Yonsei Med J.
2019 Dec;60(12):1157-1163. 10.3349/ymj.2019.60.12.1157.
Cost-Effectiveness of Rate- and Rhythm-Control Drugs for Treating Atrial Fibrillation in Korea
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. cby6908@yuhs.ac
- 2Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea. preman@yuhs.ac
- 3Institute of Human Complexity and Systems Science, Yonsei University, Seoul, Korea.
- KMID: 2463794
- DOI: http://doi.org/10.3349/ymj.2019.60.12.1157
Abstract
- PURPOSE
Although the economic and mortality burden of atrial fibrillation (AF) is substantial, it remains unclear which treatment strategies for rate and rhythm control are most cost-effective. Consequently, economic factors can play an adjunctive role in guiding treatment selection.
MATERIALS AND METHODS
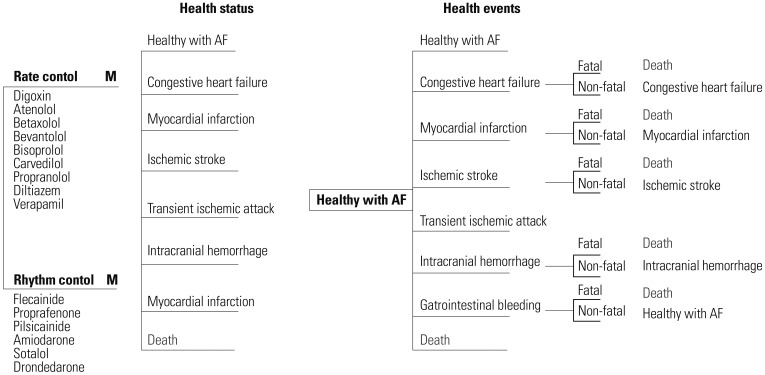
We built a Markov chain Monte Carlo model using the Korean Health Insurance Review & Assessment Service database. Drugs for rate control and rhythm control in AF were analyzed. Cost-effective therapies were selected using a cost-effectiveness ratio, calculated by net cost and quality-adjusted life years (QALY).
RESULTS
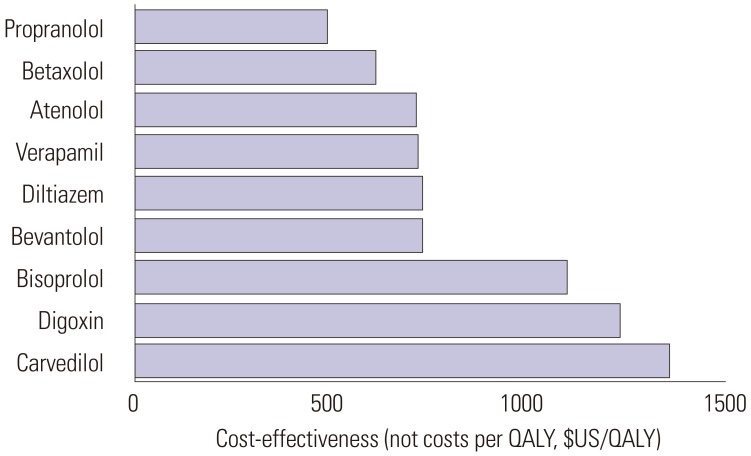
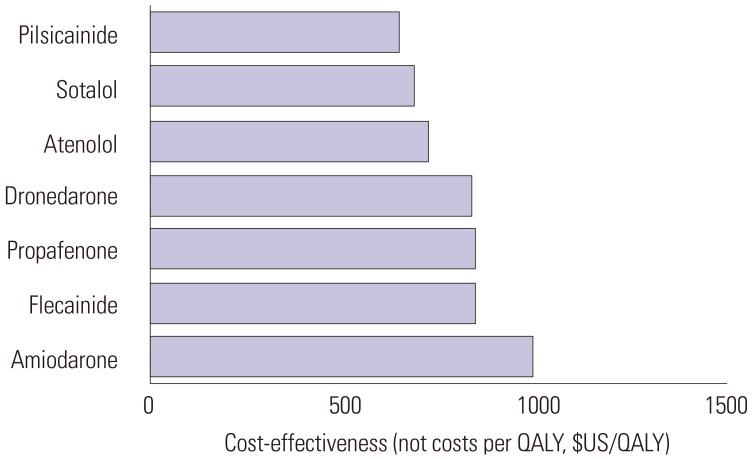
In the National Health Insurance Service data, 268149 patients with prevalent AF (age ≥18 years) were identified between January 1, 2013 and December 31, 2015. Among them, 212459 and 55690 patients were taking drugs for rate and rhythm control, respectively. Atenolol cost $714/QALY. Among the rate-control medications, the cost of propranolol was lowest at $487/QALY, while that of carvedilol was highest at $1363/QALY. Among the rhythm-control medications, the cost of pilsicainide was lowest at $638/QALY, while that of amiodarone was highest at $986/QALY. Flecainide and propafenone cost $834 and $830/QALY, respectively. The cost-effectiveness threshold of all drugs was lower than $30000/QALY. Compared with atenolol, the rate-control drugs propranolol, betaxolol, bevantolol, bisoprolol, diltiazem, and verapamil, as well as the rhythm-control drugs sotalol, pilsicainide, flecainide, propafenone, and dronedarone, showed better incremental cost-effectiveness ratios.
