J Korean Neurosurg Soc.
2019 Nov;62(6):681-690. 10.3340/jkns.2019.0070.
Clinical Effectiveness of Percutaneous Epidural Neuroplasty According to the Type of Single-Level Lumbar Disc Herniation : A 12-Month Follow-Up Study
- Affiliations
-
- 1Department of Neurosurgery, Ajou University College of Medicine, Suwon, Korea.
- 2Department of Neurosurgery, Cham Teun Teun Research Institute, Seoul, Korea.
- 3Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea. shindongah@me.com
- KMID: 2463660
- DOI: http://doi.org/10.3340/jkns.2019.0070
Abstract
OBJECTIVE
To determine whether the outcomes of percutaneous epidural neuroplasty (PEN) are influenced by the type of lumbar disc herniation (LDH) and evaluate the effectiveness of PEN in patients with single-level LDH.
METHODS
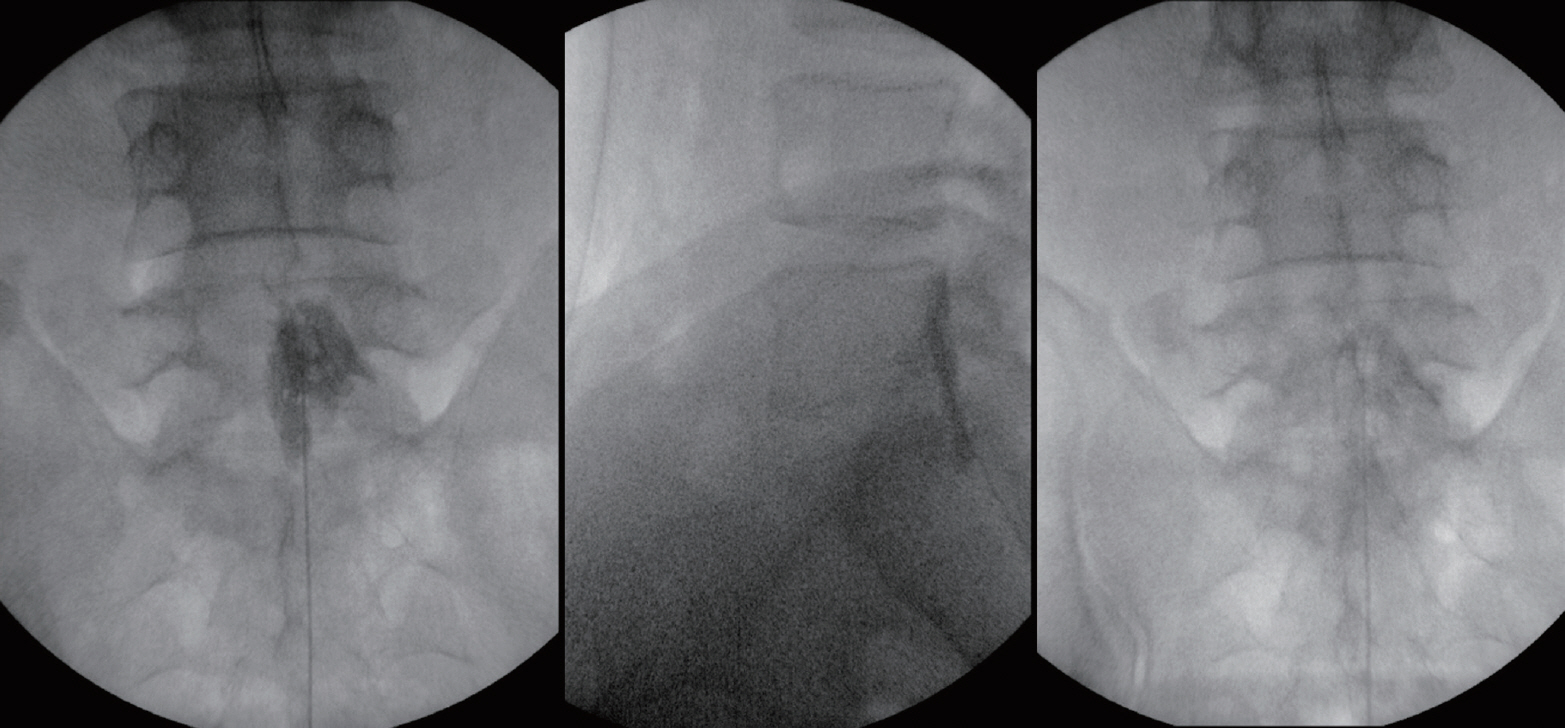
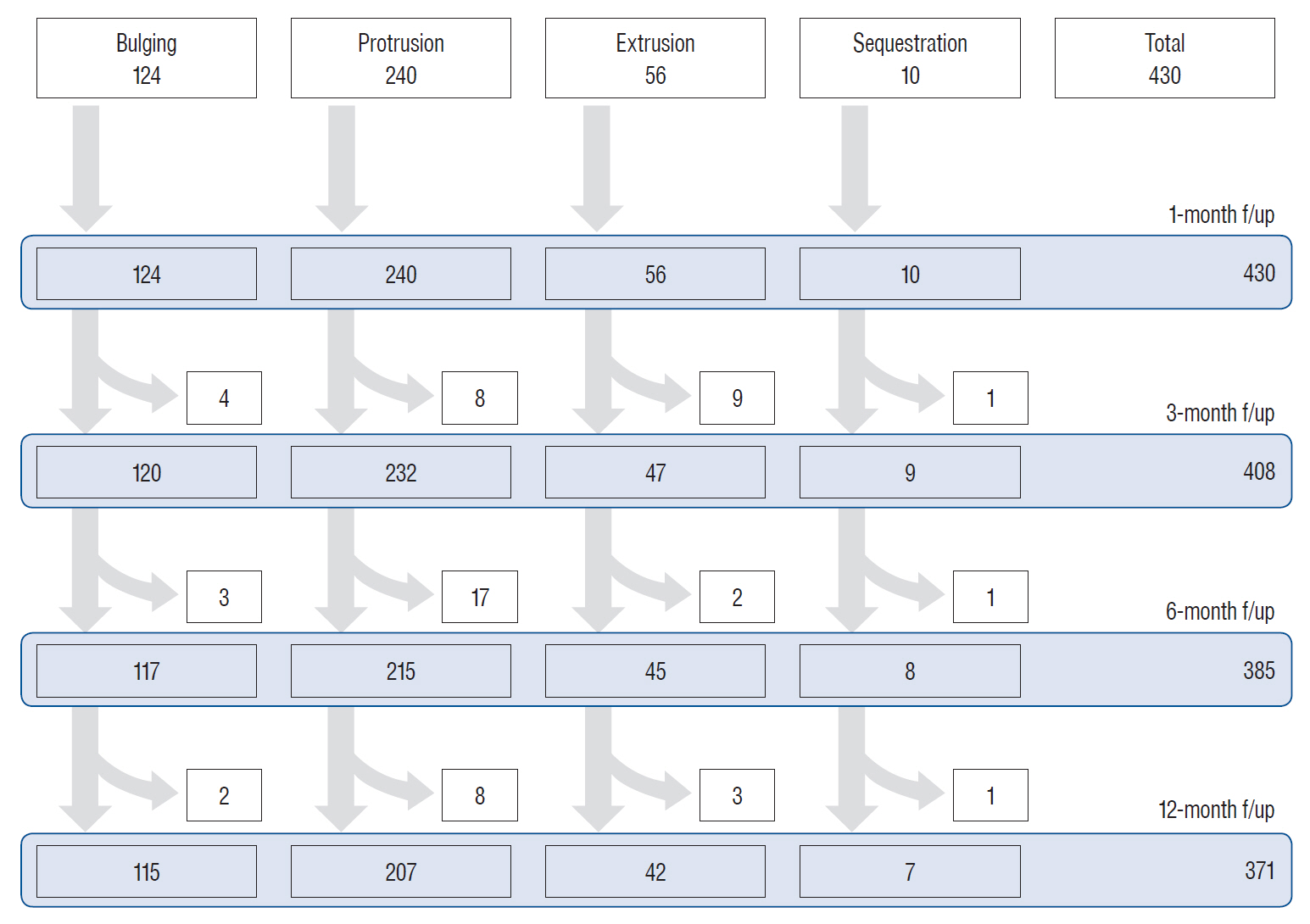
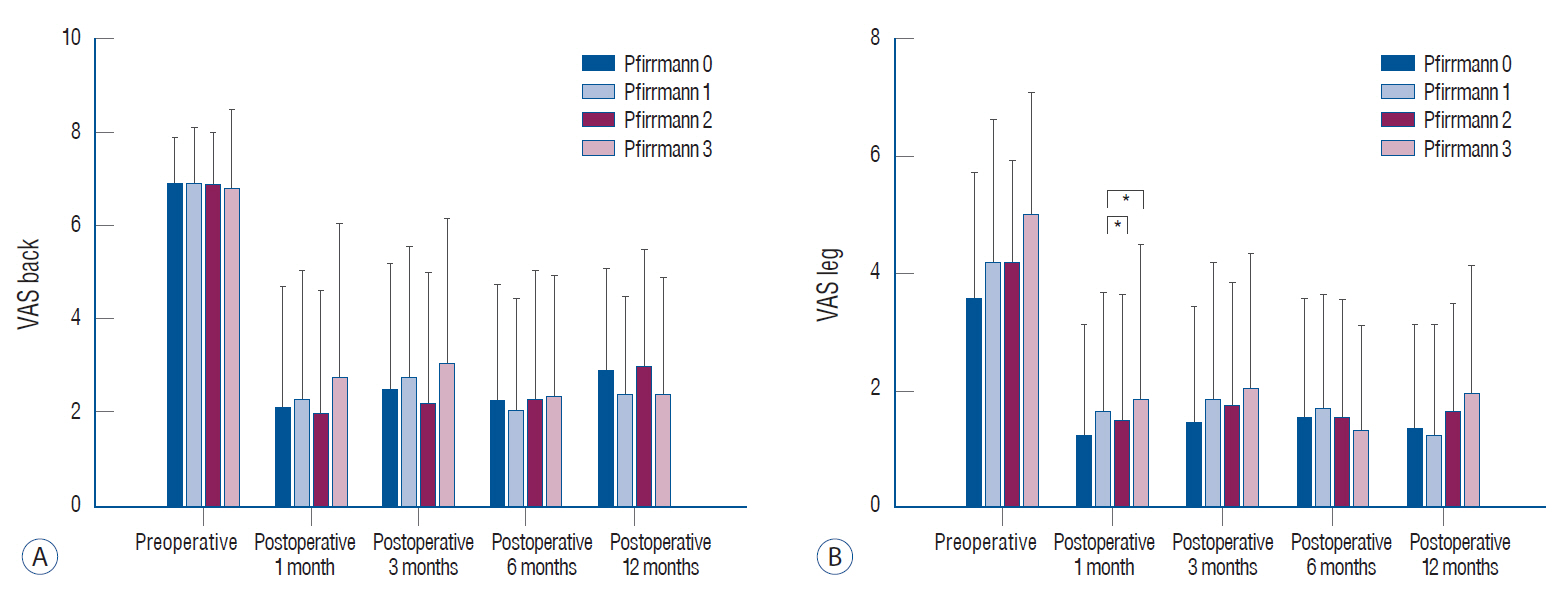
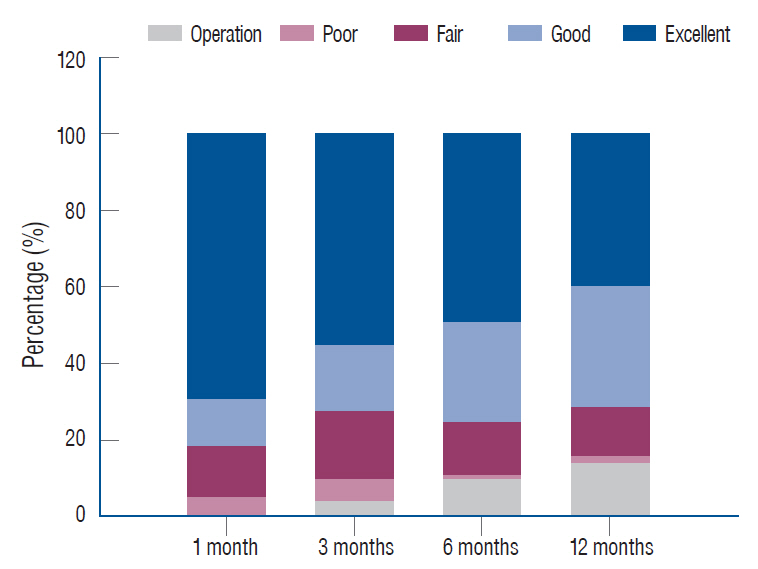
This study included 430 consecutive patients with single-level LDH who underwent PEN. Before treatment, the LDH type was categorized as bulging, protrusion, extrusion, and sequestration, while Pfirrmann grades were assigned according to imaging findings. Visual analog scale (VAS) scores for back and leg pain and success rates (Odom's criteria) were assessed at 1, 3, 6, and 12 months after treatment.
