Diabetes Metab J.
2019 Oct;43(5):627-639. 10.4093/dmj.2018.0141.
Longitudinal Changes of Body Composition Phenotypes and Their Association with Incident Type 2 Diabetes Mellitus during a 5-Year Follow-up in Koreans
- Affiliations
-
- 1Health Screening and Promotion Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. hkkim0801@amc.seoul.kr
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea.
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2460956
- DOI: http://doi.org/10.4093/dmj.2018.0141
Abstract
- BACKGROUND
To elucidate longitudinal changes of complex body composition phenotypes and their association with incident type 2 diabetes mellitus.
METHODS
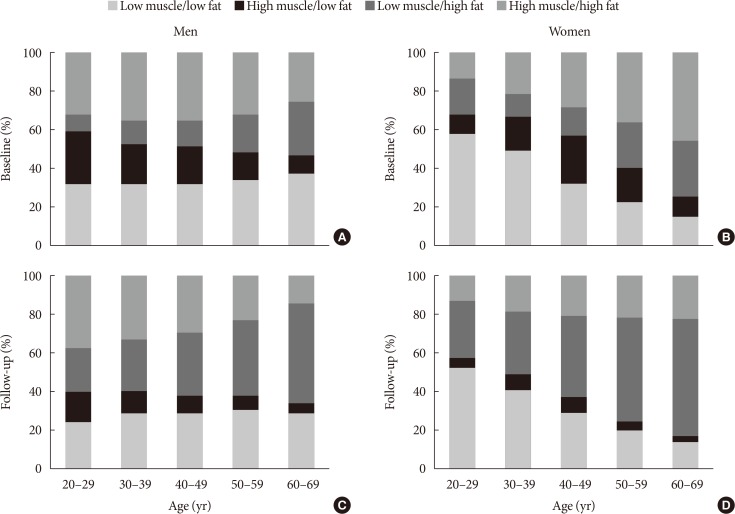
A total of 17,280 (mean age, 48.1±8.2 years) Korean adults who underwent medical check-ups were included. The mean follow-up duration was 5.5±0.5 years. Body compositions were assessed using a bioelectrical impedance analysis. Four body composition phenotypes were defined using the median of appendicular skeletal muscle mass (ASM) index and fat mass index: low muscle/low fat (LM/LF); high muscle (HM)/LF; LM/high fat (HF); and HM/HF groups.
RESULTS
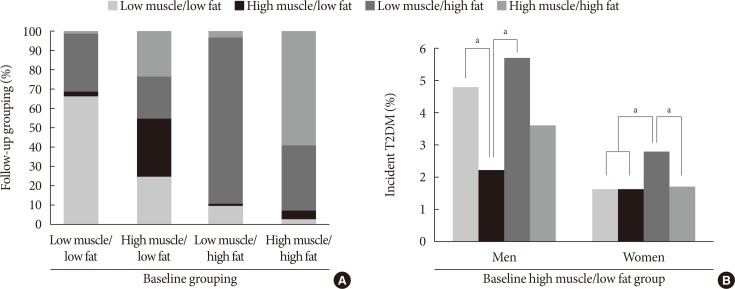
Of the individuals in the LM/LF or HM/HF groups, over 60% remained in the same group, and over 30% were moved to the LM/HF group. Most of the LM/HF group remained in this group. In the baseline HM/LF group, approximately 30% stayed in the group, and the remaining individuals transitioned to the three other groups in similar proportions. Incident diabetes was significantly lower in participants who remained in the HM/LF group than those who transitioned to the LM/LF or LM/HF group from the baseline HM/LF group in men. ASM index was significantly associated with a decreased risk for incident diabetes in men regardless of obesity status (adjusted odds ratio [OR], 0.71 per kg/m²; 95% confidence interval [CI], 0.52 to 0.97 in non-obese) (adjusted OR, 0.87; 95% CI, 0.77 to 0.98 in obese) after adjusting for other strong risk factors (e.g., baseline glycosylated hemoglobin and homeostasis model assessment of insulin resistance).
CONCLUSION
Maintenance of ASM may be protective against the development of type 2 diabetes mellitus in men, regardless of obesity status.
MeSH Terms
Figure
Cited by 2 articles
-
Age- and Sex-Related Differential Associations between Body Composition and Diabetes Mellitus
Eun Roh, Soon Young Hwang, Jung A Kim, You-Bin Lee, So-hyeon Hong, Nam Hoon Kim, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Diabetes Metab J. 2021;45(2):183-194. doi: 10.4093/dmj.2019.0171.Impact of the Dynamic Change of Metabolic Health Status on the Incident Type 2 Diabetes: A Nationwide Population-Based Cohort Study
Jung A Kim, Da Hye Kim, Seon Mee Kim, Yong Gyu Park, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi, Kyungdo Han, Hye Jin Yoo
Endocrinol Metab. 2019;34(4):406-414. doi: 10.3803/EnM.2019.34.4.406.
