Ann Hepatobiliary Pancreat Surg.
2019 Nov;23(4):353-358. 10.14701/ahbps.2019.23.4.353.
Residual gall bladder: An emerging disease after safe cholecystectomy
- Affiliations
-
- 1Department of General Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India. vikaspgi@gmail.com
- 2Government Medical College, Chandigarh, India.
- 3Department of Radiodiagnosis, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
- 4Department of Gastroenterology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
- KMID: 2464324
- DOI: http://doi.org/10.14701/ahbps.2019.23.4.353
Abstract
- BACKGROUNDS/AIMS
Residual gallbladder mucosa left after subtotal/partial cholecystectomy is prone to develop recurrent lithiasis and become symptomatic, which mandates surgical removal.
METHODS
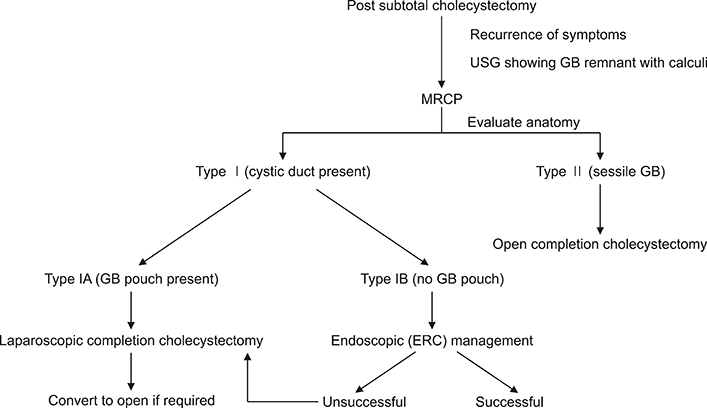
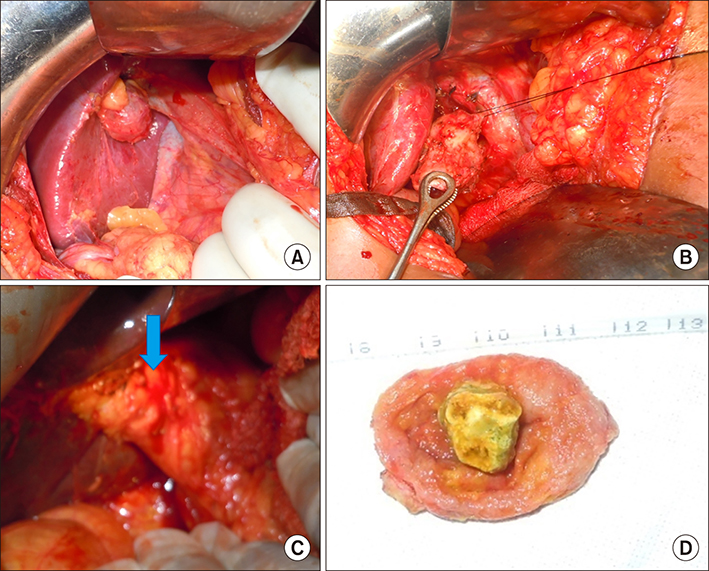
We retrospectively evaluated the patients with residual gallbladder referred to us from January 2011 to December 2017. Based on MRCP we classified calot's anatomy to - type I where cystic duct was seen and type II where sessile GB stump was seen.
RESULTS
21 patients with median age 38 years and M:F::1:9.5, had undergone cholecystectomy (3 months-20 years) prior, presented with recurrent biliary pain. 3 had jaundice (CBD stone, Mirizzi and biliary stricture), 1 had pancreatitis and one had malignancy of the GB. Imaging revealed type I anatomy in 14 (67%) and type II in 7 (33%). All underwent completion cholecystectomy - open in 18 and laparoscopic in 3 (one converted to open). Additional procedure was required in 5 patients - CBD exploration in 2 (10%) and one each Hepatico-jejunostomy, extended cholecystectomy and splenectomy. Median hospital stay was 1 day. There was no mortality and 10% morbidity. One patient with malignancy died at 2 years, two died of unrelated cause, one developed incisional hernia and the remaining were well at a median follow up of 29 months.
