Clin Orthop Surg.
2019 Sep;11(3):282-290. 10.4055/cios.2019.11.3.282.
Clinical and Radiological Changes after Microfracture of Knee Chondral Lesions in Middle-Aged Asian Patients
- Affiliations
-
- 1Department of Orthopedic Surgery, Hanil Hospital, Seoul, Korea.
- 2Department of Orthopedic Surgery, Suvekchya International Hospital, Kathmandu, Nepal.
- 3Department of Orthopedic Surgery, Gwangmyeong Sungae Hospital, Gwangmyeong, Korea.
- 4Department of Orthopedic Surgery, Seoul National University College of Medicine, Seoul, Korea. oshawks7@snu.ac.kr
- KMID: 2462556
- DOI: http://doi.org/10.4055/cios.2019.11.3.282
Abstract
- BACKGROUND
Although microfracture is widely accepted as an effective treatment option for knee chondral lesions, little is known about the deterioration of clinical outcomes and radiological progression in middle-aged patients. Therefore, this study was conducted to evaluate the clinical and radiological changes after microfracture of knee chondral lesions in middle-aged Asian patients.
METHODS
A total of 71 patients were included in the study. They were between the ages of 40 and 60 years and underwent arthroscopic microfracture for localized full-thickness cartilage defects of the knee from January 2000 to September 2015. The recovery status of chondral lesions was assessed by using the magnetic resonance observation of cartilage repair tissue (MOCART) score in postoperative magnetic resonance imaging (MRI). Clinical and radiological results were reviewed, and survival rate with conversion to arthroplasty or osteotomy as an end point was evaluated.
RESULTS
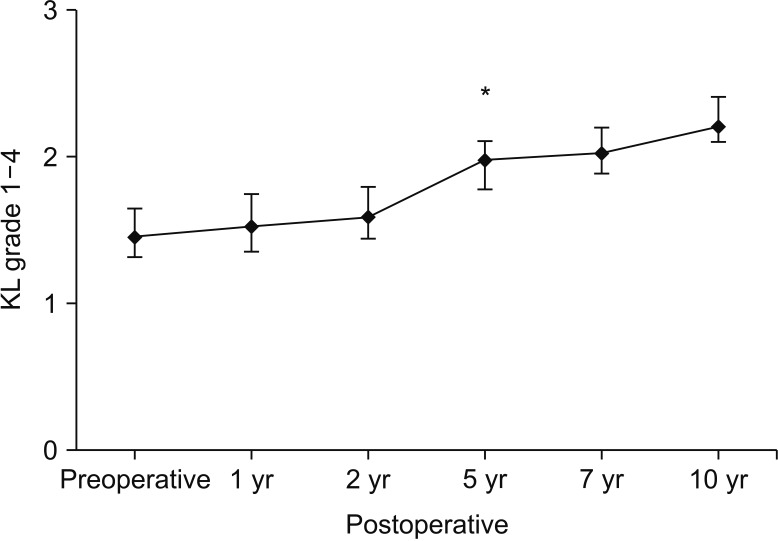
The mean age of the patients at surgery was 51.3 ± 4.7 years (range, 40 to 60 years), and the mean follow-up period was 7.2 ± 2.6 years (range, 1.0 to 17.4 years). The MOCART scores of 32 patients at mean postoperative 2.1 years showed three cases (9%) of full recovery, two cases (7%) of hyperplastic recovery, 23 cases (70%) with more than 50% filling, and four cases (14%) with less than 50% filling. Clinical scores improved significantly at 1 year after surgery (p < 0.05); however, the scores deteriorated over time after postoperative 1 year, and the mean values reached preoperative levels at postoperative 10 years. Significant radiological progression of arthritis (Kellgren-Lawrence grade) was observed at 5 years after surgery. Four patients underwent total knee arthroplasty during follow-up.
CONCLUSIONS
Most patients showed more than 50% of defect filling at 2 years after surgery on MRI. Clinical results of microfracture of knee chondral lesion showed the best improvement at postoperative 1 year but gradually worsened thereafter until postoperative 10 years. Radiological progression of arthritis was observed from 5 years after surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Rodrigo JJ. Improvement of full-thickness chondral defect healing in the human knee after debridement and microfracture using continuous passive motion. Am J Knee Surg. 1994; 7:109–116.2. Steadman JR, Rodkey WG, Briggs KK. Microfracture to treat full-thickness chondral defects: surgical technique, rehabilitation, and outcomes. J Knee Surg. 2002; 15(3):170–176. PMID: 12152979.3. Knutsen G, Drogset JO, Engebretsen L, et al. A randomized trial comparing autologous chondrocyte implantation with microfracture: findings at five years. J Bone Joint Surg Am. 2007; 89(10):2105–2112. PMID: 17908884.4. Kreuz PC, Erggelet C, Steinwachs MR, et al. Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy. 2006; 22(11):1180–1186. PMID: 17084294.
Article5. Krych AJ, Harnly HW, Rodeo SA, Williams RJ 3rd. Activity levels are higher after osteochondral autograft transfer mosaicplasty than after microfracture for articular cartilage defects of the knee: a retrospective comparative study. J Bone Joint Surg Am. 2012; 94(11):971–978. PMID: 22637203.6. Kraeutler MJ, Belk JW, Purcell JM, McCarty EC. Microfracture versus autologous chondrocyte implantation for articular cartilage lesions in the knee: a systematic review of 5-year outcomes. Am J Sports Med. 2018; 46(4):995–999. PMID: 28423287.
Article7. Gobbi A, Karnatzikos G, Kumar A. Long-term results after microfracture treatment for full-thickness knee chondral lesions in athletes. Knee Surg Sports Traumatol Arthrosc. 2014; 22(9):1986–1996. PMID: 24051505.
Article8. Harris JD, Siston RA, Pan X, Flanigan DC. Autologous chondrocyte implantation: a systematic review. J Bone Joint Surg Am. 2010; 92(12):2220–2233. PMID: 20844166.9. Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG. Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy. 2003; 19(5):477–484. PMID: 12724676.
Article10. Bae DK, Song SJ, Yoon KH, Heo DB, Kim TJ. Survival analysis of microfracture in the osteoarthritic knee-minimum 10-year follow-up. Arthroscopy. 2013; 29(2):244–250. PMID: 23369477.
Article11. Miller BS, Steadman JR, Briggs KK, Rodrigo JJ, Rodkey WG. Patient satisfaction and outcome after microfracture of the degenerative knee. J Knee Surg. 2004; 17(1):13–17. PMID: 14971668.
Article12. Weber AE, Locker PH, Mayer EN, et al. Clinical outcomes after microfracture of the knee: midterm follow-up. Orthop J Sports Med. 2018; 6(2):2325967117753572. PMID: 29450208.
Article13. Lee JJ, Lee SJ, Lee TJ, Yoon TH, Choi CH. Results of microfracture in the osteoarthritic knee with focal full-thickness articular cartilage defects and concomitant medial meniscal tears. Knee Surg Relat Res. 2013; 25(2):71–76. PMID: 23741702.
Article14. Mithoefer K, Venugopal V, Manaqibwala M. Incidence, degree, and clinical effect of subchondral bone overgrowth after microfracture in the knee. Am J Sports Med. 2016; 44(8):2057–2063. PMID: 27190069.
Article15. Mor A, Grijota M, Norgaard M, et al. Trends in arthroscopy-documented cartilage injuries of the knee and repair procedures among 15-60-year-old patients. Scand J Med Sci Sports. 2015; 25(4):e400–e407. PMID: 25262959.
Article16. Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG. Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy. 1997; 13(4):456–460. PMID: 9276052.
Article17. Hjelle K, Solheim E, Strand T, Muri R, Brittberg M. Articular cartilage defects in 1,000 knee arthroscopies. Arthroscopy. 2002; 18(7):730–734. PMID: 12209430.
Article18. Deshpande BR, Katz JN, Solomon DH, et al. Number of persons with symptomatic knee osteoarthritis in the US: impact of race and ethnicity, age, sex, and obesity. Arthritis Care Res (Hoboken). 2016; 68(12):1743–1750. PMID: 27014966.
Article19. Thambyah A, Goh JC, De SD. Contact stresses in the knee joint in deep flexion. Med Eng Phys. 2005; 27(4):329–335. PMID: 15823474.
Article20. Friedrich KM, Mamisch TC, Plank C, et al. Diffusion-weighted imaging for the follow-up of patients after matrixassociated autologous chondrocyte transplantation. Eur J Radiol. 2010; 73(3):622–628. PMID: 19181469.
Article21. Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009; 37(5):890–897. PMID: 19261899.22. Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011; 63(Suppl 11):S208–S228. PMID: 22588746.23. Frisbie DD, Trotter GW, Powers BE, et al. Arthroscopic subchondral bone plate microfracture technique augments healing of large chondral defects in the radial carpal bone and medial femoral condyle of horses. Vet Surg. 1999; 28(4):242–255. PMID: 10424704.
Article24. Miller BS, Briggs KK, Downie B, Steadman JR. Clinical outcomes following the microfracture procedure for chondral defects of the knee: a longitudinal data analysis. Cartilage. 2010; 1(2):108–112. PMID: 26069541.25. Goyal D, Keyhani S, Lee EH, Hui JH. Evidence-based status of microfracture technique: a systematic review of level I and II studies. Arthroscopy. 2013; 29(9):1579–1588. PMID: 23992991.
Article26. Mithoefer K, Williams RJ 3rd, Warren RF, et al. The microfracture technique for the treatment of articular cartilage lesions in the knee: a prospective cohort study. J Bone Joint Surg Am. 2005; 87(9):1911–1920. PMID: 16140804.27. Mithoefer K, Williams RJ 3rd, Warren RF, Wickiewicz TL, Marx RG. High-impact athletics after knee articular cartilage repair: a prospective evaluation of the microfracture technique. Am J Sports Med. 2006; 34(9):1413–1418. PMID: 16735588.28. Mithoefer K, McAdams T, Williams RJ, Kreuz PC, Mandelbaum BR. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med. 2009; 37(10):2053–2063. PMID: 19251676.29. Gill TJ, McCulloch PC, Glasson SS, Blanchet T, Morris EA. Chondral defect repair after the microfracture procedure: a nonhuman primate model. Am J Sports Med. 2005; 33(5):680–685. PMID: 15722269.30. de Windt TS, Welsch GH, Brittberg M, et al. Is magnetic resonance imaging reliable in predicting clinical outcome after articular cartilage repair of the knee?: a systematic review and meta-analysis. Am J Sports Med. 2013; 41(7):1695–1702. PMID: 23364897.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microfracture Surgery for Cartilage Regeneration in Degenerative Arthritis of the Knee
- Results of Microfracture Surgery in Osteoarthritic Knee
- Management of Focal Chondral Lesion in the Knee Joint
- A Comparison of Clinical Outcomes after Osteochondral Autologous Transplantation & Arthroscopic Microfracture Surgery for Treating of Osteochondral Lesions of the Knee
- Results of Microfracture in the Osteoarthritic Knee with Focal Full-Thickness Articular Cartilage Defects and Concomitant Medial Meniscal Tears