Clin Orthop Surg.
2019 Sep;11(3):270-274. 10.4055/cios.2019.11.3.270.
Isolated Acetabular Liner Exchange for Polyethylene Wear and Osteolysis with Well-Fixed Metal Shell
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul National University Hospital, Seoul, Korea. oskim@snu.ac.kr
- KMID: 2462554
- DOI: http://doi.org/10.4055/cios.2019.11.3.270
Abstract
- BACKGROUND
The isolated liner and head exchange procedure has been an established treatment method for polyethylene wear and osteolysis when the acetabular component remains well fixed. In this study, the mid-term results of this procedure were evaluated retrospectively.
METHODS
Among the consecutive patients operated on from September 1995, two patients (three hips) were excluded because of inadequate follow-up, and the results of remaining 34 patients (34 hips) were evaluated. There were 20 men and 14 women with a mean age of 49 years. A conventional polyethylene liner was used in 26 cases and a highly cross-linked polyethylene liner was used in eight cases. In three cases, the liner was cemented in a metal shell because a compatible liner could not be used.
RESULTS
After a follow-up of 5 to 20.2 years, re-revision surgery was necessary in 10 cases (29.4%): in eight for wear and osteolysis at 55 to 101 months after liner exchange and in two for acetabular loosening at 1 and 1.5 years after liner exchange. Re-revision surgery included all component revision (four cases), cup revision (four cases), and liner exchange (two cases). In all re-revision cases, a conventional polyethylene liner was used initially. There was no failure in the cases in which a highly cross-linked polyethylene liner was used.
CONCLUSIONS
The results of this study suggest that isolated acetabular liner exchange is a reasonable option for wear and osteolysis when the metal shell is well fixed. More promising long-term results are expected with the use of highly cross-linked polyethylene liners.
Keyword
MeSH Terms
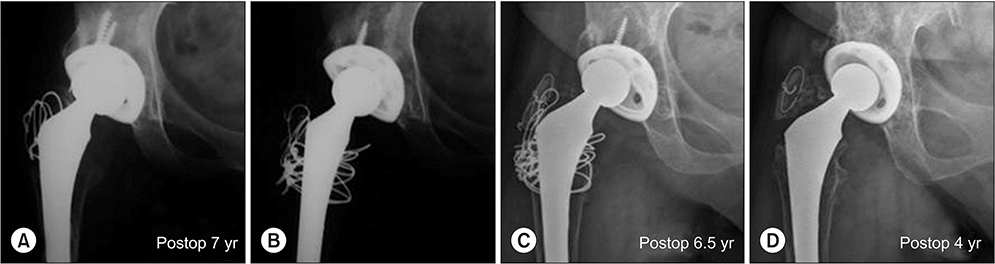
Figure
Reference
-
1. Restrepo C, Ghanem E, Houssock C, Austin M, Parvizi J, Hozack WJ. Isolated polyethylene exchange versus acetabular revision for polyethylene wear. Clin Orthop Relat Res. 2009; 467(1):194–198.
Article2. Chiang PP, Burke DW, Freiberg AA, Rubash HE. Osteolysis of the pelvis: evaluation and treatment. Clin Orthop Relat Res. 2003; (417):164–174.3. Hamilton WG, Hopper RH Jr, Engh CA Jr, Engh CA. Survivorship of polyethylene liner exchanges performed for the treatment of wear and osteolysis among porous-coated cups. J Arthroplasty. 2010; 25:6 Suppl. 75–80.
Article4. Lombardi AV Jr, Berend KR. Isolated acetabular liner exchange. J Am Acad Orthop Surg. 2008; 16(5):243–248.
Article5. Maloney WJ, Paprosky W, Engh CA, Rubash H. Surgical treatment of pelvic osteolysis. Clin Orthop Relat Res. 2001; (393):78–84.
Article6. Naudie DD, Engh CA Sr. Surgical management of polyethylene wear and pelvic osteolysis with modular uncemented acetabular components. J Arthroplasty. 2004; 19:4 Suppl 1. 124–129.
Article7. Schmalzried TP, Fowble VA, Amstutz HC. The fate of pelvic osteolysis after reoperation: no recurrence with lesional treatment. Clin Orthop Relat Res. 1998; (350):128–137.
Article8. Schmalzried TP, Guttmann D, Grecula M, Amstutz HC. The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am. 1994; 76(5):677–688.
Article9. Deheshi BM, Allen DJ, Kim PR. Treatment of retroacetabular osteolysis with calcium sulfate and retention of original components. J Arthroplasty. 2008; 23(8):1240.e9–1240.e12.