Reference
-
1. Gallagher D, Visser M, De Meersman RE, Sepulveda D, Baumgartner RN, Pierson RN, Harris T, Heymsfield SB. Appendicular skeletal muscle mass: effects of age, gender, and ethnicity. J Appl Physiol (1985). 1997; 83:229–239. PMID: 9216968.2. Fantin F, Di Francesco V, Fontana G, Zivelonghi A, Bissoli L, Zoico E, Rossi A, Micciolo R, Bosello O, Zamboni M. Longitudinal body composition changes in old men and women: interrelationships with worsening disability. J Gerontol A Biol Sci Med Sci. 2007; 62:1375–1381. PMID: 18166688.
Article3. Liu LK, Lee WJ, Liu CL, Chen LY, Lin MH, Peng LN, Chen LK. Age-related skeletal muscle mass loss and physical performance in Taiwan: implications to diagnostic strategy of sarcopenia in Asia. Geriatr Gerontol Int. 2013; 13:964–971. PMID: 23452090.
Article4. Prado CM, Siervo M, Mire E, Heymsfield SB, Stephan BC, Broyles S, Smith SR, Wells JC, Katzmarzyk PT. A population-based approach to define body-composition phenotypes. Am J Clin Nutr. 2014; 99:1369–1377. PMID: 24760978.
Article5. Bai HJ, Sun JQ, Chen M, Xu DF, Xie H, Yu ZW, Bao ZJ, Chen J, Pan YR, Lu DJ, Cheng S. Age-related decline in skeletal muscle mass and function among elderly men and women in Shanghai, China: a cross sectional study. Asia Pac J Clin Nutr. 2016; 25:326–332. PMID: 27222416.6. Frontera WR, Hughes VA, Fielding RA, Fiatarone MA, Evans WJ, Roubenoff R. Aging of skeletal muscle: a 12-yr longitudinal study. J Appl Physiol (1985). 2000; 88:1321–1326. PMID: 10749826.
Article7. DeFronzo RA, Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care. 2009; 32 Suppl 2:S157–S163. PMID: 19875544.
Article8. Srikanthan P, Hevener AL, Karlamangla AS. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: findings from the National Health and Nutrition Examination Survey III. PLoS One. 2010; 5:e10805. PMID: 22421977.
Article9. Leenders M, Verdijk LB, van der Hoeven L, Adam JJ, van Kranenburg J, Nilwik R, van Loon LJ. Patients with type 2 diabetes show a greater decline in muscle mass, muscle strength, and functional capacity with aging. J Am Med Dir Assoc. 2013; 14:585–592. PMID: 23537893.
Article10. Kim KS, Park KS, Kim MJ, Kim SK, Cho YW, Park SW. Type 2 diabetes is associated with low muscle mass in older adults. Geriatr Gerontol Int. 2014; 14 Suppl 1:115–121.
Article11. Kim CH, Kim HK, Kim EH, Bae SJ, Park JY. Association between changes in body composition and risk of developing type 2 diabetes in Koreans. Diabet Med. 2014; 31:1393–1398. PMID: 24957933.
Article12. Larsen BA, Wassel CL, Kritchevsky SB, Strotmeyer ES, Criqui MH, Kanaya AM, Fried LF, Schwartz AV, Harris TB, Ix JH. Health ABC Study. Association of muscle mass, area, and strength with incident diabetes in older adults: the health ABC Study. J Clin Endocrinol Metab. 2016; 101:1847–1855. PMID: 26930180.
Article13. Li JJ, Wittert GA, Vincent A, Atlantis E, Shi Z, Appleton SL, Hill CL, Jenkins AJ, Januszewski AS, Adams RJ. Muscle grip strength predicts incident type 2 diabetes: population-based cohort study. Metabolism. 2016; 65:883–892. PMID: 27173467.
Article14. Son JW, Lee SS, Kim SR, Yoo SJ, Cha BY, Son HY, Cho NH. Low muscle mass and risk of type 2 diabetes in middle-aged and older adults: findings from the KoGES. Diabetologia. 2017; 60:865–872. PMID: 28102434.
Article15. Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002; 50:889–896. PMID: 12028177.
