J Korean Ophthalmol Soc.
2019 Nov;60(11):1037-1042. 10.3341/jkos.2019.60.11.1037.
Dry Eye Syndrome and Morphological Changes of Meibomian Glands in Type 2 Diabetic Patients
- Affiliations
-
- 1Department of Ophthalmology, Ewha Womans University College of Medicine, Seoul, Korea. jrmoph@ewha.ac.kr
- KMID: 2463353
- DOI: http://doi.org/10.3341/jkos.2019.60.11.1037
Abstract
- PURPOSE
To evaluate the morphological changes of meibomian glands and dry eye syndrome in patients with type II diabetes.
METHODS
The medical records of 72 diabetic patients referred to the ophthalmology clinic for the evaluation of diabetic retinopathy, who had dry eye symptoms, were retrospectively reviewed.
RESULTS
A total of 72 patients, with an age of 56.3 ± 13.3 years, were analyzed. The group with diabetic retinopathy (52 patients) had a significantly lower tear film break-up time (p = 0.046), lower Schirmer's test value (p = 0.005), and higher percentage of upper (p = 0.036) and lower (p = 0.017) meibomian gland area losses than the group without diabetic retinopathy (20 patients). According to multilinear regression analyses considering sex, age, and diabetes-related characteristics, the Schirmer's test value was significantly lower with increasing stage of diabetic retinopathy (β = −1.180, p = 0.016). The percentage of upper meibomian gland area loss was significantly increased with increasing age (β = 0.605, p < 0.001), glycosylated hemoglobin (β = 1.881, p = 0.011), and stage of diabetic retinopathy (β = 4.458, p = 0.001). The percentage of lower meibomian gland loss area was significantly increased with increasing age (β = 0.443, p = 0.001) and stage of diabetic retinopathy (β = 4.879, p = 0.001).
CONCLUSIONS
In patients with type 2 diabetes, the more severe the diabetic retinopathy, the more likely the meibomian gland loss will occur, so careful and appropriate treatment should be conducted.
MeSH Terms
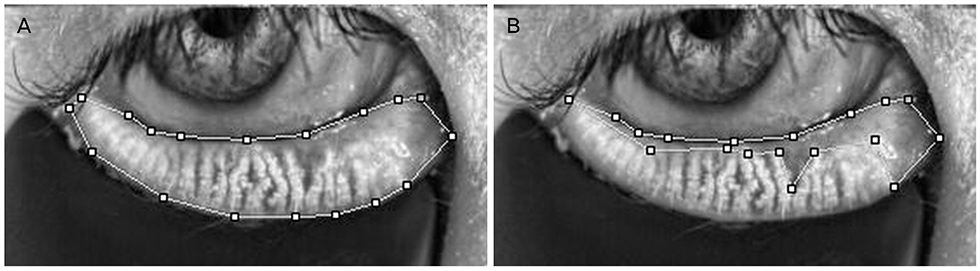
Figure
Reference
-
1. Yu T, Shi WY, Song AP, et al. Changes of meibomian glands in patients with type 2 diabetes mellitus. Int J Ophthalmol. 2016; 9:1740–1744.2. Yoon KC, Im SK, Seo MS. Changes of tear film and ocular surface in diabetes mellitus. Korean J Ophthalmol. 2004; 18:168–174.
Article3. Lin X, Xu B, Zheng Y, et al. Meibomian gland dysfunction in type 2 diabetic patients. J Ophthalmol. 2017; 2017:3047867.4. Dogru M, Katakami C, Inoue M. Tear function and ocular surface changes in noninsulin-dependent diabetes mellitus. Ophthalmology. 2001; 108:586–592.
Article5. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:75–92.6. Manaviat MR, Rashidi M, Afkhami-Ardekani M, Shoja MR. Prevalence of dry eye syndrome and diabetic retinopathy in type 2 diabetic patients. BMC Ophthalmol. 2008; 8:10.7. Hom M, De Land P. Self-reported dry eyes and diabetic history. Optometry. 2006; 77:554–558.
Article8. Zhang X, Zhao L, Deng S, et al. Dry eye syndrome in patients with diabetes mellitus: prevalence, etiology, and clinical characteristics. J Ophthalmol. 2016; 2016:8201053.9. Najafi L, Malek M, Valojerdi AE, et al. Dry eye disease in type 2 diabetes mellitus; comparison of the tear osmolarity test with other common diagnostic tests: a diagnostic accuracy study using STARD standard. J Diabetes Metab Disord. 2015; 14:39.
Article10. Kang WS, Choi HT, Ahn M, You IC. The change of tear film in classification of diabetic retinopathy. J Korean Ophthalmol Soc. 2014; 55:486–492.11. Shamsheer RP, Arunachalam C. A clinical study of meibomian gland dysfunction in patients with diabetes. Middle East Afr J of Ophthalmol. 2015; 22:462–466.12. Schultz RO, Matsuda M, Yee RW, et al. Corneal endothelial changes in type I and type II diabetes mellitus. Am J Ophthalmol. 1984; 98:401–410.13. Friend J, Thoft RA. The diabetic cornea. Int Ophthalmol Clin. 1984; 24:111–123.
Article14. Schultz RO, Van Horn DL, Peters MA, et al. Diabetic keratopathy. Trans Am Ophthalmol Soc. 1981; 79:180–199.15. Misra SL, Braatvedt GD, Patel DV. Impact of diabetes mellitus on the ocular surface: a review. Clin Exp Ophthalmol. 2016; 44:278–288.
Article16. DeMill DL, Hussain M, Pop-Busui R, Shtein RM. Ocular surface disease in patients with diabetic peripheral neuropathy. Br J Ophthalmol. 2016; 100:924–928.17. Misra SL, Patel DV, McGhee CN, et al. Peripheral neuropathy and tear film dysfunction in type 1 diabetes mellitus. J Diabetes Res. 2014; 2014:848659.
Article18. Herse PR. A review of manifestations of diabetes mellitus in the anterior eye and cornea. Am J Optom Physiol Opt. 1988; 65:224–230.19. Shih KC, Lam KS, Tong L. A systematic review on the impact of diabetes mellitus on the ocular surface. Nutr Diabetes. 2017; 7:e251.
Article20. Alves Mde C, Carvalheira JB, Módulo CM, Rocha EM. Tear film and ocular surface changes in diabetes mellitus. Arq Bras Oftalmol. 2008; 71(6 Suppl):96–103.21. Seifart U, Strempel I. The dry eye and diabetes mellitus. Ophthalmologe. 1994; 91:235–239.22. Ozdemir M, Buyukbese MA, Cetinkaya A, Ozdemir G. Risk factors for ocular surface disorders in patients with diabetes mellitus. Diabetes Res Clin Pract. 2003; 59:195–199.23. Ding J, Liu Y, Sullivan DA. Effects of insulin and high glucose on human meibomian gland epithelial cells. Invest Ophthalmol Vis Sci. 2015; 56:7814–7820.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CCL4 Concentration in Tears of Dry Eye Patients and Its Correlation With Tear Surface Parameters
- Diagnosis and treatment of dry eye syndrome
- Assessment of Meibomian Gland Dysfunction and Comparison of The Results of BUT and Schirmer Test According to Meibomian Gland State
- Clinical Analysis of Dry Eye Syndrome According to Anterior Displacement of the Marx Line
- Association between Dry Eye Questionnaires and Dry Eye Sign in Meibomian Gland Dysfunction