Yeungnam Univ J Med.
2019 Sep;36(3):260-264. 10.12701/yujm.2019.00241.
Late complication of the Nuss procedure: recurrent cardiac tamponade
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Dong-Eui Medical Center, Busan, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea. gubjae@hanmail.net
- 3Division of Cardiology, Department of Internal Medicine, Daegu Veterans Hospital, Daegu, Korea.
- 4Division of Cardiology, Department of Internal Medicine, Pohang SM Christianity Hospital, Pohang, Korea.
- 5Division of Cardiology, Department of Internal Medicine, Dongguk University Gyeongju Hospital, Gyeongju, Korea.
- 6Department of Emergency Medicine, Yeungnam University Medical Center, Daegu, Korea.
- KMID: 2460196
- DOI: http://doi.org/10.12701/yujm.2019.00241
Abstract
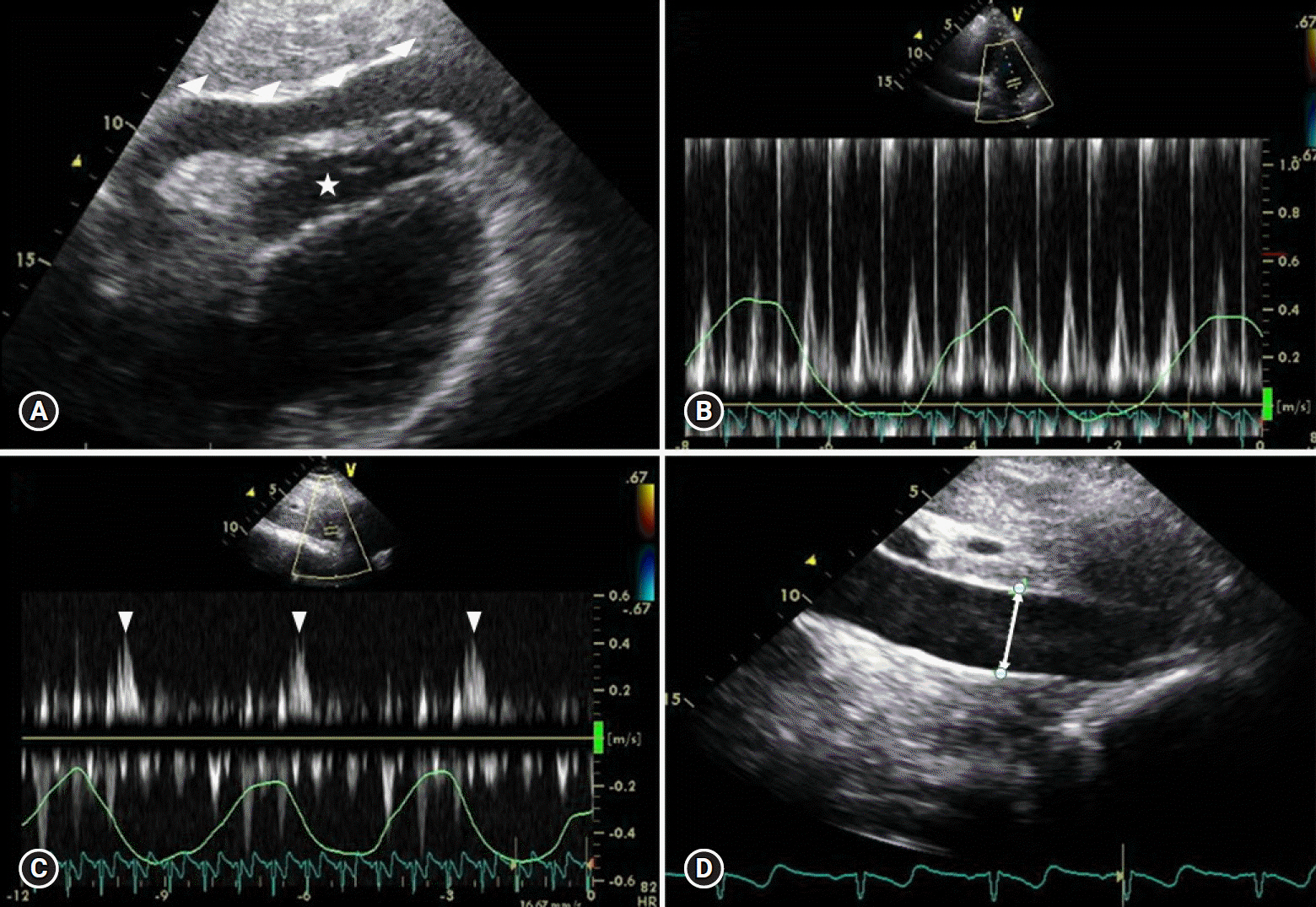
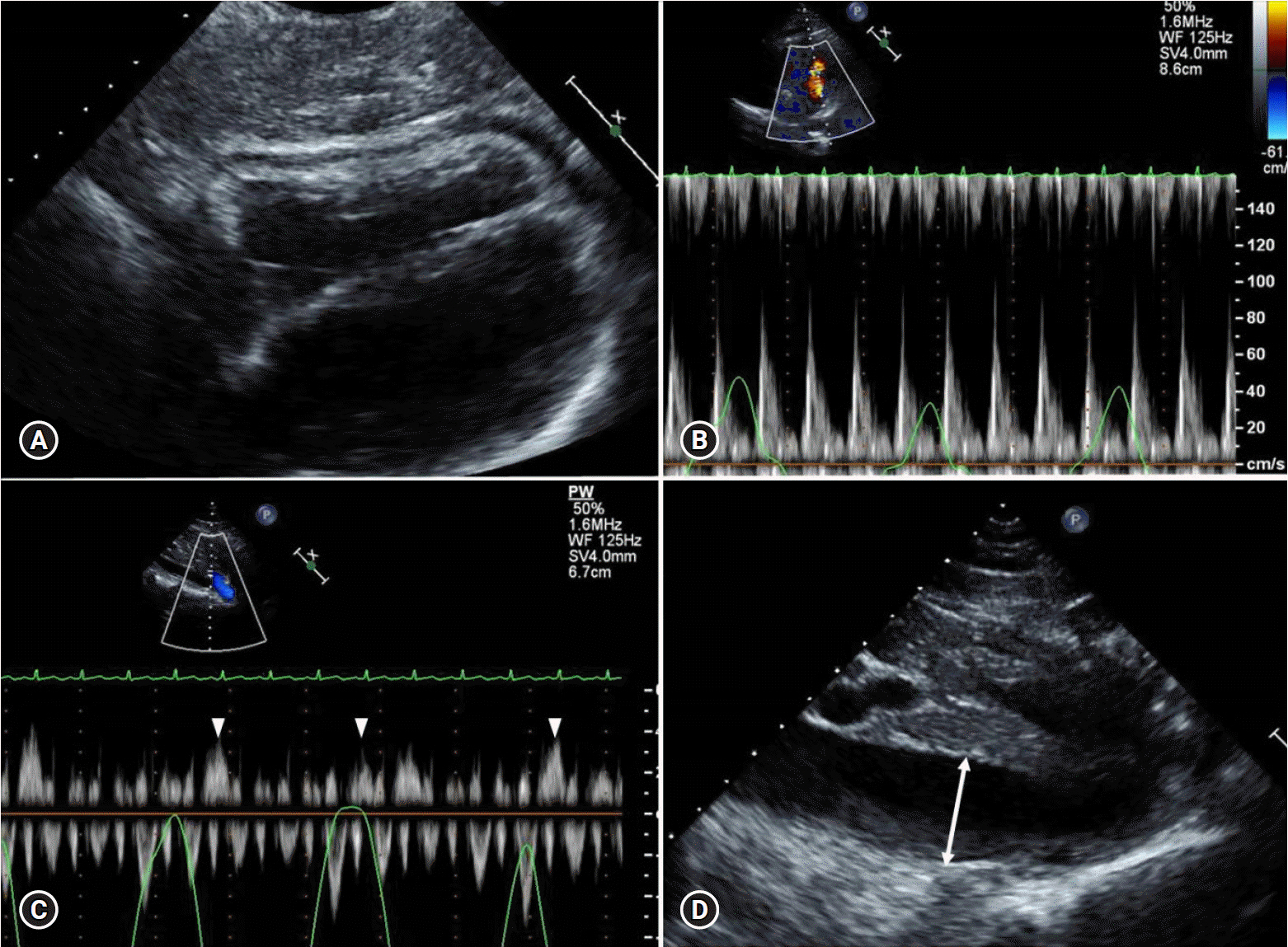
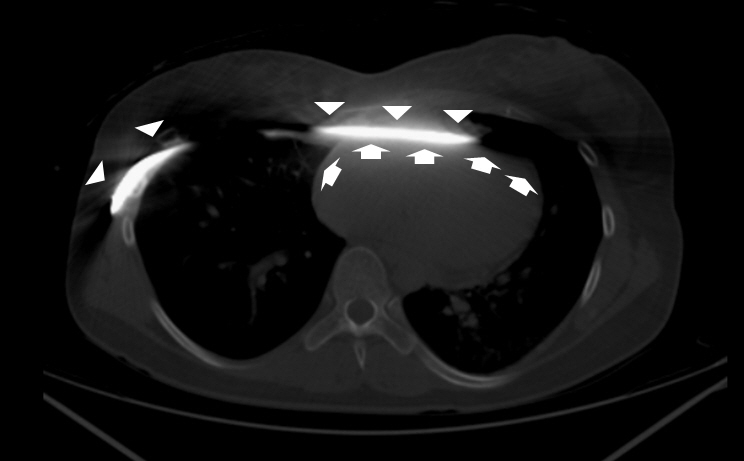
- Pectus excavatum (PE) is known as one of the most common congenital deformities of the anterior chest wall. The Nuss procedure is an effective surgical therapy to correct PE. Here, we report a case of recurrent cardiac tamponade due to hemopericardium that occurred after 16 months following the Nuss procedure. The cause of recurrent hemopericardium was thought to be local, repetitive irritation of the pericardium by the Nuss steel bar. We should keep in mind that this serious complication can occur after the Nuss procedure, even in the late phase.