Article16. Landi F, Liperoti R, Fusco D, Mastropaolo S, Quattrociocchi D, Proia A, Tosato M, Bernabei R, Onder G. Sarcopenia and mortality among older nursing home residents. J Am Med Dir Assoc. 2012; 13:121–126. PMID: 21856243.
Article17. Tanimoto Y, Watanabe M, Sun W, Tanimoto K, Shishikura K, Sugiura Y, Kusabiraki T, Kono K. Association of sarcopenia with functional decline in community-dwelling elderly subjects in Japan. Geriatr Gerontol Int. 2013; 13:958–963. PMID: 23452074.
Article18. Kim JH, Lim S, Choi SH, Kim KM, Yoon JW, Kim KW, Lim JY, Park KS, Jang HC. Sarcopenia: an independent predictor of mortality in community-dwelling older Korean men. J Gerontol A Biol Sci Med Sci. 2014; 69:1244–1252. PMID: 24721723.
Article19. Vetrano DL, Landi F, Volpato S, Corsonello A, Meloni E, Bernabei R, Onder G. Association of sarcopenia with short- and long-term mortality in older adults admitted to acute care wards: results from the CRIME study. J Gerontol A Biol Sci Med Sci. 2014; 69:1154–1161. PMID: 24744390.
Article20. Cuthbertson DJ, Bell JA, Ng SY, Kemp GJ, Kivimaki M, Hamer M. Dynapenic obesity and the risk of incident type 2 diabetes: the English Longitudinal Study of Ageing. Diabet Med. 2016; 33:1052–1059. PMID: 26479063.
Article21. Crump C, Sundquist J, Winkleby MA, Sieh W, Sundquist K. Physical fitness among swedish military conscripts and long-term risk for type 2 diabetes mellitus: a cohort study. Ann Intern Med. 2016; 164:577–584. PMID: 26954518.22. Jae SY, Franklin BA, Choo J, Yoon ES, Choi YH, Park WH. Fitness, body habitus, and the risk of incident type 2 diabetes mellitus in Korean men. Am J Cardiol. 2016; 117:585–589. PMID: 26721657.
Article23. Miljkovic I, Kuipers AL, Cauley JA, Prasad T, Lee CG, Ensrud KE, Cawthon PM, Hoffman AR, Dam TT, Gordon CL, Zmuda JM. Osteoporotic Fractures in Men Study Group. Greater skeletal muscle fat infiltration is associated with higher all-cause and cardiovascular mortality in older men. J Gerontol A Biol Sci Med Sci. 2015; 70:1133–1140. PMID: 25838547.
Article24. Eibich P, Buchmann N, Kroh M, Wagner GG, Steinhagen-Thiessen E, Demuth I, Norman K. Exercise at different ages and appendicular lean mass and strength in later life: results from the Berlin Aging Study II. J Gerontol A Biol Sci Med Sci. 2016; 71:515–520. PMID: 26442900.
Article25. Zampieri S, Pietrangelo L, Loefler S, Fruhmann H, Vogelauer M, Burggraf S, Pond A, Grim-Stieger M, Cvecka J, Sedliak M, Tirpakova V, Mayr W, Sarabon N, Rossini K, Barberi L, De Rossi M, Romanello V, Boncompagni S, Musaro A, Sandri M, Protasi F, Carraro U, Kern H. Lifelong physical exercise delays age-associated skeletal muscle decline. J Gerontol A Biol Sci Med Sci. 2015; 70:163–173. PMID: 24550352.
Article26. Kim YS, Lee Y, Chung YS, Lee DJ, Joo NS, Hong D, Song Ge, Kim HJ, Choi YJ, Kim KM. Prevalence of sarcopenia and sarcopenic obesity in the Korean population based on the Fourth Korean National Health and Nutritional Examination Surveys. J Gerontol A Biol Sci Med Sci. 2012; 67:1107–1113. PMID: 22431554.
Article27. Anderson LJ, Erceg DN, Schroeder ET. Utility of multifrequency bioelectrical impedance compared with dual-energy X-ray absorptiometry for assessment of total and regional body composition varies between men and women. Nutr Res. 2012; 32:479–485. PMID: 22901555.
Article28. Ling CH, de Craen AJ, Slagboom PE, Gunn DA, Stokkel MP, Westendorp RG, Maier AB. Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clin Nutr. 2011; 30:610–615. PMID: 21555168.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Body Composition and Diabetes
- Serum Transferrin Predicts New-Onset Type 2 Diabetes in Koreans: A 4-Year Retrospective Longitudinal Study
- Adolescent Build Plotting on Body Composition Chart and the Type of Diabetes Mellitus
- Body Composition Analysis in Newly Diagnosed Diabetic Adolescent Girls
- The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea