Yeungnam Univ J Med.
2019 Sep;36(3):208-218. 10.12701/yujm.2019.00192.
Feasibility and efficacy of coil embolization for middle cerebral artery aneurysms
- Affiliations
-
- 1Department of Neurosurgery, Kosin University Gospel Hospital, Busan, Korea.
- 2Department of Neurosurgery, Pusan National University Hospital, Busan, Korea. chwachoi@pusan.ac.kr
- 3Department of Diagnostic Radiology, Pusan National University Hospital, Busan, Korea.
- KMID: 2460189
- DOI: http://doi.org/10.12701/yujm.2019.00192
Abstract
- BACKGROUND
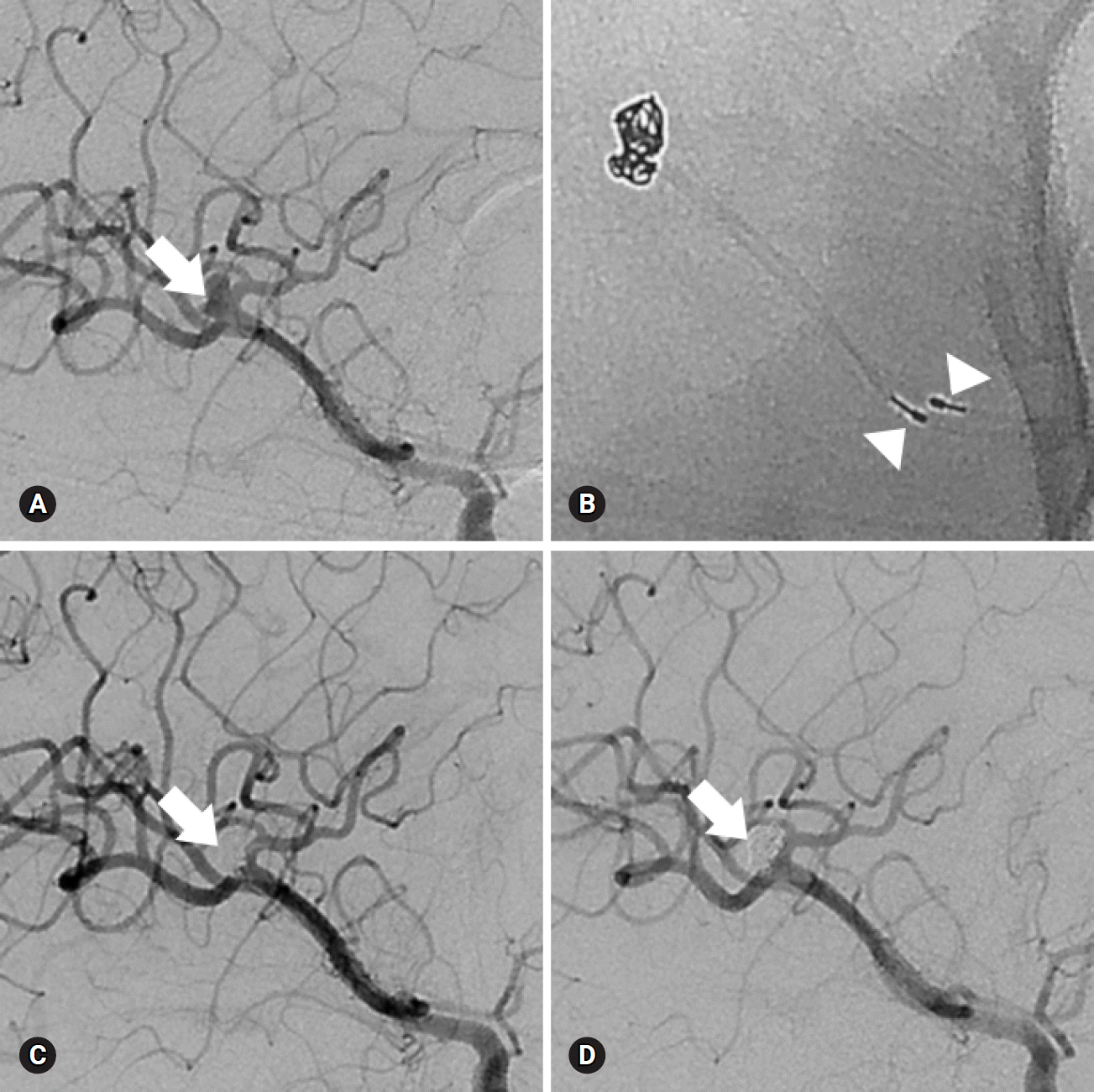
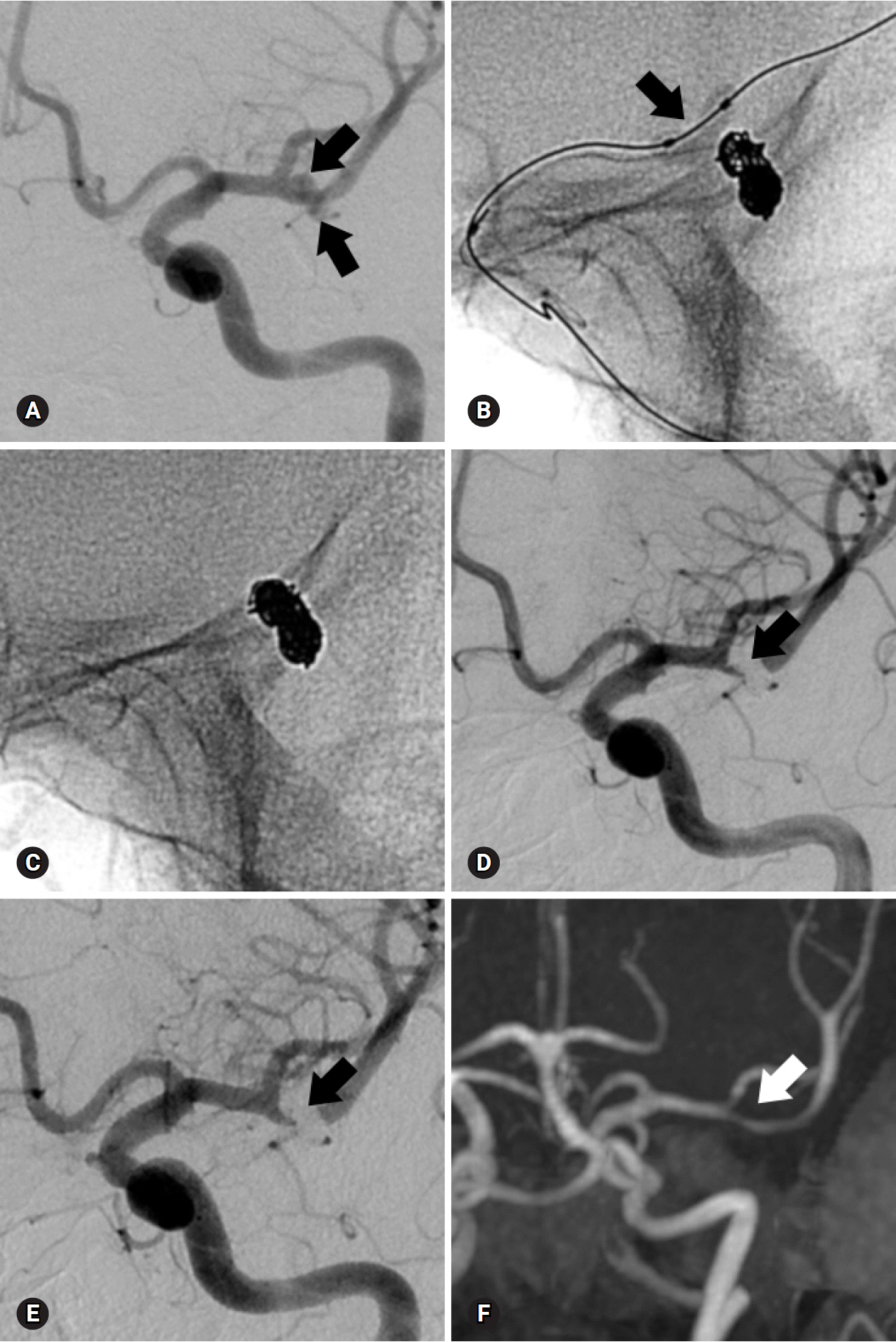
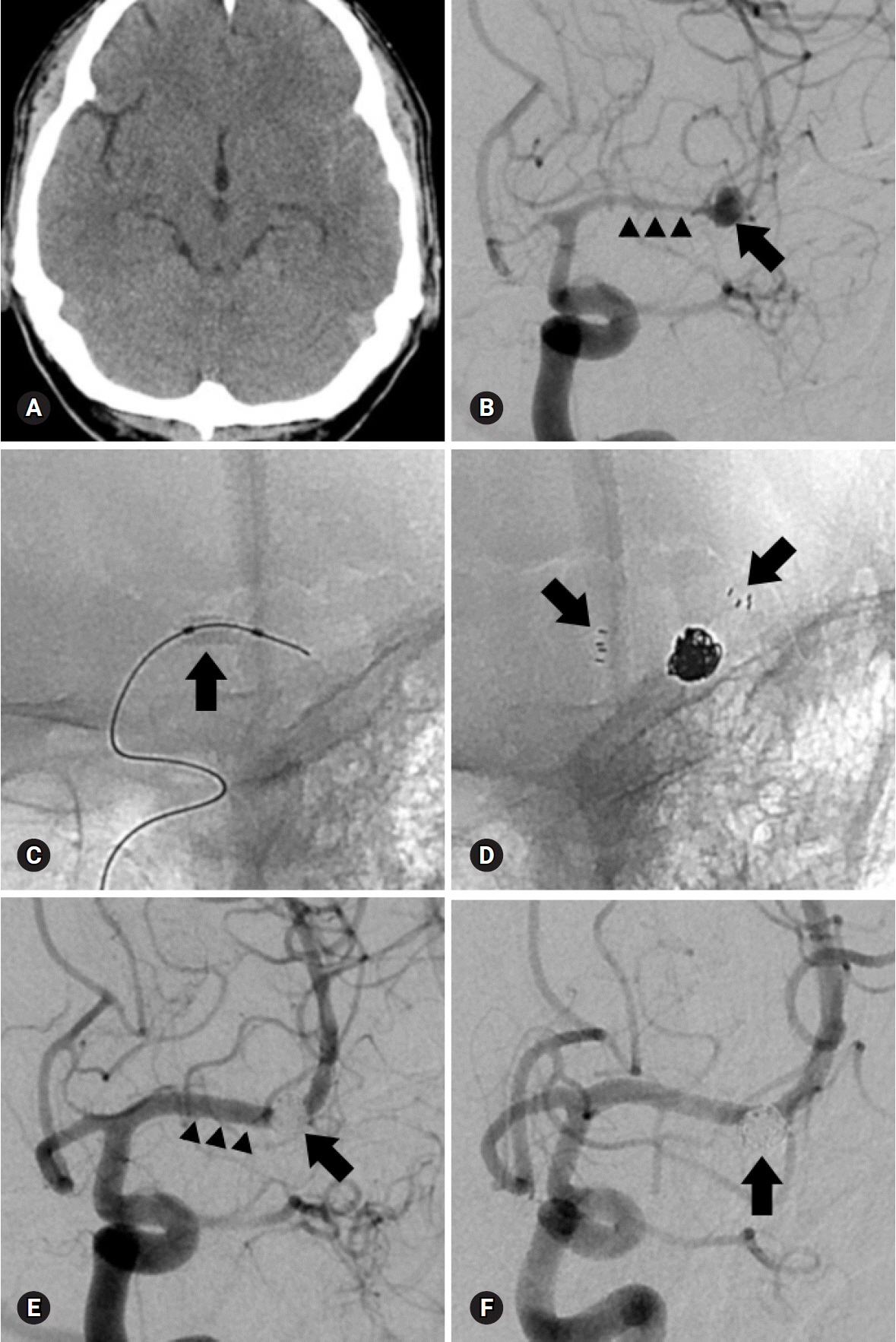
The anatomy of middle cerebral artery (MCA) aneurysms has been noted to be unfavorable for endovascular treatment. The purpose of this study was to assess the feasibility and efficacy of coiling for MCA aneurysms.