MeSH Terms
Figure
Reference
-
References
1. Jaroszewski DE, Fonkalsrud EW. Repair of pectus chest deformities in 320 adult patients: 21 year experience. Ann Thorac Surg. 2007; 84:429–33.
Article2. Nuss D, Kelly RE Jr, Croitoru DP, Katz ME. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg. 1998; 33:545–52.
Article3. Krasopoulos G, Goldstraw P. Minimally invasive repair of pectus excavatum deformity. Eur J Cardiothorac Surg. 2011; 39:149–58.
Article4. Žganjer M, Žganjer V. Surgical correction of the funnel chest deformity in children. Int Orthop. 2011; 35:1043–8.
Article5. Yoon YS, Kim HK, Choi YS, Kim K, Shim YM, Kim J. A modified Nuss procedure for late adolescent and adult pectus excavatum. World J Surg. 2010; 34:1475–80.
Article6. Park HJ, Lee SY, Lee CS, Youm W, Lee KR. The Nuss procedure for pectus excavatum: evolution of techniques and early results on 322 patients. Ann Thorac Surg. 2004; 77:289–95.
Article7. Johnson WR, Fedor D, Singhal S. A novel approach to eliminate cardiac perforation in the Nuss procedure. Ann Thorac Surg. 2013; 95:1109–11.
Article8. Kelly RE Jr, Mellins RB, Shamberger RC, Mitchell KK, Lawson ML, Oldham KT, et al. Multicenter study of pectus excavatum, final report: complications, static/exercise pulmonary function, and anatomic outcomes. J Am Coll Surg. 2013; 217:1080–9.
Article9. Fallon SC, Slater BJ, Nuchtern JG, Cass DL, Kim ES, Lopez ME, et al. Complications related to the Nuss procedure: minimizing risk with operative technique. J Pediatr Surg. 2013; 48:1044–8.
Article10. Barakat MJ, Morgan JA. Haemopericardium causing cardiac tamponade: a late complication of pectus excavatum repair. Heart. 2004; 90:e22.
Article11. Cope SA, Rodda J. Cardiac tamponade presenting to the emergency department after sternal wire disruption. Emerg Med J. 2004; 21:389–90.
Article12. Lee SH, Cho BS, Kim SJ, Lee SY, Kang MH, Han GS, et al. Cardiac tamponade caused by broken sternal wire after pectus excavatum repair: a case report. Ann Thorac Cardiovasc Surg. 2013; 19:52–4.
Article13. Hoel TN, Rein KA, Svennevig JL. A life-threatening complication of the Nuss procedure for pectus excavatum. Ann Thorac Surg. 2006; 81:370–2.14. Yang MH, Cheng YL, Tsai CS, Li CY. Delayed cardiac tamponade after the Nuss procedure for pectus excavatum: a case report and simple management. Heart Surg Forum. 2008; 11:E129–31.
Article15. Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003; 349:684–90.
Article16. Gascho JA, Martins JB, Marcus ML, Kerber RE. Effects of volume expansion and vasodilators in acute pericardial tamponade. Am J Physiol. 1981; 240:H49–53.
Article17. Spodick DH. The normal and diseased pericardium: current concepts of pericardial physiology, diagnosis and treatment. J Am Coll Cardiol. 1983; 1:240–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiac Tamponade Associated with Acupuncture
- Recurrent Cardiac Tamponade Complicated by Coronary Intervention
- Embarrassed Radiofrequency Catheter Ablation of Supraventricular Tachycardia in Pectus Excavatum
- Cardiac Tamponade during Endovascular Repair of Thoracic Aortic Dissection
- A Case of Cardiac Tamponade in a Patient with Rheumatoid Arthritis