J Korean Orthop Assoc.
2019 Oct;54(5):411-417. 10.4055/jkoa.2019.54.5.411.
Comparison of the Clinical Outcomes of a Single Injection Adductor Canal Block with the Concomitant Use of Transdermal Buprenorphine and Continuous Adductor Canal Block after Total Knee Arthroplasty
- Affiliations
-
- 1Department of Orthopedic Surgery, Busan Medical Center, Busan, Korea. jun4128@naver.com
- KMID: 2461230
- DOI: http://doi.org/10.4055/jkoa.2019.54.5.411
Abstract
- PURPOSE
To compare the clinical outcomes of single injection adductor canal block (SACB), continuous adductor canal block (CACB), and the concomitant use of transdermal buprenorphine after total knee arthroplasty (TKA).
MATERIALS AND METHODS
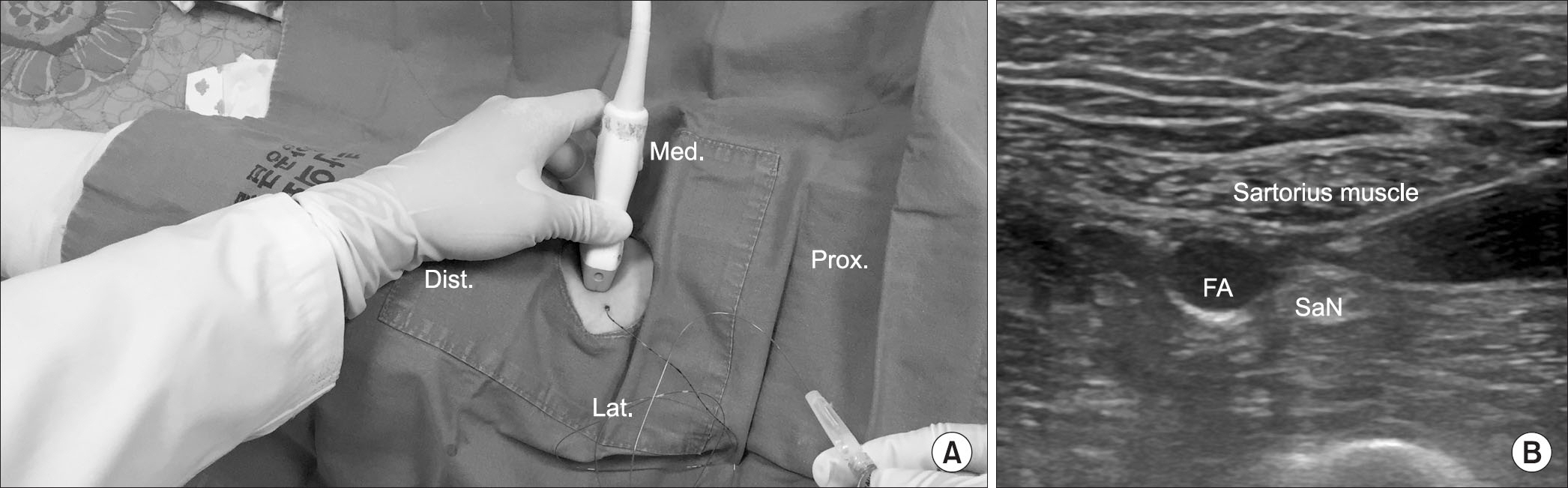
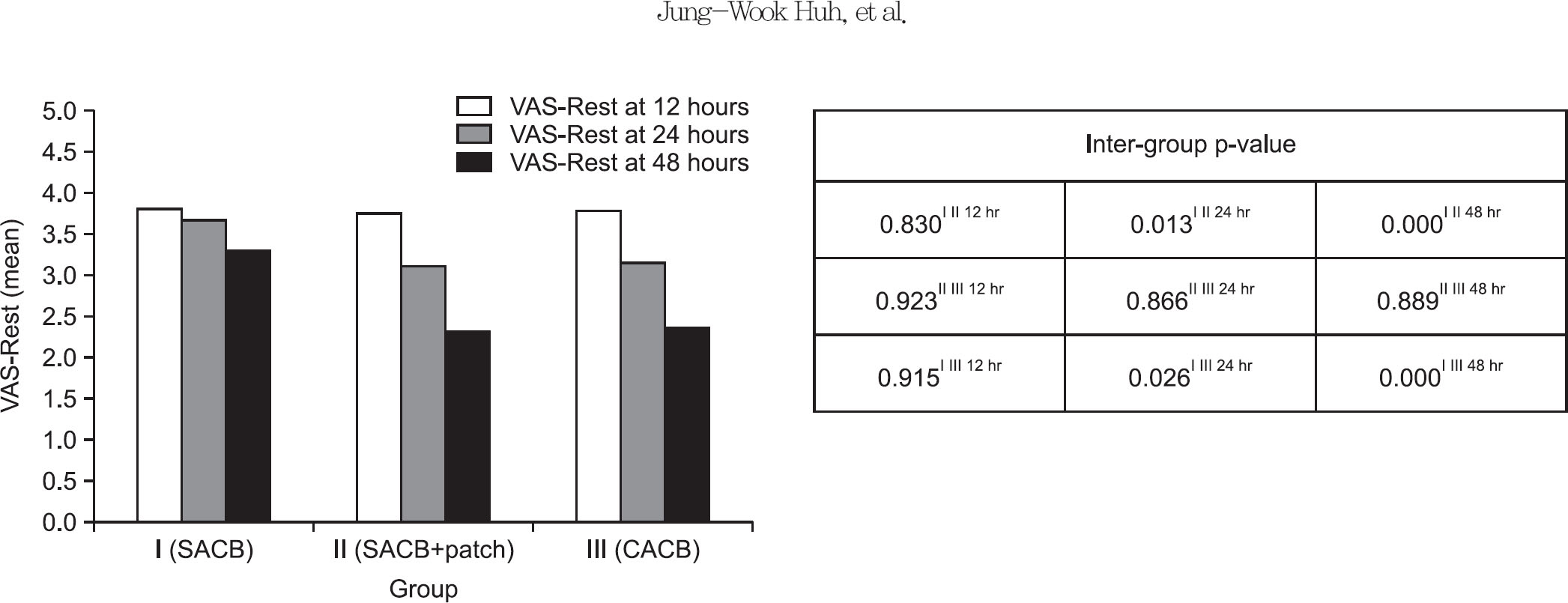
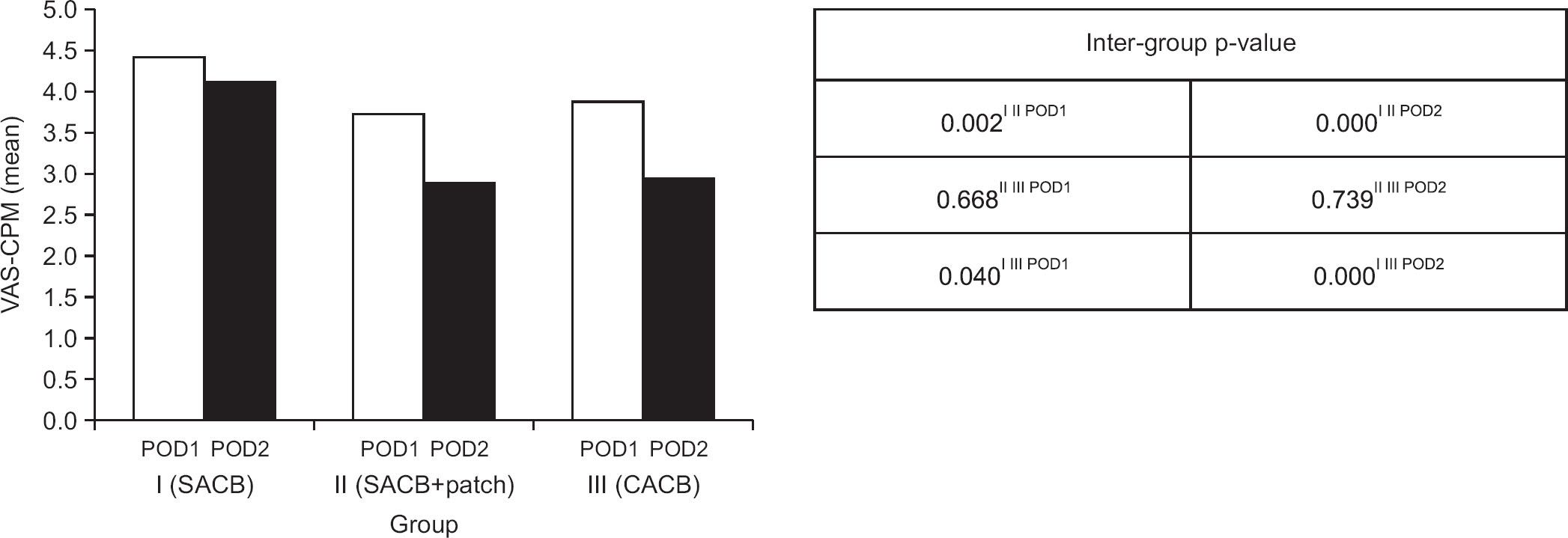
