The Current Status of Intervention for Intermediate Coronary Stenosis in the Korean Percutaneous Coronary Intervention (K-PCI) Registry
- Affiliations
-
- 1Department of Cardiology, Konkuk University School of Medicine, Chungju, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Keimyung University Dongsan Hospital, Daegu, Korea.
- 3Division of Cardiology, Yonsei University College of Medicine, Gangnam Severance Hospital, Seoul, Korea.
- 4Department of Cardiology, Pusan National University Yangsan Hospital, Busan, Korea.
- 5Department of Cardiology, The Catholic University of Korea, Incheon St. Mary's Hospital, Incheon, Korea.
- 6Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea.
- 7Division of Cardiology, Department of Internal Medicine, Seoul National University College of Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical center, Seoul, Korea.
- 8Division of Cardiology, The Catholic University of Korea, St.Vincent's Hospital, Suwon, Korea.
- 9Division of Cardiology, Department of Internal Medicine, Kangwon National University School of Medicine, Kangwon National University Hospital, Chuncheon, Korea.
- 10Division of Cardiology, University of Inje College of Medicine, Inje University Heaundae Paik Hospital, Busan, Korea.
- 11Division of Cardiology, University of Inje College of Medicine, Busan Paik Hospital, Busan, Korea. jsjang71@gmail.com
- KMID: 2460527
- DOI: http://doi.org/10.4070/kcj.2019.0074
Abstract
- BACKGROUND AND OBJECTIVES
Intermediate coronary lesion that can be under- or over-estimated by visual estimation frequently results in stenting of functionally nonsignificant lesions or deferral of percutaneous coronary intervention (PCI) of significant lesions inappropriately. We evaluated current status of PCI for intermediate lesions from a standardized database in Korea.
METHODS
We analyzed the Korean percutaneous coronary intervention (K-PCI) registry data which collected a standardized PCI database of the participating hospitals throughout the country from January 1, 2014, through December 31, 2014. Intermediate lesion was defined as a luminal narrowing between 50% and 70% by visual estimation and then compared whether the invasive physiologic or imaging study was performed or not.
RESULTS
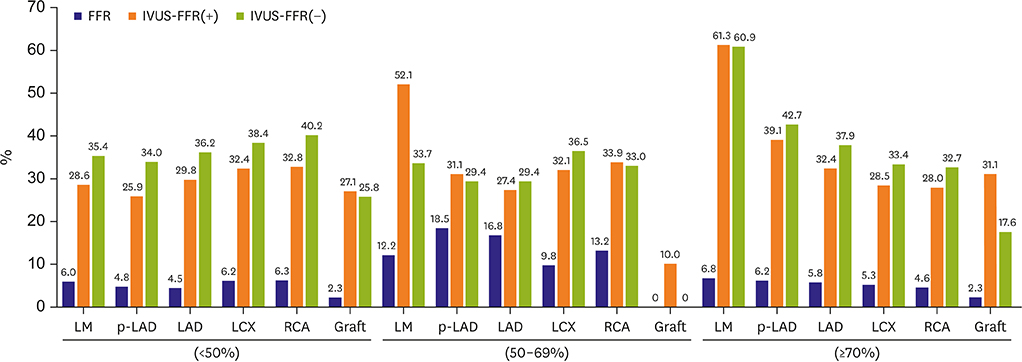
Physiology-guided PCI for intermediate lesions was performed in 16.8% for left anterior descending artery (LAD), 9.8% for left circumflex artery (LCX), 13.2% for right coronary artery (RCA). PCI was more frequently performed using intravascular ultrasound (IVUS) than using fractional flow reserve (FFR) for coronary artery segments (27.7% vs. 13.9% for LAD, 32.9% vs. 8.1% for LCX, and 33.8% vs. 10.8% for RCA). In accordance with or without FFR, PCI for intermediate lesions was more frequently performed in the hospitals with available FFR device than without FFR, especially in left main artery (LM), proximal LAD lesion (40.9% vs. 5.9% for LM, 24.6% vs 7.6% for proximal LAD).
CONCLUSIONS
These data provide the current PCI practice pattern with the use of FFR and IVUS in intermediate lesion. More common use of FFR for intermediate lesion should be encouraged.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Is Hospital Percutaneous Coronary Intervention Volume-In-hospital Outcome Relation an Issue in Acute Myocardial Infarction?
Seung-Woon Rha
Korean Circ J. 2020;50(11):1037-1039. doi: 10.4070/kcj.2020.0383.Would a Noninvasive Coronary Physiology Become a Standard and Popular Approach?
Yun-Kyeong Cho, Chang-Wook Nam
Korean Circ J. 2021;51(2):140-142. doi: 10.4070/kcj.2020.0511.Dose Coronary Angiography Suffice for Assessment of Intermediate Coronary Stenosis?
Sung Gyun Ahn, Sang Jun Lee
Korean Circ J. 2019;49(11):1033-1034. doi: 10.4070/kcj.2019.0227.Reduction of In-Stent Restenosis and Inflammation with One Stent: New Concept of Sirolimus and Ascorbic Acid-Eluting Coronary Stent
JiWung Ryu, Jung-Sun Kim
Korean Circ J. 2021;51(12):1015-1016. doi: 10.4070/kcj.2021.0336.Role of Novel Oral Anticoagulant for Patient with Atrial Fibrillation Underwent Percutaneous Coronary Intervention
Jang-Whan Bae
Cardiovasc Prev Pharmacother. 2019;1(1):19-29. doi: 10.36011/cpp.2019.1.e1.
Reference
-
1. Park SJ, Kang SJ, Ahn JM, et al. Visual-functional mismatch between coronary angiography and fractional flow reserve. JACC Cardiovasc Interv. 2012; 5:1029–1036.
Article2. Trask N, Califf RM, Conley MJ, et al. Accuracy and interobserver variability of coronary cineangiography: a comparison with postmortem evaluation. J Am Coll Cardiol. 1984; 3:1145–1154.
Article3. Katritsis D, Webb-Peploe M. Limitations of coronary angiography: an underestimated problem? Clin Cardiol. 1991; 14:20–24.
Article4. Patel MR, Calhoon JH, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 appropriate use criteria for coronary revascularization in patients with stable ischemic heart disease: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2017; 69:2212–2241.5. Authors/Task Force members. Windecker S, Kolh P, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014; 35:2541–2619.6. Pijls NH, van Schaardenburgh P, Manoharan G, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol. 2007; 49:2105–2111.7. Safi M, Mehrabi MA, Alipour Parsa S, Khaheshi I, Naderian M. The role of FFR in clinical decision making in patients with moderate coronary lesions: a pilot study. Acta Biomed. 2018; 89:378–381.8. Parise H, Maehara A, Stone GW, Leon MB, Mintz GS. Meta-analysis of randomized studies comparing intravascular ultrasound versus angiographic guidance of percutaneous coronary intervention in pre-drug-eluting stent era. Am J Cardiol. 2011; 107:374–382.
Article9. Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009; 360:213–224.
Article10. Jang JS, Song YJ, Kang W, et al. Intravascular ultrasound-guided implantation of drug-eluting stents to improve outcome: a meta-analysis. JACC Cardiovasc Interv. 2014; 7:233–243.11. Jang JS, Han KR, Moon KW, et al. The current status of percutaneous coronary intervention in Korea: based on year 2014 cohort of Korean percutaneous coronary intervention (K-PCI) registry. Korean Circ J. 2017; 47:328–340.
Article12. Gwon HC, Jeon DW, Kang HJ, et al. The practice pattern of percutaneous coronary intervention in Korea: based on year 2014 cohort of Korean percutaneous coronary intervention (K-PCI) registry. Korean Circ J. 2017; 47:320–327.
Article13. Pothineni NV, Shah NN, Rochlani Y, et al. U.S. trends in inpatient utilization of fractional flow reserve and percutaneous coronary intervention. J Am Coll Cardiol. 2016; 67:732–733.
