Cancer Res Treat.
2019 Oct;51(4):1357-1369. 10.4143/crt.2018.430.
Surveillance Rate and its Impact on Survival of Hepatocellular Carcinoma Patients in South Korea: A Cohort Study
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. jsh@snubh.org
- KMID: 2460585
- DOI: http://doi.org/10.4143/crt.2018.430
Abstract
- PURPOSE
Though regular surveillance of hepatocellular carcinoma (HCC) for high-risk patients is widely recommended, its rate and effectiveness are not clear. The aim of this study is to investigate the actual rate of HCC surveillance and its related factors and to clarify its impact on survival in a Korean HCC cohort.
MATERIALS AND METHODS
From 2012 to 2015, 319 newly diagnosed HCC patients were prospectively enrolled at a tertiary hospital. Patient interviews based on a structured questionnaire survey were conducted. Surveillance was defined as liver imaging test ≥ 2 times with at least 3-month interval within 2 years prior to HCC diagnosis.
RESULTS
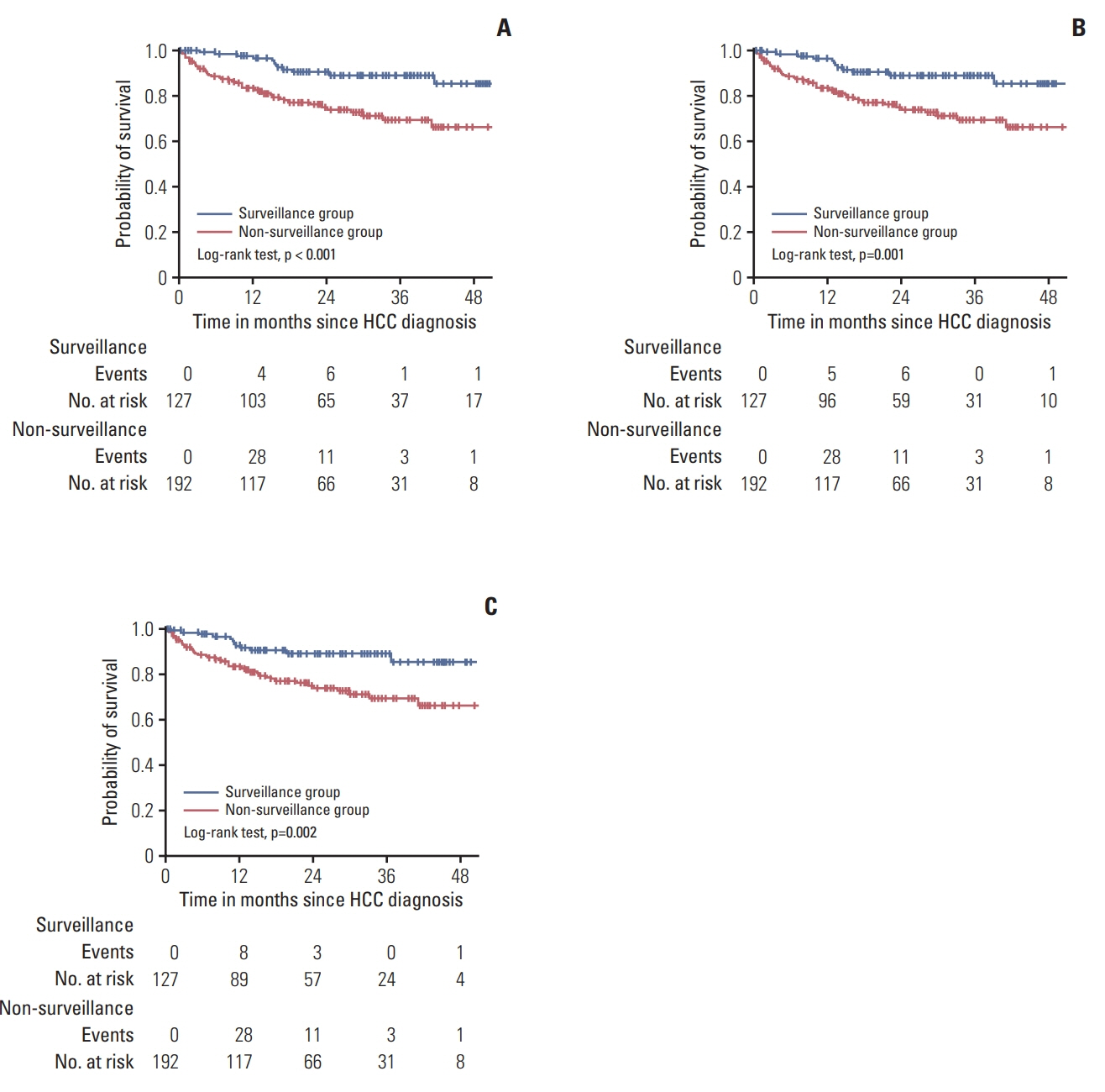
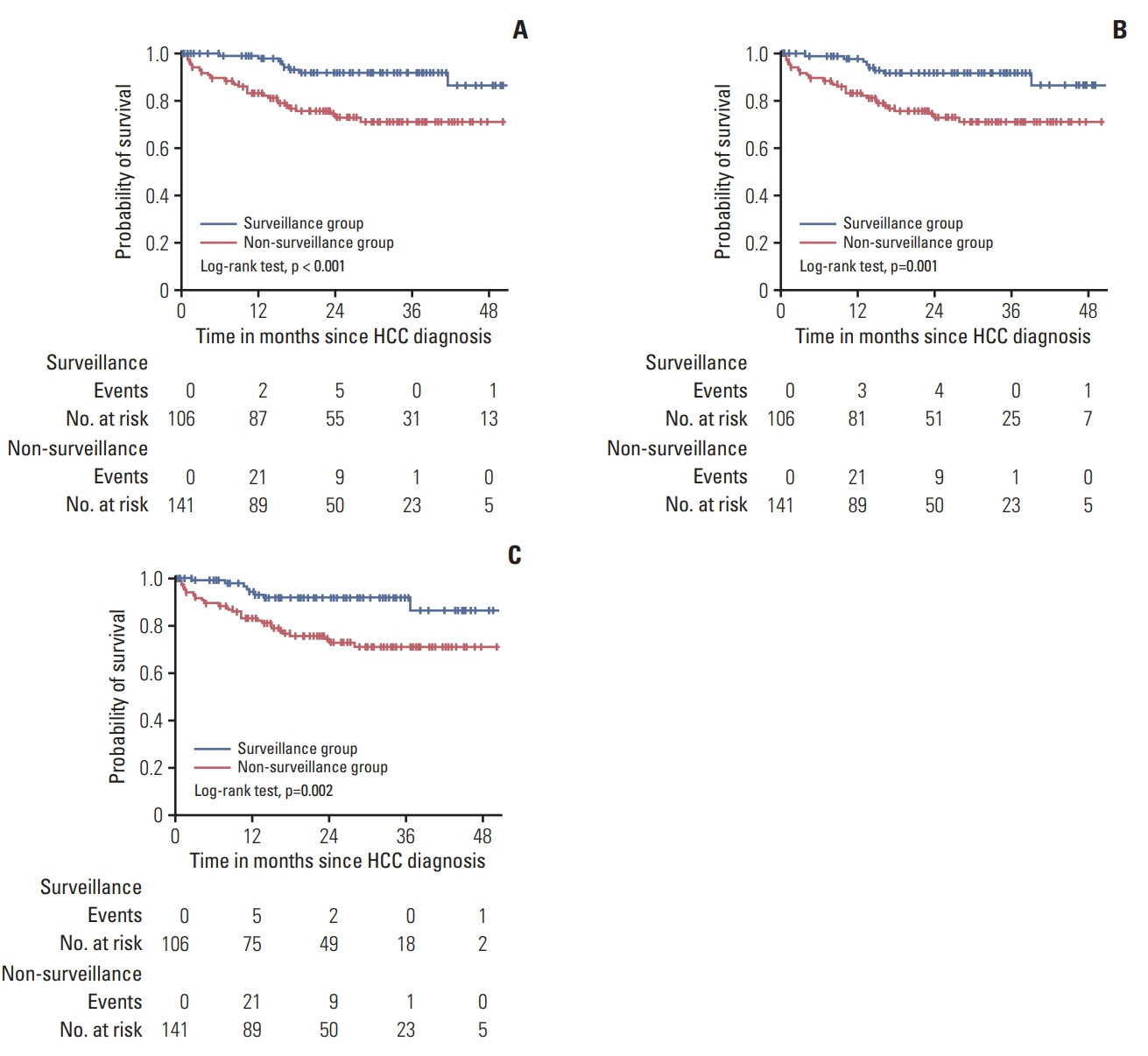
Surveillance rate was 39.8%. Of the HCC patients with high-risk factors, only 182 (57.1%) had knowledge for the need for regular surveillance, and 141 (44.2%) had the accurate information about the method (ultrasound-based study). Surveillance group showed a higher proportion of early HCC (p < 0.001) and a longer overall survival (p < 0.001) compared to non-surveillance group. The multivariable Cox regression analysis indicated Child-Pugh class A, history of anti-viral therapy, low serum α-fetoprotein level, non-advanced Barcelona Clinic Liver Cancer stage as independent predictors of overall survival, while regular surveillance was not (p=0.436).
CONCLUSION
Less than half of the newly diagnosed Korean HCC patients were under surveillance and the accurate perception for the need of HCC surveillance was insufficient. Of those under surveillance, most patients were diagnosed with early stage HCC, which led to the improved survival. Comprehensive efforts to optimize the surveillance program for the target population are warranted.
MeSH Terms
Figure
Reference
-
References
1. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol. 2017; 3:524–48.2. Stuart KE, Anand AJ, Jenkins RL. Hepatocellular carcinoma in the United States: prognostic features, treatment outcome, and survival. Cancer. 1996; 77:2217–22.
Article3. Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011; 53:1020–2.
Article4. European Association for the Study of The Liver; European Organisation for Research and Treatment of Cancer. EASLEORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012; 56:908–43.5. Singal AG, Yopp A, Skinner CS, Packer M, Lee WM, Tiro JA. Utilization of hepatocellular carcinoma surveillance among American patients: a systematic review. J Gen Intern Med. 2012; 27:861–7.
Article6. Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2004; 130:417–22.
Article7. Kansagara D, Papak J, Pasha AS, O'Neil M, Freeman M, Relevo R, et al. Screening for hepatocellular carcinoma in chronic liver disease: a systematic review. Ann Intern Med. 2014; 161:261–9.8. Mittal S, Kanwal F, Ying J, Chung R, Sada YH, Temple S, et al. Effectiveness of surveillance for hepatocellular carcinoma in clinical practice: a United States cohort. J Hepatol. 2016; 65:1148–54.
Article9. Kim DY, Kim HJ, Jeong SE, Kim SG, Kim HJ, Sinn DH, et al. The Korean guideline for hepatocellular carcinoma surveillance. J Korean Med Assoc. 2015; 58:385–97.
Article10. Lee JM, Park JW, Choi BI. 2014 KLCSG-NCC Korea Practice Guidelines for the management of hepatocellular carcinoma: HCC diagnostic algorithm. Dig Dis. 2014; 32:764–77.
Article11. Kudo M, Zheng RQ, Kim SR, Okabe Y, Osaki Y, Iijima H, et al. Diagnostic accuracy of imaging for liver cirrhosis compared to histologically proven liver cirrhosis: a multicenter collaborative study. Intervirology. 2008; 51 Suppl 1:17–26.12. Minagawa M, Ikai I, Matsuyama Y, Yamaoka Y, Makuuchi M. Staging of hepatocellular carcinoma: assessment of the Japanese TNM and AJCC/UICC TNM systems in a cohort of 13,772 patients in Japan. Ann Surg. 2007; 245:909–22.13. Forner A, Reig ME, de Lope CR, Bruix J. Current strategy for staging and treatment: the BCLC update and future prospects. Semin Liver Dis. 2010; 30:61–74.
Article14. Duffy SW, Nagtegaal ID, Wallis M, Cafferty FH, Houssami N, Warwick J, et al. Correcting for lead time and length bias in estimating the effect of screen detection on cancer survival. Am J Epidemiol. 2008; 168:98–104.
Article15. Cucchetti A, Trevisani F, Pecorelli A, Erroi V, Farinati F, Ciccarese F, et al. Estimation of lead-time bias and its impact on the outcome of surveillance for the early diagnosis of hepatocellular carcinoma. J Hepatol. 2014; 61:333–41.
Article16. Singal AG, Pillai A, Tiro J, et al. Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med. 2014; 11:e1001624.
Article17. Edenvik P, Davidsdottir L, Oksanen A, Isaksson B, Hultcrantz R, Stal P. Application of hepatocellular carcinoma surveillance in a European setting: what can we learn from clinical practice? Liver Int. 2015; 35:1862–71.
Article18. Selvapatt N, House H, Brown A. Hepatocellular carcinoma surveillance: are we utilizing it? J Clin Gastroenterol. 2016; 50:e8–12.19. Dalton-Fitzgerald E, Tiro J, Kandunoori P, Halm EA, Yopp A, Singal AG. Practice patterns and attitudes of primary care providers and barriers to surveillance of hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol. 2015; 13:791–8.
Article20. McGowan CE, Edwards TP, Luong MU, Hayashi PH. Suboptimal surveillance for and knowledge of hepatocellular carcinoma among primary care providers. Clin Gastroenterol Hepatol. 2015; 13:799–804.
Article21. Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al. Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis. Health Technol Assess. 2007; 11:1–206.
Article22. Farvardin S, Patel J, Khambaty M, Yerokun OA, Mok H, Tiro JA, et al. Patient-reported barriers are associated with lower hepatocellular carcinoma surveillance rates in patients with cirrhosis. Hepatology. 2017; 65:875–84.
Article23. Mancebo A, Gonzalez-Dieguez ML, Navascues CA, Cadahia V, Varela M, Perez R, et al. Adherence to a semiannual surveillance program for hepatocellular carcinoma in patients with liver cirrhosis. J Clin Gastroenterol. 2017; 51:557–63.
Article24. Singal AG, Volk ML, Rakoski MO, Fu S, Su GL, McCurdy H, et al. Patient involvement in healthcare is associated with higher rates of surveillance for hepatocellular carcinoma. J Clin Gastroenterol. 2011; 45:727–32.
Article25. Santi V, Trevisani F, Gramenzi A, Grignaschi A, Mirici-Cappa F, Del Poggio P, et al. Semiannual surveillance is superior to annual surveillance for the detection of early hepatocellular carcinoma and patient survival. J Hepatol. 2010; 53:291–7.
Article26. Wu CY, Hsu YC, Ho HJ, Chen YJ, Lee TY, Lin JT. Association between ultrasonography screening and mortality in patients with hepatocellular carcinoma: a nationwide cohort study. Gut. 2016; 65:693–701.
Article27. van Meer S, de Man RA, Coenraad MJ, Sprengers D, van Nieuwkerk KM, Klumpen HJ, et al. Surveillance for hepatocellular carcinoma is associated with increased survival: results from a large cohort in the Netherlands. J Hepatol. 2015; 63:1156–63.
Article28. Trevisani F, De Notariis S, Rapaccini G, Farinati F, Benvegnu L, Zoli M, et al. Semiannual and annual surveillance of cirrhotic patients for hepatocellular carcinoma: effects on cancer stage and patient survival (Italian experience). Am J Gastroenterol. 2002; 97:734–44.
Article29. Wang JH, Chang KC, Kee KM, Chen PF, Yen YH, Tseng PL, et al. Hepatocellular carcinoma surveillance at 4- vs. 12-month intervals for patients with chronic viral hepatitis: a randomized study in community. Am J Gastroenterol. 2013; 108:416–24.
Article30. Lee YH, Choi KS, Jun JK, Suh M, Lee HY, Kim YN, et al. Costeffectiveness of liver cancer screening in adults at high risk for liver cancer in the republic of Korea. Cancer Res Treat. 2014; 46:223–33.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surveillance for hepatocellular carcinoma: It is time to move forward
- Surveillance of hepatocellular carcinoma: is only ultrasound enough?
- Current Status and Future Directions of Hepatocellular Carcinoma Surveillance Test Based on Cost-effective Analysis
- Current status of image-based surveillance in hepatocellular carcinoma
- National Cancer Screening Program for Hepatocellular Carcinoma