Article10. Etienne G, Ragland PS, Mont MA. Use of cancellous bone chips and demineralized bone matrix in the treatment of acetabular osteolysis: preliminary 2-year follow-up. Orthopedics. 2004; 27:1 Suppl. s123–s126.
Article11. Griffin WL, Fehring TK, Mason JB, McCoy TH, Odum S, Terefenko CS. Early morbidity of modular exchange for polyethylene wear and osteolysis. J Arthroplasty. 2004; 19:7 Suppl 2. 61–66.
Article12. Haidukewych GJ. Osteolysis in the well-fixed socket: cup retention or revision? J Bone Joint Surg Br. 2012; 94:11 Suppl A. 65–69.13. Maloney WJ, Herzwurm P, Paprosky W, Rubash HE, Engh CA. Treatment of pelvic osteolysis associated with a stable acetabular component inserted without cement as part of a total hip replacement. J Bone Joint Surg Am. 1997; 79(11):1628–1634.
Article14. Stamenkov R, Neale SD, Kane T, Findlay DM, Taylor DJ, Howie DW. Cemented liner exchange with bone grafting halts the progression of periacetabular osteolysis. J Arthroplasty. 2014; 29(4):822–826.
Article15. Walmsley DW, Waddell JP, Schemitsch EH. Isolated head and liner exchange in revision hip arthroplasty. J Am Acad Orthop Surg. 2017; 25(4):288–296.
Article16. Adelani MA, Mall NA, Nyazee H, Clohisy JC, Barrack RL, Nunley RM. Revision total hip arthroplasty with retained acetabular component. J Bone Joint Surg Am. 2014; 96(12):1015–1020.
Article17. Beaule PE, Le Duff MJ, Dorey FJ, Amstutz HC. Fate of cementless acetabular components retained during revision total hip arthroplasty. J Bone Joint Surg Am. 2003; 85(12):2288–2293.
Article18. Terefenko KM, Sychterz CJ, Orishimo K, Engh CA Sr. Polyethylene liner exchange for excessive wear and osteolysis. J Arthroplasty. 2002; 17(6):798–804.
Article19. Ilchmann T, Mjoberg B, Wingstrand H. Measurement accuracy in acetabular cup wear: three retrospective methods compared with Roentgen stereophotogrammetry. J Arthroplasty. 1995; 10(5):636–642.20. Mehin R, Yuan X, Haydon C, et al. Retroacetabular osteolysis: when to operate? Clin Orthop Relat Res. 2004; (428):247–255.21. Suh DH, Han SB, Yun HH, Chun SK, Shon WY. Characterization of progression of pelvic osteolysis after cementless total hip arthroplasty: computed tomographic study. J Arthroplasty. 2013; 28(10):1851–1855.
Article22. Boucher HR, Lynch C, Young AM, Engh CA Jr, Engh C Sr. Dislocation after polyethylene liner exchange in total hip arthroplasty. J Arthroplasty. 2003; 18(5):654–657.
Article23. Lie SA, Hallan G, Furnes O, Havelin LI, Engesaeter LB. Isolated acetabular liner exchange compared with complete acetabular component revision in revision of primary uncemented acetabular components: a study of 1649 revisions from the Norwegian Arthroplasty Register. J Bone Joint Surg Br. 2007; 89(5):591–594.24. O'Brien JJ, Burnett RS, McCalden RW, MacDonald SJ, Bourne RB, Rorabeck CH. Isolated liner exchange in revision total hip arthroplasty: clinical results using the direct lateral surgical approach. J Arthroplasty. 2004; 19(4):414–423.25. Egawa H, Ho H, Huynh C, Hopper RH Jr, Engh CA Jr, Engh CA. A three-dimensional method for evaluating changes in acetabular osteolytic lesions in response to treatment. Clin Orthop Relat Res. 2010; 468(2):480–490.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short Term Results of Cementation of a Polyethylene Liner into a Well-Fixed Metal Shell
- Dissociation of Polyethylene liner in Metal backed Cup without Hip Dislocation History: A Case Report
- Late dissociation of the polyethylene liner from a modular acetabular metal shell after primary total hip arthroplasty: a report of five cases
- Treatment of Pelvic Osteolysis with a stable Cementless Acetabular Cup with Exchange of Polyethlene Liner and Morselized Bone Graft
- A Study for The Conformity Between Polyethylene Liner and Metal Backing Cup in THR