Hip Pelvis.
2019 Dec;31(4):216-223. 10.5371/hp.2019.31.4.216.
Hemiarthroplasty in the Hip Fracture Patient with Renal Impairment: To Cement or Not to Cement
- Affiliations
-
- 1Department of Orthopaedic Surgery, Tan Tock Seng Hospital, Singapore. tong_leng_tan@ttsh.com.sg
- KMID: 2464238
- DOI: http://doi.org/10.5371/hp.2019.31.4.216
Abstract
- PURPOSE
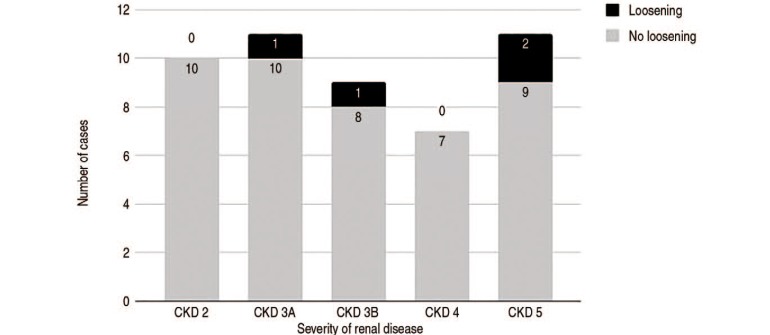
Patients with chronic kidney disease (CKD) have a higher risk of complications when undergoing hip hemiarthroplasty. The primary aim is to test the null hypothesis that there is no difference between cemented and uncemented stem loosening rates in patients with CKD who receive a hip hemiarthroplasty for femoral neck fractures. The secondary aim is to determine the effect of increasing severity of renal disease on the rate of stem loosening in this CKD patient subset.
MATERIALS AND METHODS
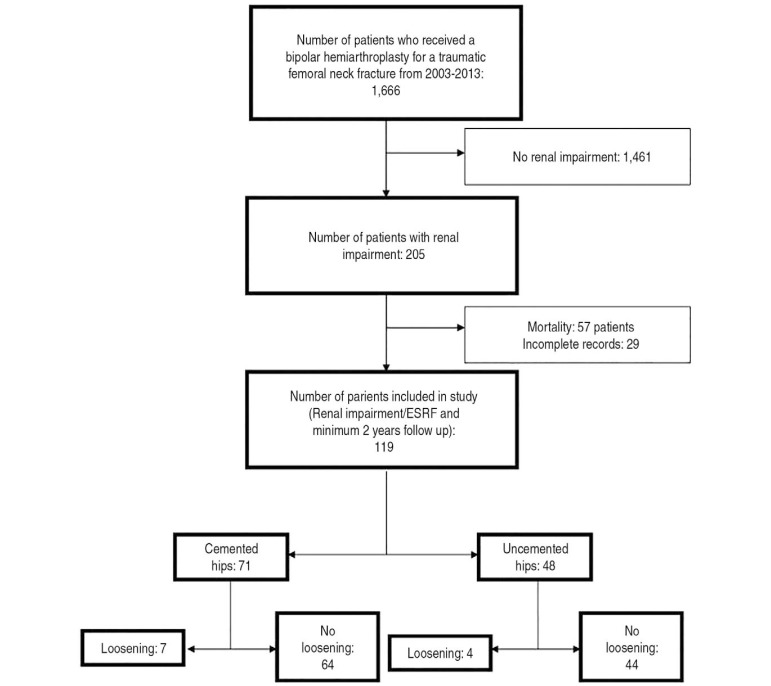
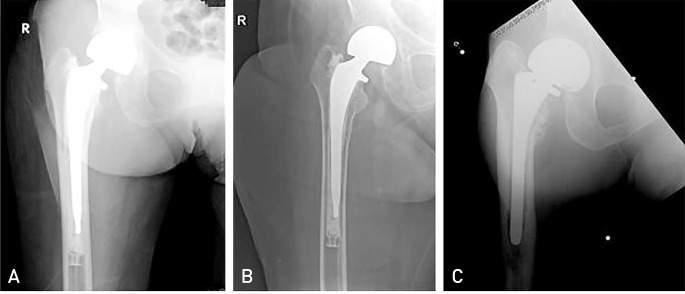
A retrospective study of all patients with CKD who underwent a hip hemiarthroplasty for a traumatic femoral-neck fracture between 2003 and 2013 was performed. Patients with a minimum of two-year follow-up were included; those with pathological fractures or loosening due to infection were excluded. The outcome measure was radiographic aseptic loosening of the stem, defined as progressive radiolucency of more than 2 mm, progressive subsidence or migration of the implant.
