J Korean Assoc Oral Maxillofac Surg.
2019 Oct;45(5):276-284. 10.5125/jkaoms.2019.45.5.276.
The effect of fixation plate use on bone healing during the reconstruction of mandibular defects
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Gangneung-Wonju National University, Gangneung, Korea. ywpark@gwnu.ac.kr
- KMID: 2461480
- DOI: http://doi.org/10.5125/jkaoms.2019.45.5.276
Abstract
OBJECTIVES
This study sought to compare efficiency results between the use of a customized implant (CI) and a reconstruction plate (RP) in mandibular defect reconstruction in an animal model.
MATERIALS AND METHODS
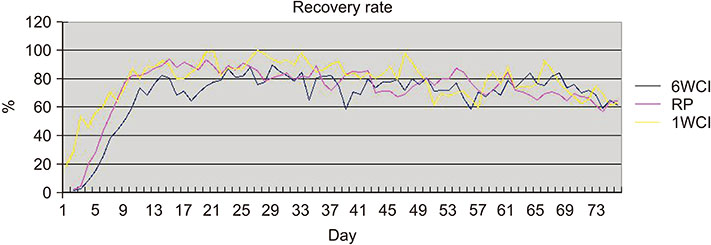
Fifteen rabbits underwent surgery to create a defect in the right side of the mandible and were randomly divided into two groups. For reconstruction of the mandibular defect, the RP group (n=5) received five-hole mini-plates without bone grafting and the CI group (n=10) received fabricated CIs based on the cone-beam computed tomography (CBCT) data taken preoperatively. The CI group was further divided into two subgroups depending on the time of CBCT performance preoperatively, as follows: a six-week CI (6WCI) group (n=5) and a one-week CI (1WCI) group (n=5). Daily food intake amount (DFIA) was measured to assess the recovery rate. Radiographic images were acquired to evaluate screw quantity. CBCT and histological examination were performed in the CI subgroup after sacrifice.
RESULTS
The 1WCI group showed the highest value in peak average recovery rate and the fastest average recovery rate. In terms of reaching a 50% recovery rate, the 1WCI group required the least number of days as compared with the other groups (2.6±1.3 days), while the RP group required the least number of days to reach an 80% recovery rate (7.8±2.2 days). The 1WCI group showed the highest percentage of intact screws (94.3%). New bone formation was observed in the CI group during histological examination.
CONCLUSION
Rabbits with mandibular defects treated with CI showed higher and faster recovery rates and more favorable screw status as compared with those treated with a five-hole mini-plate without bone graft.
Keyword
MeSH Terms
Figure
Reference
-
1. Standring S. Gray's anatomy: the anatomical basis of clinical practice. 40th ed. London: Churchill Livingstone;2008.2. Genden EM, Kessler SM. Reconstruction of the head and neck: a defect-oriented approach. New York: Thieme;2012.3. Rachmiel A, Shilo D, Blanc O, Emodi O. Reconstruction of complex mandibular defects using integrated dental custom-made titanium implants. Br J Oral Maxillofac Surg. 2017; 55:425–427.
Article4. Millard DR Jr, Deane M, Garst WP. Bending an iliac bone graft for anterior mandibular arch repair. Plast Reconstr Surg. 1971; 48:600–602.
Article5. Blocker TG Jr, Stout RA. Mandibular reconstruction, World War II. Plast Reconstr Surg (1946). 1949; 4:153–156.
Article6. Ostrup LT, Fredrickson JM. Reconstruction of mandibular defects after radiation, using a free, living bone graft transferred by microvascular anastomose. An experimental study. Plast Reconstr Surg. 1975; 55:563–572.7. Hidalgo DA. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg. 1989; 84:71–79.8. Kim JW, Hwang JH, Ahn KM. Fibular flap for mandible reconstruction in osteoradionecrosis of the jaw: selection criteria of fibula flap. Maxillofac Plast Reconstr Surg. 2016; 38:46.
Article9. Goh BT, Lee S, Tideman H, Stoelinga PJ. Mandibular reconstruction in adults: a review. Int J Oral Maxillofac Surg. 2008; 37:597–605.
Article10. Mücke T, Müller AA, Kansy K, Hallermann W, Kerkmann H, Schuck N, et al. Microsurgical reconstruction of the head and neck--Current practice of maxillofacial units in Germany, Austria, and Switzerland. J Craniomaxillofac Surg. 2011; 39:449–452.
Article11. Chow JM, Hill JH. Primary mandibular reconstruction using the AO reconstruction plate. Laryngoscope. 1986; 96:768–773.
Article12. Saunders JR Jr, Hirata RM, Jaques DA. Definitive mandibular replacement using reconstruction plates. Am J Surg. 1990; 160:387–389.
Article13. Wei FC, Celik N, Yang WG, Chen IH, Chang YM, Chen HC. Complications after reconstruction by plate and soft-tissue free flap in composite mandibular defects and secondary salvage reconstruction with osteocutaneous flap. Plast Reconstr Surg. 2003; 112:37–42.
Article14. Arden RL, Rachel JD, Marks SC, Dang K. Volume-length impact of lateral jaw resections on complication rates. Arch Otolaryngol Head Neck Surg. 1999; 125:68–72.
Article15. Spencer KR, Sizeland A, Taylor GI, Wiesenfeld D. The use of titanium mandibular reconstruction plates in patients with oral cancer. Int J Oral Maxillofac Surg. 1999; 28:288–290.
Article16. Yu Y, Zhang WB, Liu XJ, Guo CB, Yu GY, Peng X. Three-dimensional accuracy of virtual planning and surgical navigation for mandibular reconstruction with free fibula flap. J Oral Maxillofac Surg. 2016; 74:1503.e1–1503.e10.
Article17. Rotaru H, Stan H, Florian IS, Schumacher R, Park YT, Kim SG, et al. Cranioplasty with custom-made implants: analyzing the cases of 10 patients. J Oral Maxillofac Surg. 2012; 70:e169–e176.
Article18. Lee UL, Kwon JS, Woo SH, Choi YJ. Simultaneous bimaxillary surgery and mandibular reconstruction with a 3-dimensional printed titanium implant fabricated by electron beam melting: a preliminary mechanical testing of the printed mandible. J Oral Maxillofac Surg. 2016; 74:1501.e1–1501.e15.
Article19. Cheng G, Li Z, Wan Q, Lv K, Li D, Xing X, et al. A novel animal model treated with tooth extraction to repair the full-thickness defects in the mandible of rabbits. J Surg Res. 2015; 194:706–716.
Article20. Chung SM, Jung IK, Yoon BH, Choi BR, Kim DM, Jang JS. Evaluation of different combinations of biphasic calcium phosphate and growth factors for bone formation in calvarial defects in a rabbit model. Int J Periodontics Restorative Dent. 2016; 36 Suppl:s49–s59.
Article21. Grünheid T, Brugman P, Zentner A, Langenbach GE. Changes in rabbit jaw-muscle activity parameters in response to reduced masticatory load. J Exp Biol. 2010; 213:775–781.
Article22. Moon YM, Kim YJ, Kim MK, Kim SG, Kweon H, Kim TW. Early effect of Botox-A injection into the masseter muscle of rats: functional and histological evaluation. Maxillofac Plast Reconstr Surg. 2015; 37:46.
Article23. Dawood A, Marti Marti B, Sauret-Jackson V, Darwood A. 3D printing in dentistry. Br Dent J. 2015; 219:521–529.
Article24. Chae MP, Smoll NR, Hunter-Smith DJ, Rozen WM. Establishing the natural history and growth rate of ameloblastoma with implications for management: systematic review and meta-analysis. PLoS One. 2015; 10:e0117241.
Article25. Ishida T, Soma K, Miura F. [Stress distribution in mandible induced by occlusal force in different horizontal mandibular positions]. Nihon Kyosei Shika Gakkai Zasshi. 1988; 47:767–779. Japanese.26. Namaki S, Matsumoto M, Ohba H, Tanaka H, Koshikawa N, Shinohara M. Masticatory efficiency before and after surgery in oral cancer patients: comparative study of glossectomy, marginal mandibulectomy and segmental mandibulectomy. J Oral Sci. 2004; 46:113–117.
Article27. Lee SW, György S, Choi JB, Choi JY, Kim SG. Carbon plate shows even distribution of stress, decreases screw loosening, and increases recovery of preoperative daily feed intake amount in a rabbit model of mandibular continuity defects. J Craniomaxillofac Surg. 2014; 42:e245–e251.
Article28. Pinheiro M, Alves JL. The feasibility of a custom-made endoprosthesis in mandibular reconstruction: Implant design and finite element analysis. J Craniomaxillofac Surg. 2015; 43:2116–2128.
Article29. Cohen A, Laviv A, Berman P, Nashef R, Abu-Tair J. Mandibular reconstruction using stereolithographic 3-dimensional printing modeling technology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:661–666.
Article30. Davidson J, Birt BD, Gruss J. A-O plate mandibular reconstruction: a complication critique. J Otolaryngol. 1991; 20:104–107.31. Jo C, Bae D, Choi B, Kim J. Removal of supernumerary teeth utilizing a computer-aided design/computer-aided manufacturing surgical guide. J Oral Maxillofac Surg. 2017; 75:924.e1–924.e9.
Article32. Lee JW, An JH, Park SH, Chong JH, Kim GS, Han J, et al. Retrospective clinical study of an implant with a sandblasted, large-grit, acid-etched surface and internal connection: analysis of short-term success rate and marginal bone loss. Maxillofac Plast Reconstr Surg. 2016; 38:42.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- RECONSTRUCTION OF INTRAORAL JAW DEFECTS WITH CORTICOCANCELLOUS BLOCK OF MANDIBULAR SYMPHYSIS
- Comparison of Mechanical Stability between Fibular Free Flap Reconstruction versus Locking Mandibular Reconstruction Plate Fixation
- The effects of resorbable plate in the healing process of mandibular fracture of the rabbits
- Can bone marrow aspirate improve mandibular fracture repair in camels (Camelus dromedarius)? A preliminary study
- Observation of Compression Plate for Treatment of the Femoral Shaft Fractures