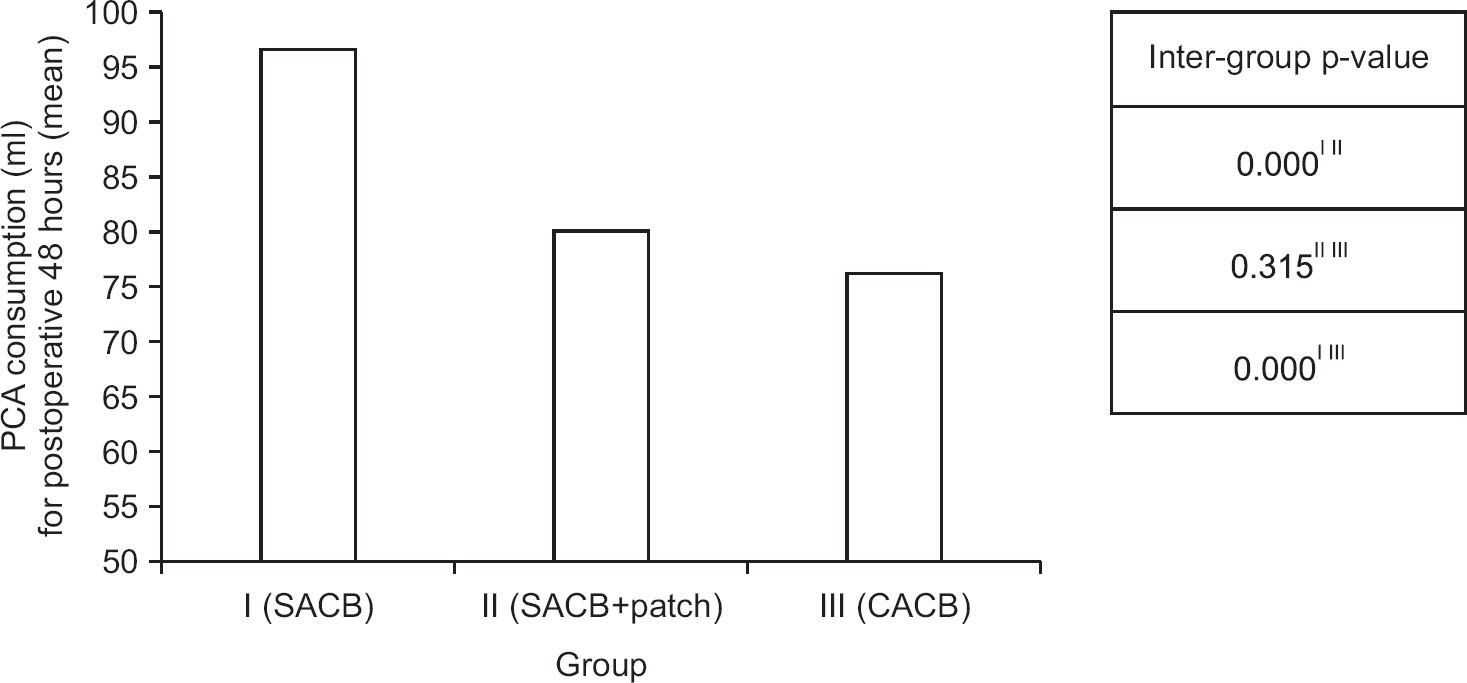
A total of 125 patients who underwent TKA were divided into three groups and the clinical results were retrospecitively compared. Group I was comprised of patients with pain controlled by SACB (n=41). Group II consisted of patients with pain controlled by both SACB and transdermal buprenorphine (10 µg/h) (n=44). Group III contained patients with pain controlled by CACB (n=40). The visual analogue scale (VAS) was used as the pain control indicator and the patients were measured on a VAS for resting on the bed (VAS-Rest) at 12 hours, 24 hours, and 48 hours after surgery. The VAS while doing continuous passive motion (VAS-CPM) on the first and second postoperative day was also measured. In addition, the total amount of medications used (Butopahn, Tridol, and Ketorac) for the intravenous patient controlled analgesia (PCA) was counted for 48 hours after surgery. As the indicator of the functional recovery outcome, the incidence of nausea and vomiting was observed for 48 hours after surgery. The maximum knee joint flexion range and maximum walking distance on the first and second postoperative day, and the total length of stay at the hospital were compared.
RESULTS
The VAS-Rest was similar in the three groups at 12 hours after surgery, but at 24 hours and 48 hours after surgery, group II and III a lower VAS-CPM and total amount of medications used for PCA than group I (p<0.05). The three groups showed a low incidence of nausea and vomiting, maximum knee joint flexion range, and similar walking distance and total length of stay at the hospital.
