Allergy Asthma Respir Dis.
2019 Oct;7(4):206-211. 10.4168/aard.2019.7.4.206.
Clinical characteristics of nontraumatic chylothorax in pediatric patients
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Hospital, Seoul, Korea.
- 2Department of Pediatrics, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea. stealawayou@hanmail.net
- 3Department of Radiology, Seoul National University Hospital, Seoul, Korea.
- KMID: 2461398
- DOI: http://doi.org/10.4168/aard.2019.7.4.206
Abstract
- PURPOSE
To evaluate clinical characteristics of pediatric nontraumaitc chylothorax and to suggest appropriate therapeutic managements.
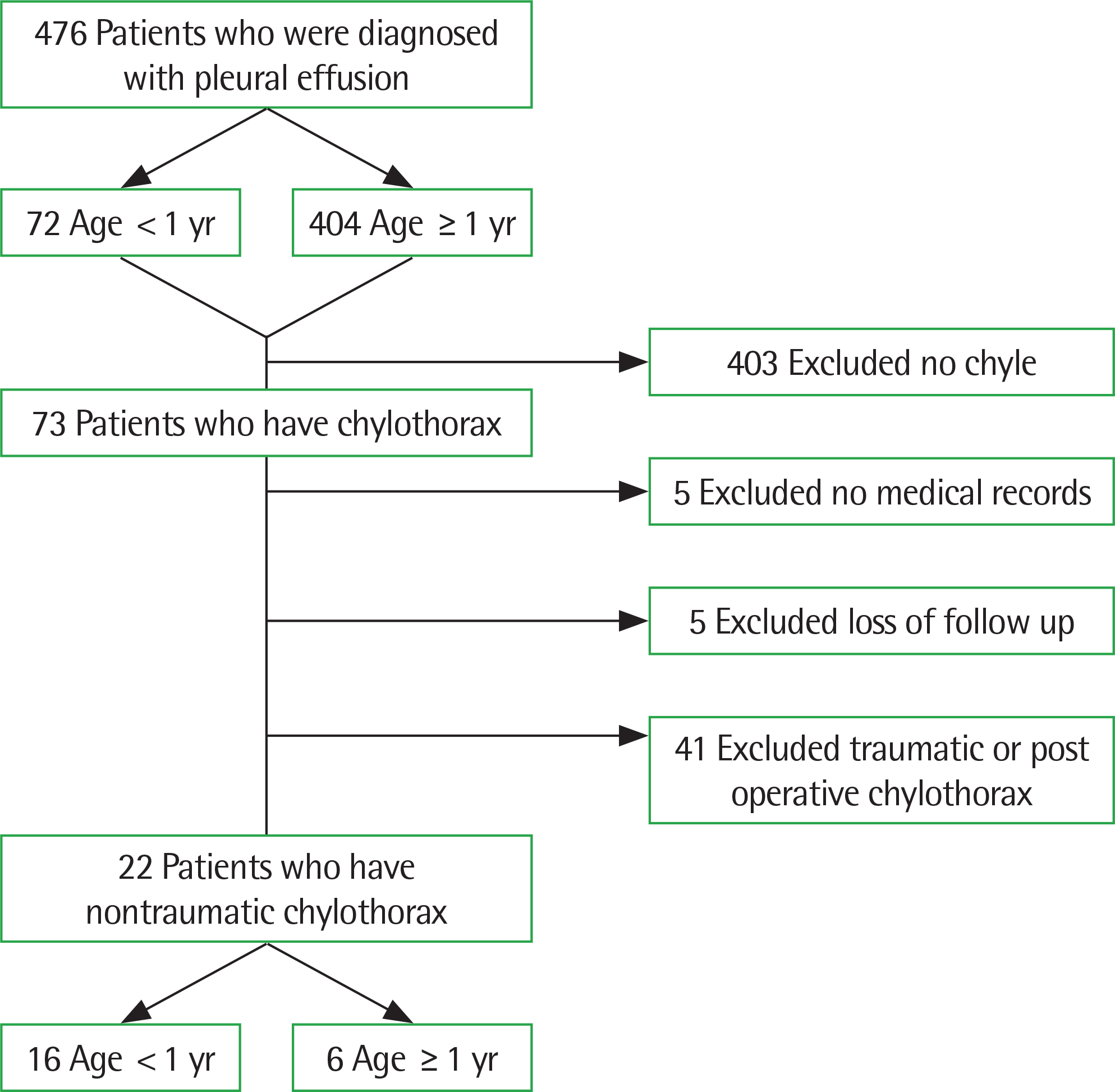
METHODS
We retrospectively reviewed medical records of 22 patients with nontraumatic chylothorax from January 2005 to December 2018 in the Children's Hospital of Seoul National University. We analyze their etiology, treatment, complications and outcome.
RESULTS
Of the 22 patients, 16 were diagnosed before 1 year old and 6 after 1 year old. The causes of chylothorax under 1-year-old children were related to congenital factors (n=9), unknown causes (n=5), and high central venous pressure (n=2). The causes of chylothorax over 1-year-old children were related to congenital factors (n=3), unknown causes (n=1), high venous pressure (n=1), and lymphoma (n=1). All patients had dietary modification. Eight of them were cured by dietary modification, but there was no improvement in over 1-year-old children. Medication was added to patients refractory to dietary modification. Four patients with medication were improved and 5 were improved by surgical management. Nutritional, immunological and other complications occurred in many patients. Five death cases were reported. Four patients were under 1 year old and 1 was over 1 year old. The causes of nontraumatic chylothorax in dead patients were high central venous pressure (n=3), congenital (n=1), and unknown (n=1).