RESULTS
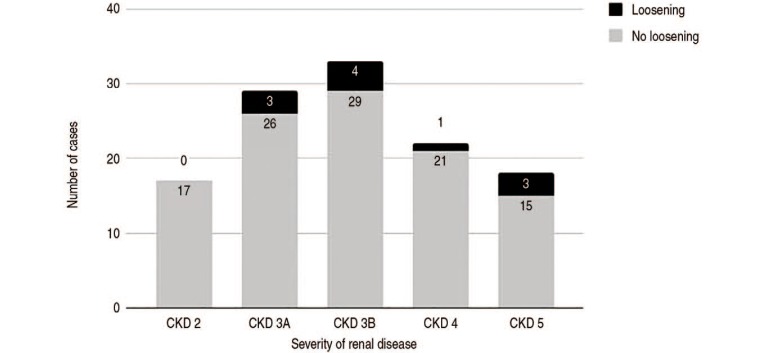
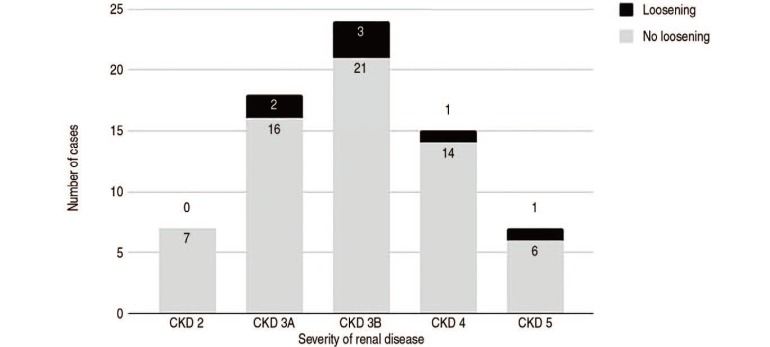
One-hundred and nineteen cases were included in this study. Loosening occurred in 11 cases (9.24%). A comparison between cemented and uncemented groups revealed no difference in the rate of loosening (P=0.079). In all cases, worsening renal function did not increase the rate of loosening (P=0.311). The rate of loosening did not increase with worsening renal function in either the cemented (P=0.678) or uncemented groups (P=0.307).
CONCLUSION
There is no difference in the rate of loosening between cemented and uncemented hemiarthroplasty for femoral neck fractures in the elderly with CKD. The rate of loosening did not increase with worsening renal function. All patients with renal impairment, not just those with end-stage renal failure, warrant close follow-up as early loosening can occur throughout the entire spectrum of renal disease.
MeSH Terms
Figure
Reference
-
1. Mataliotakis G, Lykissas MG, Mavrodontidis AN, Kontogeorgakos VA, Beris AE. Femoral neck fractures secondary to renal osteodystrophy. Literature review and treatment algorithm. J Musculoskelet Neuronal Interact. 2009; 9:130–137. PMID: 19724147.2. Karaeminogullari O, Demirors H, Sahin O, Ozalay M, Ozdemir N, Tandogan RN. Analysis of outcomes for surgically treated hip fractures in patients undergoing chronic hemodialysis. J Bone Joint Surg Am. 2007; 89:324–331. PMID: 17272447.
Article3. Toomey HE, Toomey SD. Hip arthroplasty in chronic dialysis patients. J Arthroplasty. 1998; 13:647–652. PMID: 9741441.
Article4. Blacha J, Kolodziej R, Karwanski M. Bipolar cemented hip hemiarthroplasty in patients with femoral neck fracture who are on hemodialysis is associated with risk of stem migration. Acta Orthop. 2009; 80:174–178. PMID: 19404798.
Article5. Kalra S, McBryde CW, Lawrence T. Intracapsular hip fractures in end-stage renal failure. Injury. 2006; 37:175–184. PMID: 16426611.
Article6. Gualtieri G, Vellani G, Dallari D, et al. Total hip arthroplasty in patients dialyzed or with renal transplants. Chir Organi Mov. 1995; 80:139–145. PMID: 7587515.7. Moe SM. Renal osteodystrophy or kidney-induced osteoporosis? Curr Osteoporos Rep. 2017; 15:194–197. PMID: 28497212.
Article8. Fritz J, Lurie B, Miller TT. Imaging of hip arthroplasty. Semin Musculoskelet Radiol. 2013; 17:316–327. PMID: 23787986.
Article9. Chang CY, Huang AJ, Palmer WE. Radiographic evaluation of hip implants. Semin Musculoskelet Radiol. 2015; 19:12–20. PMID: 25633021.
Article10. Barrack RL. Early failure of modern cemented stems. J Arthroplasty. 2000; 15:1036–1050. PMID: 11112201.
Article11. Naito M, Ogata K, Shiota E, Nakamoto M, Goya T. Hip arthroplasty in haemodialysis patients. J Bone Joint Surg Br. 1994; 76:428–431. PMID: 8175847.
Article12. Nagoya S, Nagao M, Takada J, Kuwabara H, Kaya M, Yamashita T. Efficacy of cementless total hip arthroplasty in patients on long-term hemodialysis. J Arthroplasty. 2005; 20:66–71. PMID: 15660062.
Article13. Li WC, Shih CH, Ueng SW, Shih HN, Lee MS, Hsieh PH. Uncemented total hip arthroplasty in chronic hemodialysis patients. Acta Orthop. 2010; 81:178–182. PMID: 20175645.
Article14. National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003; 42:S1–S201. PMID: 14520607.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unipolar Versub Bipolar Hip Hemiarthroplasty for Fractures of Femoral Neck in the Dlderly
- Effect of Pressurized Cement Insertion on Cardiopulmonary Parameters during Cemented Hip Hemiarthroplasty: A Randomized Prospective Study
- Cemented Total Hip Replacement Arthroplasty
- Predictors of Intraoperative Fractures during Hemiarthroplasty for the Treatment of Fragility Hip Fractures
- Total Hip Arthroplasty after Fracture of the Acetabulum