CONCLUSIONS
Residual GB lithiasis should be suspected if there are recurrent symptoms after cholecystectomy. MRCP based proposed classification can guide the management strategy. Completion cholecystectomy is curative.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim Y, Wima K, Jung AD, Martin GE, Dhar VK, Shah SA. Laparoscopic subtotal cholecystectomy compared to total cholecystectomy: a matched national analysis. J Surg Res. 2017; 218:316–321.2. Dissanaike S. A step-by-step guide to laparoscopic subtotal fenestrating cholecystectomy: a damage control approach to the difficult gallbladder. J Am Coll Surg. 2016; 223:e15–e18.3. Shin M, Choi N, Yoo Y, Kim Y, Kim S, Mun S. Clinical outcomes of subtotal cholecystectomy performed for difficult cholecystectomy. Ann Surg Treat Res. 2016; 91:226–232.4. Nakajima J, Sasaki A, Obuchi T, Baba S, Nitta H, Wakabayashi G. Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg Today. 2009; 39:870–875.5. Jara G, Rosciano J, Barrios W, Vegas L, Rodríguez O, Sánchez R, et al. Laparoscopic subtotal cholecystectomy: a surgical alternative to reduce complications in complex cases. Cir Esp. 2017; 95:465–470.6. van Dijk AH, Donkervoort SC, Lameris W, de Vries E, Eijsbouts QAJ, Vrouenraets BC, et al. Short- and long-term outcomes after a reconstituting and fenestrating subtotal cholecystectomy. J Am Coll Surg. 2017; 225:371–379.7. Palanivelu C, Rangarajan M, Jategaonkar PA, Madankumar MV, Anand NV. Laparoscopic management of remnant cystic duct calculi: a retrospective study. Ann R Coll Surg Engl. 2009; 91:25–29.8. Singh A, Kapoor A, Singh RK, Prakash A, Behari A, Kumar A, et al. Management of residual gall bladder: a 15-year experience from a north Indian tertiary care centre. Ann Hepatobiliary Pancreat Surg. 2018; 22:36–41.9. Tantia O, Jain M, Khanna S, Sen B. Post cholecystectomy syndrome: role of cystic duct stump and re-intervention by laparoscopic surgery. J Minim Access Surg. 2008; 4:71–75.10. Concors SJ, Kirkland ML, Schuricht AL, Dempsey DT, Morris JB, Vollmer CM, et al. Resection of gallbladder remnants after subtotal cholecystectomy: presentation and management. HPB (Oxford). 2018; 20:1062–1066.11. Chowbey P, Soni V, Sharma A, Khullar R, Baijal M. Residual gallstone disease - laparoscopic management. Indian J Surg. 2010; 72:220–225.12. Henneman D, da Costa DW, Vrouenraets BC, van Wagensveld BA, Lagarde SM. Laparoscopic partial cholecystectomy for the difficult gallbladder: a systematic review. Surg Endosc. 2013; 27:351–358.13. Parmar AK, Khandelwal RG, Mathew MJ, Reddy PK. Laparoscopic completion cholecystectomy: a retrospective study of 40 cases. Asian J Endosc Surg. 2013; 6:96–99.14. Zhu JG, Zhang ZT. Laparoscopic remnant cholecystectomy and transcystic common bile duct exploration for gallbladder/cystic duct remnant with stones and choledocholithiasis after cholecystectomy. J Laparoendosc Adv Surg Tech A. 2015; 25:7–11.15. Walsh RM, Chung RS, Grundfest-Broniatowski S. Incomplete excision of the gallbladder during laparoscopic cholecystectomy. Surg Endosc. 1995; 9:67–70.16. Matsui Y, Hirooka S, Kotsuka M, Yamaki S, Yamamoto T, Kosaka H, et al. Use of a piece of free omentum to prevent bile leakage after subtotal cholecystectomy. Surgery. 2018; 164:419–423.17. Do JH, Choi YS, Ze EY. Adenocarcinoma developed from remnant cystic duct after cholecystectomy. BMC Gastroenterol. 2014; 14:175.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biliary manometry in patients with gall stones: a comparison between patients with common bile duct stones, gall bladder stones, intra-hepatic duct stones, previous cholecystectomy, and controls
- Late Port Site Metastasis from Occult Gall Bladder Carcinoma After Laparoscopic Cholecystectomy for Cholelithiasis: The Role of 18F-FDG PET/CT
- Xanthogranulomatous Cholecystitis
- Gall bladder wal varices:Easy diagnosis with multiphase incremental bolus dynamic CT
- Clinical Analysis of Laparoscopic Cholecystectomy in Complicated Cholelithiasis