CONCLUSION
The combination of SACB and transdermal buprenorphine has great pain control effect initially. On the other hand, it is not associated with catheter complications and it is convenient to use and safety toward the renal function. Therefore, the concomitant use of SACB and transdermal buprenorphine can be an effective pain control method after TKA.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Paul JE, Arya A, Hurlburt L. . Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anesthesiology. 2010. 113:1144–62.2. Jæger P, Zaric D, Fomsgaard JS. . Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a randomized, double-blind study. Reg Anesth Pain Med. 2013. 38:526–32.3. Association of Anaesthetists of Great Britain and Ireland, Griffiths R, Alper J. . Management of proximal femoral fractures 2011: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2012. 67:85–98.4. Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg. 2011. 113:904–25.5. Marhofer D, Marhofer P, Triffterer L, Leonhardt M, Weber M, Zeitlinger M. Dislocation rates of perineural catheters: a volunteer study. Br J Anaesth. 2013. 111:800–6.
Article6. Jenkins CR, Karmakar MK. An unusual complication of interscalene brachial plexus catheterization: delayed catheter migration. Br J Anaesth. 2005. 95:535–7.
Article7. Cuvillon P, Ripart J, Lalourcey L. . The continuous femoral nerve block catheter for postoperative analgesia: bacterial colonization, infectious rate and adverse effects. Anesth An-alg. 2001. 93:1045–9.
Article8. Seo SS, Kim OG, Seo JH, Kim DH, Kim YG, Park BY. Comparison of the effect of continuous femoral nerve block and adductor canal block after primary total knee arthroplasty. Clin Orthop Surg. 2017. 9:303–9.
Article9. Plosker GL. Buprenorphine 5, 10 and 20 mg/h transdermal patch: a review of its use in the management of chronic non-malignant pain. Drugs. 2011. 71:2491–509.10. Kapil RP, Cipriano A, Friedman K. . Once-weekly transdermal buprenorphine application results in sustained and consistent steady-state plasma levels. J Pain Symptom Manage. 2013. 46:65–75.
Article11. Grond S, Radbruch L, Lehmann KA. Clinical pharmacokinetics of transdermal opioids: focus on transdermal fentanyl. Clin Pharmacokinet. 2000. 38:59–89.12. Andersen LØ, Gaarn-Larsen L, Kristensen BB, Husted H, Otte KS, Kehlet H. Subacute pain and function after fast-track hip and knee arthroplasty. Anaesthesia. 2009. 64:508–13.
Article13. Lee S, Rooban N, Vaghadia H, Sawka AN, Tang R. A randomized non-inferiority trial of adductor canal block for analgesia after total knee arthroplasty: single injection versus catheter technique. J Arthroplasty. 2018. 33:1045–51.
Article14. Shah NA, Jain NP, Panchal KA. Adductor canal blockade following total knee arthroplasty-continuous or single shot technique? Role in postoperative analgesia, ambulation ability and early functional recovery: a randomized controlled trial. J Arthroplasty. 2015. 30:1476–81.
Article15. Greengrass RA, Klein SM, D’Ercole FJ, Gleason DG, Shimer CL, Steele SM. Lumbar plexus and sciatic nerve block for knee arthroplasty: comparison of ropivacaine and bupivacaine. Can J Anaesth. 1998. 45:1094–6.
Article16. Serpell MG, Millar FA, Thomson MF. Comparison of lumbar plexus block versus conventional opioid analgesia after total knee replacement. Anaesthesia. 1991. 46:275–7.
Article17. Karlsson M, Berggren AC. Efficacy and safety of low-dose transdermal buprenorphine patches (5, 10, and 20 microg/h) versus prolonged-release tramadol tablets (75, 100, 150, and 200 mg) in patients with chronic osteoarthritis pain: a 12-week, randomized, open-label, controlled, parallel-group noninferiority study. Clin Ther. 2009. 31:503–13.18. Kumar S, Chaudhary AK, Singh PK. . Transdermal buprenorphine patches for postoperative pain control in abdominal surgery. J Clin Diagn Res. 2016. 10:UC05–8.
Article19. Sisak K, Lloyd J, Fiddian N. Multi-ligament instability after early dislocation of a primary total knee replacement: case report. Knee. 2011. 18:59–61.20. Chan EY, Fransen M, Sathappan S, Chua NH, Chan YH, Chua N. Comparing the analgesia effects of single-injection and continuous femoral nerve blocks with patient controlled analgesia after total knee arthroplasty. J Arthroplasty. 2013. 28:608–13.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Effect of Continuous Femoral Nerve Block and Adductor Canal Block after Primary Total Knee Arthroplasty
- The relative analgesic value of a femoral nerve block versus adductor canal block following total knee arthroplasty: a randomized, controlled, double-blinded study
- The feasibility of direct adductor canal block (DACB) as a part of periarticular injection in total knee arthroplasty
- Does Combination Therapy of Popliteal Sciatic Nerve Block and Adductor Canal Block Effectively Control Early Postoperative Pain after Total Knee Arthroplasty?
- Can bedside patient-reported numbness predict postoperative ambulation ability for total knee arthroplasty patients with nerve block catheters?