CONCLUSION
Propranolol and pilsicainide appear to be cost-effective in patients with AF in Korea assuming that drug usage or compliance is the same.
Keyword
MeSH Terms
-
Amiodarone
Atenolol
Atrial Fibrillation*
Betaxolol
Bisoprolol
Compliance
Cost-Benefit Analysis
Diltiazem
Flecainide
Humans
Insurance, Health
Korea*
Markov Chains
Mortality
National Health Programs
Propafenone
Propranolol
Quality-Adjusted Life Years
Sotalol
Verapamil
Amiodarone
Atenolol
Betaxolol
Bisoprolol
Diltiazem
Flecainide
Propafenone
Propranolol
Sotalol
Verapamil
Figure
Reference
-
1. Braunwald E. Cardiovascular Medicine at the turn of the millennium: triumphs, concerns, and opportunities. N Engl J Med. 1997; 337:1360–1369. PMID: 9358131.
Article2. Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998; 98:946–952. PMID: 9737513.3. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016; 37:2893–2962. PMID: 27567408.
Article4. January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1–e76. PMID: 24685669.5. Stewart S, Hart CL, Hole DJ, McMurray JJ. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002; 113:359–364. PMID: 12401529.
Article6. Maisel WH, Stevenson LW. Atrial fibrillation in heart failure: epidemiology, pathophysiology, and rationale for therapy. Am J Cardiol. 2003; 91(6A):2D–8D.
Article7. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991; 22:983–988. PMID: 1866765.
Article8. Kim TH, Yang PS, Uhm JS, Kim JY, Pak HN, Lee MH, et al. CHA2DS2-VASc Score (Congestive heart failure, hypertension, age ≥75 [doubled], diabetes mellitus, prior stroke or transient ischemic attack [doubled], vascular disease, age 65–74, female) for stroke in Asian patients with atrial fibrillation: a Korean nationwide sample cohort study. Stroke. 2017; 48:1524–1530. PMID: 28455320.9. Aronow WS. Management of the older person with atrial fibrillation. J Gerontol A Biol Sci Med Sci. 2002; 57:M352–M363. PMID: 12023264.
Article10. Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the An-Ticoagulation and risk factors in atrial fibrillation (ATRIA) study. JAMA. 2001; 285:2370–2375. PMID: 11343485.11. Lloyd-Jones DM, Wang TJ, Leip EP, Larson MG, Levy D, Vasan RS, et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004; 110:1042–1046. PMID: 15313941.12. Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006; 114:119–125. PMID: 16818816.
Article13. Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J. 2006; 27:949–953. PMID: 16527828.
Article14. Son MK, Lim NK, Cho MC, Park HY. Incidence and risk factors for atrial fibrillation in Korea: the National Health Insurance Service Database (2002–2010). Korean Circ J. 2016; 46:515–521. PMID: 27482260.
Article15. Kim D, Yang PS, Jang E, Yu HT, Kim TH, Uhm JS, et al. 10-year nationwide trends of the incidence, prevalence, and adverse outcomes of non-valvular atrial fibrillation nationwide health insurance data covering the entire Korean population. Am Heart J. 2018; 202:20–26. PMID: 29802976.
Article16. Lee H, Kim TH, Baek YS, Uhm JS, Pak HN, Lee MH, et al. The trends of atrial fibrillation-related hospital visit and cost, treatment pattern and mortality in Korea: 10-year nationwide sample cohort data. Korean Circ J. 2017; 47:56–64. PMID: 28154592.
Article17. Lee S, Anglade MW, Pham D, Pisacane R, Kluger J, Coleman CI. Cost-effectiveness of rivaroxaban compared to warfarin for stroke prevention in atrial fibrillation. Am J Cardiol. 2012; 110:845–851. PMID: 22651881.
Article18. O'Brien CL, Gage BF. Costs and effectiveness of ximelagatran for stroke prophylaxis in chronic atrial fibrillation. JAMA. 2005; 293:699–706. PMID: 15701911.19. Shah SV, Gage BF. Cost-effectiveness of dabigatran for stroke prophylaxis in atrial fibrillation. Circulation. 2011; 123:2562–2570. PMID: 21606397.
Article20. Kim H, Kim H, Cho SK, Kim JB, Joung B, Kim C. Cost-effectiveness of rivaroxaban compared to warfarin for stroke prevention in atrial fibrillation. Korean Circ J. 2019; 49:252–263. PMID: 30468041.
Article21. Wyse DG, Waldo AL, DiMarco JP, Domanski MJ, Rosenberg Y, Schron EB, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002; 347:1825–1833. PMID: 12466506.
Article22. Van Gelder IC, Hagens VE, Bosker HA, Kingma JH, Kamp O, Kingma T, et al. A comparison of rate control and rhythm control in patients with recurrent persistent atrial fibrillation. N Engl J Med. 2002; 347:1834–1840. PMID: 12466507.
Article23. Choi YJ, Kang KW, Kim TH, Cha MJ, Lee JM, Park J, et al. Comparison of rhythm and rate control strategies for stroke occurrence in a prospective cohort of atrial fibrillation patients. Yonsei Med J. 2018; 59:258–264. PMID: 29436194.
Article24. Marshall DA, Levy AR, Vidaillet H, Fenwick E, Slee A, Blackhouse G, et al. Cost-effectiveness of rhythm versus rate control in atrial fibrillation. Ann Intern Med. 2004; 141:653–661. PMID: 15520421.
Article25. Lee HY, Yang PS, Kim TH, Uhm JS, Pak HN, Lee MH, et al. Atrial fibrillation and the risk of myocardial infarction: a nation-wide propensity-matched study. Sci Rep. 2017; 7:12716. PMID: 28983076.
Article26. Lee SS, Kong KA, Kim D, Lim YM, Yang PS, Yi JE, et al. Clinical implication of an impaired fasting glucose and prehypertension related to new onset atrial fibrillation in a healthy Asian population without underlying disease: a nationwide cohort study in Korea. Eur Heart J. 2017; 38:2599–2607. PMID: 28662568.
Article27. Sullivan PW, Ghushchyan V. Preference-based EQ-5D index scores for chronic conditions in the United States. Med Decis Making. 2006; 26:410–420. PMID: 16855129.
Article28. Gage BF, Cardinalli AB, Owens DK. The effect of stroke and stroke prophylaxis with aspirin or warfarin on quality of life. Arch Intern Med. 1996; 156:1829–1836. PMID: 8790077.
Article29. Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA. 1996; 276:1253–1258. PMID: 8849754.
Article30. Hohnloser SH, Kuck KH, Lilienthal J. Rhythm or rate control in atrial fibrillation--Pharmacological Intervention in Atrial Fibrillation (PIAF): a randomised trial. Lancet. 2000; 356:1789–1794. PMID: 11117910.
Article31. Carlsson J, Miketic S, Windeler J, Cuneo A, Haun S, Micus S, et al. Randomized trial of rate-control versus rhythm-control in persistent atrial fibrillation: the Strategies of Treatment of Atrial Fibrillation (STAF) study. J Am Coll Cardiol. 2003; 41:1690–1696. PMID: 12767648.32. Eckman MH, Falk RH, Pauker SG. Cost-effectiveness of therapies for patients with nonvalvular atrial fibrillation. Arch Intern Med. 1998; 158:1669–1677. PMID: 9701102.
Article33. Catherwood E, Fitzpatrick WD, Greenberg ML, Holzberger PT, Malenka DJ, Gerling BR, et al. Cost-effectiveness of cardioversion and antiarrhythmic therapy in nonvalvular atrial fibrillation. Ann Intern Med. 1999; 130:625–636. PMID: 10215558.
Article34. Hagens VE, Vermeulen KM, TenVergert EM, Van Veldhuisen DJ, Bosker HA, Kamp O, et al. Rate control is more cost-effective than rhythm control for patients with persistent atrial fibrillation- -results from the RAte Control versus Electrical cardioversion (RACE) study. Eur Heart J. 2004; 25:1542–1549. PMID: 15342174.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Mechanism of and Preventive Therapy for Stroke in Patients with Atrial Fibrillation
- Optimal Rhythm Control Strategy in Patients With Atrial Fibrillation
- 2018 Korean Heart Rhythm Society Guidelines for Antiarrhythmic Drug Therapy in Non-valvular Atrial Fibrillation
- Mid-term Result of Operations for Atrial Fibrillation
- Relation between Atrial Fibrillation and Echocardiographic Size of Left Atrium