J Korean Acad Prosthodont.
2019 Oct;57(4):342-349. 10.4047/jkap.2019.57.4.342.
Retrospective study on survival, success rate and complication of implant-supported fixed prosthesis according to the materials in the posterior area
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry and Institute of Oral Bio-Science, Chonbuk National University, Jeonju, Republic of Korea. jmseo@jbnu.ac.kr
- KMID: 2461140
- DOI: http://doi.org/10.4047/jkap.2019.57.4.342
Abstract
- PURPOSE
The purpose of this study was to retrospectively investigate the survival and success rate of implant-supported fixed prosthesis according to the materials in the posterior area. Other purposes were to observe the complications and evaluate the factors affecting failure.
MATERIALS AND METHODS
Patients who had been restored implant prosthesis in the posterior area by the same prosthodontist in the department of prosthodontics, dental hospital, Chonbuk National University, in the period from January 2011 to June 2018 were selected for the study. The patient's sex, age, material, location, type of prosthesis and complications were examined using medical records. The Kaplan-Meier method was used to analyze the survival and success rate. The Log-rank test was conducted to compare the differences between the groups. Cox proportional hazards model was used to assess the association between potential risk factors and success rate.
RESULTS
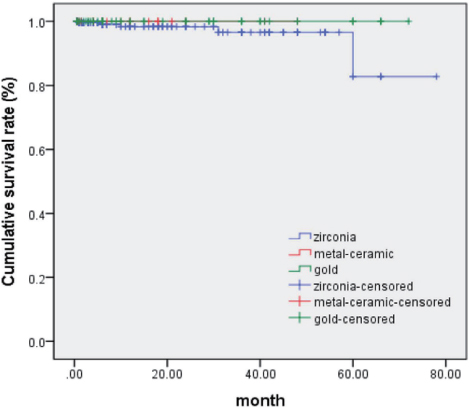
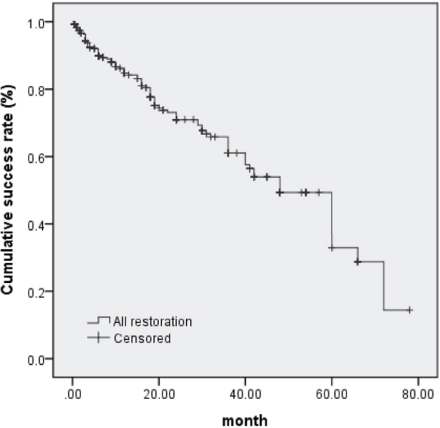
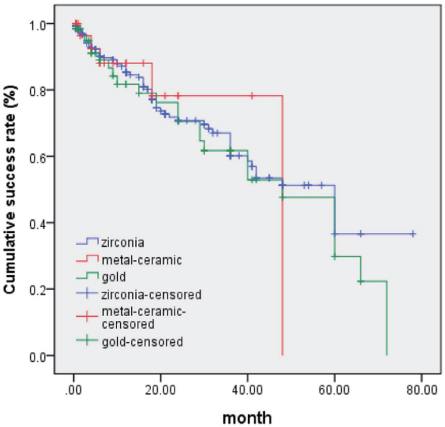
A total of 364 implants were observed in 245 patients, with an average follow-up of 17.1 months. A total of 5 implant prostheses failed and were removed, and the 3 and 5 year cumulative survival rate of all implant prostheses were 97.5 and 91.0, respectively. The 3 and 5 year cumulative success rate of all implant prostheses were 61.1% and 32.9%, respectively. Material, sex, age, location and type of prosthesis did not affect success rate (P>.05). Complications occurred in the order of proximal contact loss (53 cases), retention loss (17 cases), peri-implant mucositis (12 cases), infraocclusion (4 cases) and so on.
CONCLUSION
Considering a high cumulative survival rate of implant-supported fixed prostheses, regardless of the materials, implant restored in posterior area can be considered as a reliable treatment to tooth replacement. However, regular inspections and, if necessary, repairs and adjustments are very important because of the frequent occurrence of complications
Keyword
MeSH Terms
Figure
Reference
-
1. Fehmer V, Mühlemann S, Hämmerle CH, Sailer I. Criteria for the selection of restoration materials. Quintessence Int. 2014; 45:723–730.2. Benic GI, Mühlemann S, Fehmer V, Hämmerle CH, Sailer I. Randomized controlled within-subject evaluation of digital and conventional workflows for the fabrication of lithium disilicate single crowns. Part I: digital versus conventional unilateral impressions. J Prosthet Dent. 2016; 116:777–782.
Article3. Guess PC, Att W, Strub JR. Zirconia in fixed implant prosthodontics. Clin Implant Dent Relat Res. 2012; 14:633–645.
Article4. Silva NR, Bonfante EA, Zavanelli RA, Thompson VP, Ferencz JL, Coelho PG. Reliability of metalloceramic and zirconia-based ceramic crowns. J Dent Res. 2010; 89:1051–1056.
Article5. Walton TR. An up-to-15-year comparison of the survival and complication burden of three-unit tooth-supported fixed dental prostheses and implant-supported single crowns. Int J Oral Maxillofac Implants. 2015; 30:851–861.
Article6. Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003; 90:121–132.
Article7. Göthberg C, Bergendal T, Magnusson T. Complications after treatment with implant-supported fixed prostheses: a retrospective study. Int J Prosthodont. 2003; 16:201–207.8. Byun SJ, Heo SM, Ahn SG, Chang M. Analysis of proximal contact loss between implant-supported fixed dental prostheses and adjacent teeth in relation to influential factors and effects. A cross-sectional study. Clin Oral Implants Res. 2015; 26:709–714.
Article9. Yoon JH, Park YB, Youn SH, Oh NS. Korea Academy of Prosthodontics criteria for longevity studies of dental prostheses. J Korean Acad Prosthodont. 2016; 54:341–353.
Article10. Pjetursson BE, Valente NA, Strasding M, Zwahlen M, Liu S, Sailer I. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic single crowns. Clin Oral Implants Res. 2018; 29:199–214.
Article11. Buser D, Weber HP, Lang NP. Tissue integration of non-submerged implants. 1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res. 1990; 1:33–40.
Article12. Cochran DL, Buser D, ten Bruggenkate CM, Weingart D, Taylor TM, Bernard JP, Peters F, Simpson JP. The use of reduced healing times on ITI implants with a sandblasted and acid-etched (SLA) surface: early results from clinical trials on ITI SLA implants. Clin Oral Implants Res. 2002; 13:144–153.
Article13. Pjetursson BE, Tan K, Lang NP, Brägger U, Egger M, Zwahlen M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004; 15:625–642.
Article14. Koori H, Morimoto K, Tsukiyama Y, Koyano K. Statistical analysis of the diachronic loss of interproximal contact between fixed implant prostheses and adjacent teeth. Int J Prosthodont. 2010; 23:535–540.15. Chopra A, Sivaraman K, Narayan AI, Balakrishnan D. Etiology and classification of food impaction around implants and implant-retained prosthesis. Clin Implant Dent Relat Res. 2019; 21:391–397.
Article16. Michalakis KX, Pissiotis AL, Hirayama H. Cement failure loads of 4 provisional luting agents used for the cementation of implant-supported fixed partial dentures. Int J Oral Maxillofac Implants. 2000; 15:545–549.17. In J, Lee DK. Survival analysis: Part I - analysis of time-to-event. Korean J Anesthesiol. 2018; 71:182–191.
Article18. Lin RS, León LF. Estimation of treatment effects in weighted log-rank tests. Contemp Clin Trials Commun. 2017; 8:147–155.
Article19. Sailer I, Strasding M, Valente NA, Zwahlen M, Liu S, Pjetursson BE. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic multiple-unit fixed dental prostheses. Clin Oral Implants Res. 2018; 29:184–198.
Article20. Schneider D, Witt L, Hämmerle CHF. Influence of the crown-to-implant length ratio on the clinical performance of implants supporting single crown restorations: a cross-sectional retrospective 5-year investigation. Clin Oral Implants Res. 2012; 23:169–174.
Article21. Kolgeci L, Mericske E, Worni A, Walker P, Katsoulis J, Mericske-Stern R. Technical complications and failures of zirconia-based prostheses supported by implants followed up to 7 years: a case series. Int J Prosthodont. 2014; 27:544–552.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A retrospective comparison of clinical outcomes of implant restorations for posterior edentulous area: 3-unit bridge supported by 2 implants vs 3 splinted implant-supported crowns
- Occlusion for implant-supported fixed dental prostheses in partially edentulous patients: a literature review and current concepts
- Reinforcing the retention of provisional restoration using provisional implant on maxillary anterior region: clinical case report
- Full mouth rehabilitation of edentulous patient with fixed implant prosthesis
- Implant success rates in full-arch rehabilitations supported by upright and tilted implants: a retrospective investigation with up to five years of follow-up