RESULTS
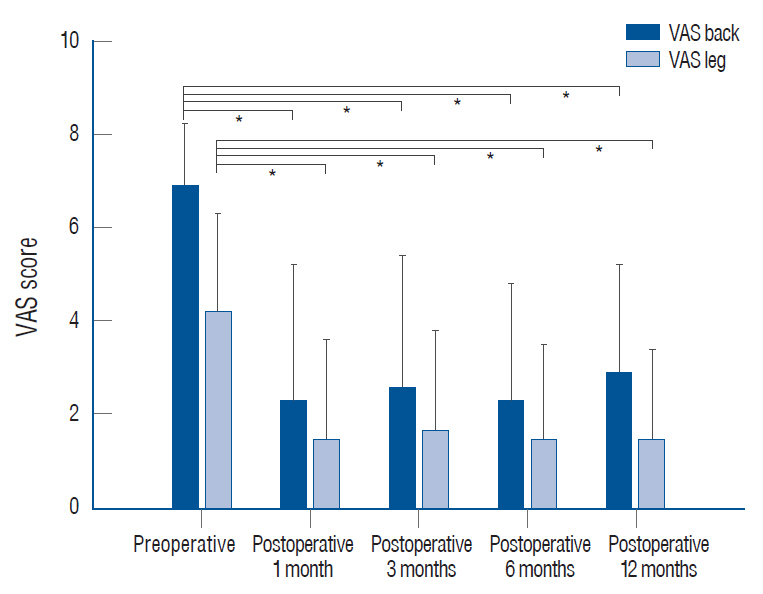
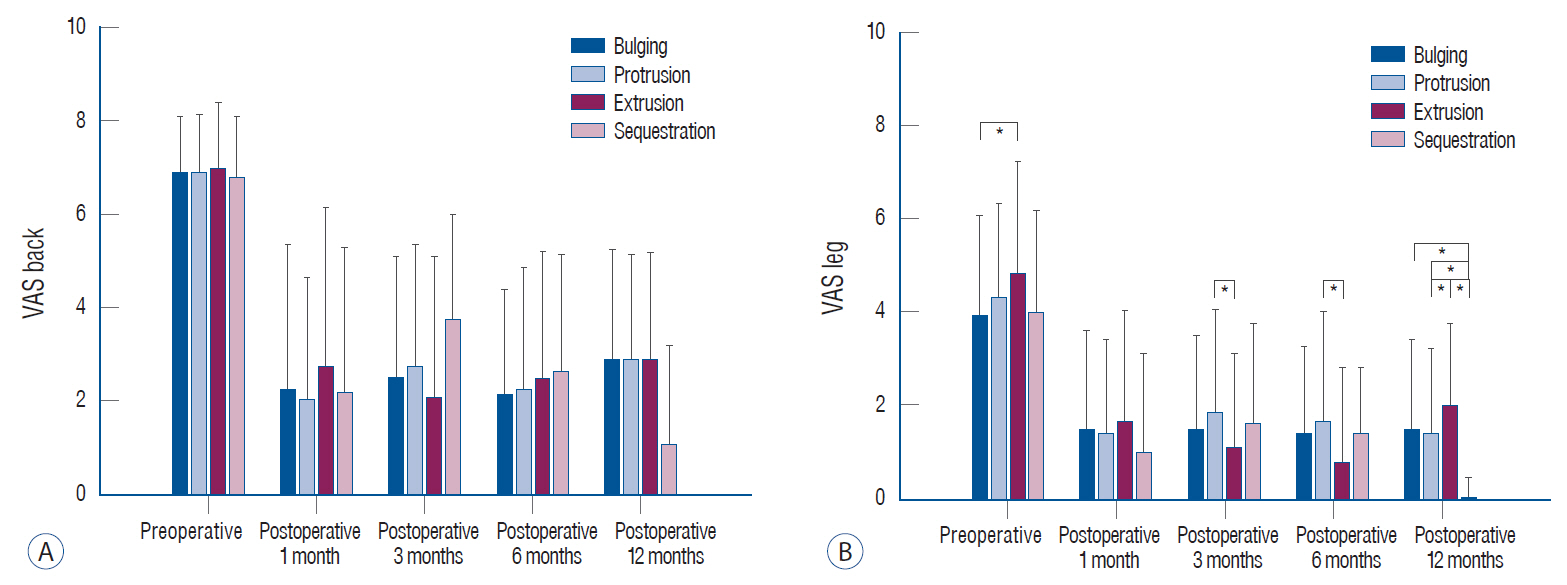
The mean preoperative VAS scores for back and leg pain were 6.90 and 4.23, respectively; these decreased after PEN as follows : 2.25 and 1.45, respectively, at 1 month; 2.61 and 1.68, respectively, at 3 months; 2.28 and 1.48, respectively, at 6 months; and 2.88 and 1.48, respectively, at 12 months (p<0.001). The decrease in VAS scores for leg pain was significantly greater in the extrusion and sequestration groups than in the other two groups (p<0.05); there were no other significant differences among groups. More than 70% patients exhibited good or excellent 12-month outcomes according to Odom's criteria. Subsequent surgery was required for 59 patients (13.7%), with a significantly higher rate in the extrusion (25.0%) and sequestration (30.0%) groups than in the bulging (7.3%) and protrusion (13.8%) groups (p<0.05). Nevertheless, subsequent surgery was not required for >70% patients with extrusion or sequestration. Patients with Pfirrmann grades 1-3 (14.0-21.5%) showed a significantly higher rate of subsequent surgery than those with Pfirrmann grade 0 (4.9%; p<0.05).
CONCLUSION
Our findings suggest that PEN is an effective treatment for back and leg pain caused by single-level LDH, with the outcomes remaining unaffected by the LDH type.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The role of percutaneous neurolysis in lumbar disc herniation: systematic review and meta-analysis
Laxmaiah Manchikanti, Emilija Knezevic, Nebojsa Nick Knezevic, Mahendra R. Sanapati, Alan D. Kaye, Srinivasa Thota, Joshua A. Hirsch
Korean J Pain. 2021;34(3):346-368. doi: 10.3344/kjp.2021.34.3.346.Comments on “The role of percutaneous neurolysis in lumbar disc herniation: systematic review and meta-analysis”
Min Cheol Chang
Korean J Pain. 2022;35(1):124-125. doi: 10.3344/kjp.2022.35.1.124.
Reference
-
References
1. Canale ST BJ. Campbell’s operative orthopaedics. Philadelphia: Elsevier;2003.2. Carey TS, Garrett JM, Jackman AM. Beyond the good prognosis. Examination of an inception cohort of patients with chronic low back pain. Spine (Phila Pa 1976). 25:115–120. 2000.3. Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. 85:102–108. 2003.4. Chopra P, Smith HS, Deer TR, Bowman RC. Role of adhesiolysis in the management of chronic spinal pain: a systematic review of effectiveness and complications. Pain Physician. 8:87–100. 2005.5. Epter RS, Helm S 2nd, Hayek SM, Benyamin RM, Smith HS, Abdi S. Systematic review of percutaneous adhesiolysis and management of chronic low back pain in post lumbar surgery syndrome. Pain Physician. 12:361–378. 2009.6. Franklin CVJ, Kalirathinam D, Palekar T, Nathani N. Effectiveness of PNF training for chronic low back pain. IOSR JNHS. 2:41–52. 2013.
Article7. Han YJ, Lee MN, Cho MJ, Park HJ, Moon DE, Kim YH. Contrast runoff correlates with the clinical outcome of cervical epidural neuroplasty using a racz catheter. Pain Physician. 19:E1035–E1040. 2016.8. Hayek SM, Helm S, Benyamin RM, Singh V, Bryce DA, Smith HS. Effectiveness of spinal endoscopic adhesiolysis in post lumbar surgery syndrome: a systematic review. Pain Physician. 12:419–435. 2009.9. Heavner JE, Racz GB, Raj P. Percutaneous epidural neuroplasty: prospective evaluation of 0.9% NaCl versus 10% NaCl with or without hyaluronidase. Reg Anesth Pain Med. 24:202–207. 1999.
Article10. Helm Ii S, Benyamin RM, Chopra P, Deer TR, Justiz R. Percutaneous adhesiolysis in the management of chronic low back pain in post lumbar surgery syndrome and spinal stenosis: a systematic review. Pain Physician. 15:E435–E462. 2012.11. Ji GY, Oh CH, Moon B, Choi SH, Shin DA, Yoon YS, et al. Efficacy of percutaneous epidural neuroplasty does not correlate with dural sac cross-sectional area in single level disc disease. Yonsei Med J. 56:691–697. 2015.