Article14. Ahn JM, Park DW, Shin ES, et al. Fractional flow reserve and cardiac events in coronary artery disease: data from a prospective IRIS-FFR registry (Interventional Cardiology Research Incooperation Society Fractional Flow Reserve). Circulation. 2017; 135:2241–2251.15. Dattilo PB, Prasad A, Honeycutt E, Wang TY, Messenger JC. Contemporary patterns of fractional flow reserve and intravascular ultrasound use among patients undergoing percutaneous coronary intervention in the United States: insights from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2012; 60:2337–2339.16. Tanaka N, Kohsaka S, Murata T, et al. Treatment strategy modification and its implication on the medical cost of fractional flow reserve-guided percutaneous coronary intervention in Japan. J Cardiol. 2019; 73:38–44.
Article17. Hong SJ, Kim BK, Shin DH, et al. Effect of intravascular ultrasound-guided vs angiography-guided everolimus-eluting stent implantation: the IVUS-XPL randomized clinical trial. JAMA. 2015; 314:2155–2163.18. Witzenbichler B, Maehara A, Weisz G, et al. Relationship between intravascular ultrasound guidance and clinical outcomes after drug-eluting stents: the assessment of dual antiplatelet therapy with drug-eluting stents (ADAPT-DES) study. Circulation. 2014; 129:463–470.19. Inohara T, Kohsaka S, Miyata H, et al. Appropriateness ratings of percutaneous coronary intervention in Japan and its association with the trend of noninvasive testing. JACC Cardiovasc Interv. 2014; 7:1000–1009.20. Cho YK, Nam CW, Han JK, et al. Usefulness of combined intravascular ultrasound parameters to predict functional significance of coronary artery stenosis and determinants of mismatch. EuroIntervention. 2015; 11:163–170.
Article21. Han JK, Koo BK, Park KW, et al. Optimal intravascular ultrasound criteria for defining the functional significance of intermediate coronary stenosis: an international multicenter study. Cardiology. 2014; 127:256–262.
Article22. Jang JS, Shin HC, Bae JS, et al. Diagnostic performance of intravascular ultrasound-derived minimal Lumen area to predict functionally significant non-left main coronary artery disease: a meta-analysis. Korean Circ J. 2016; 46:622–631.
Article23. De Bruyne B, Fearon WF, Pijls NH, et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med. 2014; 371:1208–1217.
Article24. Xaplanteris P, Fournier S, Pijls NHJ, et al. Five-year outcomes with PCI guided by fractional flow reserve. N Engl J Med. 2018; 379:250–259.
Article25. Chen ZW, Yu ZQ, Yang HB, et al. Rapid predictors for the occurrence of reduced left ventricular ejection fraction between LAD and non-LAD related ST-elevation myocardial infarction. BMC Cardiovasc Disord. 2016; 16:3.
Article26. Fearon WF, Bornschein B, Tonino PA, et al. Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. Circulation. 2010; 122:2545–2550.
Article27. Fearon WF, Nishi T, De Bruyne B, et al. Clinical outcomes and cost-effectiveness of fractional flow reserve-guided percutaneous coronary intervention in patients with stable coronary artery disease: three-year follow-up of the FAME 2 trial (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation). Circulation. 2018; 137:480–487.28. Nam CW, Yoon HJ, Cho YK, et al. Outcomes of percutaneous coronary intervention in intermediate coronary artery disease: fractional flow reserve-guided versus intravascular ultrasound-guided. JACC Cardiovasc Interv. 2010; 3:812–817.29. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011; 58:e44–122.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of Coronary Intervention in Patients with ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease
- Percutaneous Coronary Intervention and Coronary Artery Bypass Grafting for the Treatment of Left Main Coronary Artery Disease
- Recent Advances in Percutaneous Coronary Intervention in Coronary Artery Disease
- The Second Report from K-PCI Registry: a Step toward Continuous Systemic Monitoring of Korean Percutaneous Coronary Intervention Practice
- Percutaneous coronary intervention in patients with multi-vessel coronary artery disease: a focus on physiology