CONCLUSION
Nontraumatic chylothorax more frequently occurs in under 1-year-old children. The most common cause is congenital factors. Stepwise management is effective in many patients, but specific treatment is needed in some cases. The prognosis is related to the onset of age and underlying diseases.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Light RW. Chylothorax and pseudochylothorax. Light RW, editor. Pleural diseases. 6th ed.Philadelphia (PA): Wolters Kluwer Lippincott Williams and Wilkins;2013.2. Hillerdal G. Chylothorax and pseudochylothorax. Eur Respir J. 1997; 10:1157–62.
Article3. Beghetti M, La Scala G, Belli D, Bugmann P, Kalangos A, Le Coultre C. Etiology and management of pediatric chylothorax. J Pediatr. 2000; 136:653–8.
Article4. Büttiker V, Fanconi S, Burger R. Chylothorax in children: guidelines for diagnosis and management. Chest. 1999; 116:682–7.5. Romero S. Nontraumatic chylothorax. Curr Opin Pulm Med. 2000; 6:287–91.
Article6. Soto-Martinez M, Massie J. Chylothorax: diagnosis and management in children. Paediatr Respir Rev. 2009; 10:199–207.
Article7. Milsom JW, Kron IL, Rheuban KS, Rodgers BM. Chylothorax: an assessment of current surgical management. J Thorac Cardiovasc Surg. 1985; 89:221–7.
Article8. Panthongviriyakul C, Bines JE. Postoperative chylothorax in children: an evidence-based management algorithm. J Paediatr Child Health. 2008; 44:716–21.
Article9. Bialkowski A, Poets CF, Franz AR. Erhebungseinheit für seltene pädia-trische Erkrankungen in Deutschland Study Group. Congenital chylothorax: a prospective nationwide epidemiological study in Germany. Arch Dis Child Fetal Neonatal Ed. 2015; 100:F169–72.
Article10. Wu C, Wang Y, Pan Z, Wu Y, Wang Q, Li Y, et al. Analysis of the etiology and treatment of chylothorax in 119 pediatric patients in a single clinical center. J Pediatr Surg. 2019; 54:1293–7.
Article11. van Straaten HL, Gerards LJ, Krediet TG. Chylothorax in the neonatal period. Eur J Pediatr. 1993; 152:2–5.
Article12. Chan DK, Ho NK. Noonan syndrome with spontaneous chylothorax at birth. Aust Paediatr J. 1989; 25:296–8.
Article13. Van Aerde J, Campbell AN, Smyth JA, Lloyd D, Bryan MH. Spontaneous chylothorax in newborns. Am J Dis Child. 1984; 138:961–4.
Article14. Rocha G. Pleural effusions in the neonate. Curr Opin Pulm Med. 2007; 13:305–11.
Article15. Dubin PJ, King IN, Gallagher PG. Congenital chylothorax. Curr Opin Pediatr. 2000; 12:505–9.
Article16. Tutor JD. Chylothorax in infants and children. Pediatrics. 2014; 133:722–33.
Article17. Lin CH, Lin WC, Chang JS. Presentations and management of different causes of chylothorax in children: one medical center's experience. Bio-medicine. 2017; 7:30–4.
Article18. Chernick V, Reed MH. Pneumothorax and chylothorax in the neonatal period. J Pediatr. 1970; 76:624–32.
Article19. Chen E, Itkin M. Thoracic duct embolization for chylous leaks. Semin Intervent Radiol. 2011; 28:63–74.
Article20. Chan SY, Lau W, Wong WH, Cheng LC, Chau AK, Cheung YF. Chylothorax in children after congenital heart surgery. Ann Thorac Surg. 2006; 82:1650–6.
Article21. Cannizzaro V, Frey B, Bernet-Buettiker V. The role of somatostatin in the treatment of persistent chylothorax in children. Eur J Cardiothorac Surg. 2006; 30:49–53.
Article22. Nguyen DM, Shum-Tim D, Dobell AR, Tchervenkov CI. The management of chylothorax/chylopericardium following pediatric cardiac surgery: a 10-year experience. J Card Surg. 1995; 10(4 Pt 1):302–8.
Article23. Bernet-Buettiker V, Waldvogel K, Cannizzaro V, Albisetti M. Antithrom-bin activity in children with chylothorax. Eur J Cardiothorac Surg. 2006; 29:406–9.24. Garty BZ, Levinson AI, Danon YL, Wilmott R, Douglas SD. Lymphocyte subpopulations in children with abnormal lymphatic circulation. J Allergy Clin Immunol. 1989; 84(4 Pt 1):515–20.
Article25. Kovacikova L, Lakomy M, Skrak P, Cingelova D. Immunologic status in pediatric cardiosurgical patients with chylothorax. Bratisl Lek Listy. 2007; 108:3–6.26. Mohan H, Paes ML, Haynes S. Use of intravenous immunoglobulins as an adjunct in the conservative management of chylothorax. Paediatr Anaesth. 1999; 9:89–92.
Article27. Orange JS, Geha RS, Bonilla FA. Acute chylothorax in children: selective retention of memory T cells and natural killer cells. J Pediatr. 2003; 143:243–9.
Article28. Wasmuth-Pietzuch A, Hansmann M, Bartmann P, Heep A. Congenital chylothorax: lymphopenia and high risk of neonatal infections. Acta Paediatr. 2004; 93:220–4.
Article29. Zuluaga MT. Chylothorax after surgery for congenital heart disease. Curr Opin Pediatr. 2012; 24:291–4.
Article30. Mery CM, Moffett BS, Khan MS, Zhang W, Guzmán-Pruneda FA, Fraser CD Jr, et al. Incidence and treatment of chylothorax after cardiac surgery in children: analysis of a large multi-institution database. J Thorac Cardiovasc Surg. 2014; 147:678–86.e1.