Article12. Lee JH, Lee SH. Clinical effectiveness of percutaneous adhesiolysis using Navicath for the management of chronic pain due to lumbosacral disc herniation. Pain Physician. 15:213–221. 2012.13. Manchikanti L, Bakhit CE. Percutaneous lysis of epidural adhesions. Pain Physician. 3:46–64. 2000.
Article14. Manchikanti L, Boswell MV, Datta S, Fellows B, Abdi S, Singh V, et al. Comprehensive review of therapeutic interventions in managing chronic spinal pain. Pain Physician. 12:E123–E198. 2009.15. Manchikanti L, Boswell MV, Singh V, Benyamin RM, Fellows B, Abdi S, et al. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 12:699–802. 2009.16. Manchikanti L, Cash KA, McManus CD, Pampati V, Singh V, Benyamin R. The preliminary results of a comparative effectiveness evaluation of adhesiolysis and caudal epidural injections in managing chronic low back pain secondary to spinal stenosis: a randomized, equivalence controlled trial. Pain Physician. 12:E341–E354. 2009.17. Manchikanti L, Manchikanti KN, Gharibo CG, Kaye AD. Efficacy of percutaneous adhesiolysis in the treatment of lumbar post surgery syndrome. Anesth Pain Med. 6:e26172. 2016.
Article18. Manchikanti L, Pampati V, Fellows B, Rivera J, Beyer CD, Damron KS. Role of one day epidural adhesiolysis in management of chronic low back pain: a randomized clinical trial. Pain Physician. 4:153–166. 2001.19. Manchikanti L, Pampati V, Fellows B, Rivera JJ, Damron KS, Beyer C, et al. Effectiveness of percutaneous adhesiolysis with hypertonic saline neurolysis in refractory spinal stenosis. Pain Physician. 4:366–373. 2001.20. Manchikanti L, Singh V, Bakhit CE, Fellows B. Interventional techniques in the management of chronic pain: part 1.0. Pain Physician. 3:7–42. 2000.21. Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. A comparative effectiveness evaluation of percutaneous adhesiolysis and epidural steroid injections in managing lumbar post surgery syndrome: a randomized, equivalence controlled trial. Pain Physician. 12:E355–E368. 2009.22. Manchikanti L, Staats PS, Singh V, Schultz DM, Vilims BD, Jasper JF, et al. Evidence-based practice guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 6:3–81. 2003.23. Oh CH, Ji GY, Cho PG, Choi WS, Shin DA, Kim KN, et al. The catheter tip position and effects of percutaneous epidural neuroplasty in patients with lumbar disc disease during 6-months of follow-up. Pain Physician. 17:E599–E608. 2014.24. Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 356:2245–2256. 2007.
Article25. Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 230:583–588. 2004.
Article26. Splendiani A, Puglielli E, De Amicis R, Barile A, Masciocchi C, Gallucci M. Spontaneous resolution of lumbar disk herniation: predictive signs for prognostic evaluation. Neuroradiology. 46:916–922. 2004.
Article27. Taheri A, Khajenasiri AR, Nazemian Yazdi NA, Safari S, Sadeghi J, Hatami M. Clinical evaluation of percutaneous caudal epidural adhesiolysis with the racz technique for low back pain due to contained disc herniation. Anesth Pain Med. 6:e26749. 2016.
Article28. Trainor TJ, Wiesel SW. Epidemiology of back pain in the athlete. Clin Sports Med. 21:93–103. 2002.
Article29. Trescot AM, Chopra P, Abdi S, Datta S, Schultz DM. Systematic review of effectiveness and complications of adhesiolysis in the management of chronic spinal pain: an update. Pain Physician. 10:129–146. 2007.30. Veihelmann A, Devens C, Trouillier H, Birkenmaier C, Gerdesmeyer L, Refior HJ. Epidural neuroplasty versus physiotherapy to relieve pain in patients with sciatica: a prospective randomized blinded clinical trial. J Orthop Sci. 11:365–369. 2006.
Article31. Viesca CO, Racz GB, Day MR. Special techniques in pain management: lysis of adhesions. Anesthesiol Clin North Am. 21:745–766. vi. 2003.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Percutaneous Epidural Neuroplasty Does Not Correlate with Dural Sac Cross-Sectional Area in Single Level Disc Disease
- Lumbar Epidural Venography in the Diagnosis of Lumbar Disc Herniation
- Percutaneous epidural balloon neuroplasty: a narrative review of current evidence
- Acute Motor Weakness of Opposite Lower Extremity after Percutaneous Epidural Neuroplasty
- Clinical Outcomes of Epidural Neuroplasty for Cervical Disc Herniation