METHODS
From January 2004 to December 2015, 72 MCA aneurysms (38 unruptured and 34 ruptured) in 67 patients were treated with coils. Treatment-related complications, clinical outcomes, and immediate and follow-up angiographic outcomes were retrospectively analyzed.
RESULTS
Aneurysms were located at the MCA bifurcation (n=60), 1st segment (M1, n=8), and 2nd segment (M2, n=4). Sixty-nine aneurysms (95.8%) were treated by neck remodeling techniques using multi-catheter (n=44), balloon (n=14), stent (n=8), or combination of these (n=3). Only 3 aneurysms were treated by single-catheter technique. Angiographic results were 66 (91.7%) complete, 5 (6.9%) remnant neck, and 1 (1.4%) incomplete occlusion. Procedural complications included aneurysm rupture (n=1), asymptomatic coil migration to the distal vessel (n=1), and acute thromboembolism (n=10) consisting of 8 asymptomatic and 2 symptomatic events. Treatment-related permanent morbidity and mortality rates were 4.5% and 3.0%, respectively. There was no bleeding on clinical follow-up (mean, 29 months; range, 6-108 months). Follow-up angiographic results (mean, 26 months; range, 6-96 months) in patients included 1 major and 3 minor recanalizations.
CONCLUSION
Coiling of MCA aneurysms could be a technically feasible and clinically effective treatment strategy with acceptable angiographic and clinical outcomes. However, the safety and efficacy of this technique as compared to surgical clipping remains to be ascertained.
MeSH Terms
Figure
Reference
-
References
1. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 2002; 360:1267–74.
Article2. Regli L, Uske A, de Tribolet N. Endovascular coil placement compared with surgical clipping for the treatment of unruptured middle cerebral artery aneurysms: a consecutive series. J Neurosurg. 1999; 90:1025–30.
Article3. Regli L, Dehdashti AR, Uske A, de Tribolet N. Endovascular coiling compared with surgical clipping for the treatment of unruptured middle cerebral artery aneurysms: an update. Acta Neurochir Suppl. 2002; 82:41–6.
Article4. Raftopoulos C, Mathurin P, Boscherini D, Billa RF, van Boven M, Hantson P. Prospective analysis of aneurysm treatment in a series of 103 consecutive patients when endovascular embolization is considered the first option. J Neurosurg. 2000; 93:175–82.
Article5. Iijima A, Piotin M, Mounayer C, Spelle L, Weill A, Moret J. Endovascular treatment with coils of 149 middle cerebral artery berry aneurysms. Radiology. 2005; 237:611–9.
Article6. Doerfler A, Wanke I, Goericke SL, Wiedemayer H, Engelhorn T, Gizewski ER, et al. Endovascular treatment of middle cerebral artery aneurysms with electrolytically detachable coils. AJNR Am J Neuroradiol. 2006; 27:513–20.7. Quadros RS, Gallas S, Noudel R, Rousseaux P, Pierot L. Endovascular treatment of middle cerebral artery aneurysms as first option: a single center experience of 92 aneurysms. AJNR Am J Neuroradiol. 2007; 28:1567–72.
Article8. Horowitz M, Gupta R, Gologorsky Y, Jovin T, Genevro J, Levy E, et al. Clinical and anatomic outcomes after endovascular coiling of middle cerebral artery aneurysms: report on 30 treated aneurysms and review of the literature. Surg Neurol. 2006; 66:167–71.
Article9. Kim J, Chang C, Jung Y. Feasibility and midterm outcomes of endovascular coil embolization of an unruptured middle cerebral artery aneurysm with an incorporated branch. World Neurosurg. 2018; 118:e745–52.
