colorectal Tube in endoscopic decompression of acute, malignant colonic obstruction. Gastrointest Endosc. 2001; 54:229–32.
Article23. Tanaka T, Furukawa A, Murata K, Sakamoto T. Endoscopic transanal decompression with a drainage tube for acute colonic obstruction: clinical aspects of preoperative treatment. Dis Colon Rectum. 2001; 44:418–22.24. Fischer A, Schrag HJ, Goos M, Obermaier R, Hopt UT, Baier PK. Transanal endoscopic tube decompression of acute colonic obstruction: experience with 51 cases. Surg Endosc. 2008; 22:683–8.
Article25. Xu M, Zhong Y, Yao L, Xu J, Zhou P, Wang P, et al. Endoscopic decompression using a transanal drainage tube for acute obstruction of the rectum and left colon as a bridge to curative surgery. Colorectal Dis. 2009; 11:405–9.
Article26. Shigeta K, Baba H, Yamafuji K, Kaneda H, Katsura H, Kubochi K. Outcomes for patients with obstructing colorectal cancers treated with one-stage surgery using transanal drainage tubes. J Gastrointest Surg. 2014; 18:1507–13.
Article27. Sobin L, Gospodarowicz M, Wittekind C. TNM classification of malignant tumours. 7th ed. Hoboken, NJ: John Wiley & Sons, Inc.;2009.28. Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007; 18:805–35.29. Sabbagh C, Chatelain D, Trouillet N, Mauvais F, Bendjaballah S, Browet F, et al. Does use of a metallic colon stent as a bridge to surgery modify the pathology data in patients with colonic obstruction? A case-matched study. Surg Endosc. 2013; 27:3622–31.
Article30. Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol. 2012; 17:1–29.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of long-term oncologic outcomes of stage III colorectal cancer following laparoscopic versus open surgery
- Long-term Outcomes of Laparoscopic Surgery for Colorectal Cancer
- The Prognostic Impact of Obstructed Colorectal Cancer
- The Prognosis and Recurrence Pattern of Right- and Left-Sided Colon Cancer in Stage II, Stage III, and Liver Metastasis After Curative Resection
- Comparison of long-term outcomes of colonic stenting as a “bridge to surgery” and emergency surgery in patients with left-sided malignant colonic obstruction