Article10. Kim BM, Park SI, Kim DJ, Kim DI, Suh SH, Kwon TH, et al. Endovascular coil embolization of aneurysms with a branch incorporated into the sac. AJNR Am J Neuroradiol. 2010; 31:145–51.
Article11. Lubicz B, Leclerc X, Gauvrit JY, Lejeune JP, Pruvo JP. HyperForm remodeling-balloon for endovascular treatment of wide-neck intracranial aneurysms. AJNR Am J Neuroradiol. 2004; 25:1381–3.12. Lubicz B, Lefranc F, Levivier M, Dewitte O, Pirotte B, Brotchi J, et al. Endovascular treatment of intracranial aneurysms with a branch arising from the sac. AJNR Am J Neuroradiol. 2006; 27:142–7.13. Roy D, Milot G, Raymond J. Endovascular treatment of unruptured aneurysms. Stroke. 2001; 32:1998–2004.
Article14. Ausman JI. The future of neurovascular surgery. Part I: intracranial aneurysms. Surg Neurol. 1997; 48:98–100.
Article15. Suzuki S, Tateshima S, Jahan R, Duckwiler GR, Murayama Y, Gonzalez NR, et al. Endovascular treatment of middle cerebral artery aneurysms with detachable coils: angiographic and clinical outcomes in 115 consecutive patients. Neurosurgery. 2009; 64:876–88.16. Bracard S, Abdel-Kerim A, Thuillier L, Klein O, Anxionnat R, Finitsis S, et al. Endovascular coil occlusion of 152 middle cerebral artery aneurysms: initial and midterm angiographic and clinical results. J Neurosurg. 2010; 112:703–8.
Article17. Jayaraman MV, Do HM, Versnick EJ, Steinberg GK, Marks MP. Morphologic assessment of middle cerebral artery aneurysms for endovascular treatment. J Stroke Cerebrovasc Dis. 2007; 16:52–6.
Article18. Higashida RT, Lahue BJ, Torbey MT, Hopkins LN, Leip E, Hanley DF. Treatment of unruptured intracranial aneurysms: a nationwide assessment of effectiveness. AJNR Am J Neuroradiol. 2007; 28:146–51.19. van Rooij WJ, Sluzewski M. Procedural morbidity and mortality of elective coil treatment of unruptured intracranial aneurysms. AJNR Am J Neuroradiol. 2006; 27:1678–80.20. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005; 366:809–17.
Article21. Choi JH, Park JE, Kim MJ, Kim BS, Shin YS. Aneurysmal neck clipping as the primary treatment option for both ruptured and unruptured middle cerebral artery aneurysms. J Korean Neurosurg Soc. 2016; 59:269–75.
Article22. Brinjikji W, Lanzino G, Cloft HJ, Rabinstein A, Kallmes DF. Endovascular treatment of middle cerebral artery aneurysms: a systematic review and single-center series. Neurosurgery. 2011; 68:397–402.23. Kim SR, Vora N, Jovin TG, Gupta R, Thomas A, Kassam A, et al. Anatomic results and complications of stent-assisted coil embolization of intracranial aneurysms. Interv Neuroradiol. 2008; 14:267–84.
Article24. Nishido H, Piotin M, Bartolini B, Pistocchi S, Redjem H, Blanc R. Analysis of complications and recurrences of aneurysm coiling with special emphasis on the stent-assisted technique. AJNR Am J Neuroradiol. 2014; 35:339–44.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Single-session Coil Embolization of Multiple Intracranial Aneurysms
- Recent Trends in the Treatment of Cerebral Aneurysms: Comparison between Endovascular Coil Embolization and Surgical Clipping
- Endovascular Coil Embolization After Clipping: Endovascular Treatment of Incompletely Clipped or Recurred Cerebral Aneurysms
- Complications of Endovascular Detachable Coil Treatment in Cerebral Aneurysms
- Coil Embolization for Distal Middle Cerebral Artery Aneurysm