Investig Magn Reson Imaging.
2019 Sep;23(3):251-258. 10.13104/imri.2019.23.3.251.
Feasibility of Spin-Echo Echo-Planar Imaging MR Elastography in Livers of Children and Young Adults
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul, Korea. lamer-22@yuhs.ac
- 2Department of Radiology, Research Institute of Radiological Science, Center for Clinical Imaging Data Science, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Pediatric Gastroenterology, Hepatology and Nutrition, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Pediatric Surgery, Yonsei University College of Medicine, Seoul, Korea.
- 5Severance Pediatric Liver Disease Research Group, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2459879
- DOI: http://doi.org/10.13104/imri.2019.23.3.251
Abstract
- PURPOSE
To assess the feasibility of the use of spin-echo echo-planar imaging (SE-EPI) magnetic resonance elastography (MRE) in livers of children and young adults.
MATERIALS AND METHODS
Patients (≤ 20 years old) who underwent 3T SE-EPI MRE were included retrospectively. Subjects were divided into three groups according to the purpose of the liver MRI: suspicion of fatty liver or focal fat deposition in the liver (FAT group), liver fibrosis after receiving a Kasai operation from biliary atresia (BA group), and hepatic iron deposition after receiving chemotherapy or transfusions (IRON group). Technical failure of MRE was defined when a stiffness map showed no pixel value with a confidence index higher than 95%, and the patients were divided as success and failure groups accordingly. Clinical findings including age, gender, weight, height, and body mass index and magnetic resonance imaging results including proton density fat fraction (PDFF), T2*, and MRE values were assessed. Factors affecting failure of MRE were evaluated and the image quality in wave propagation image and stiffness map was evaluated using the appropriate scores.
RESULTS
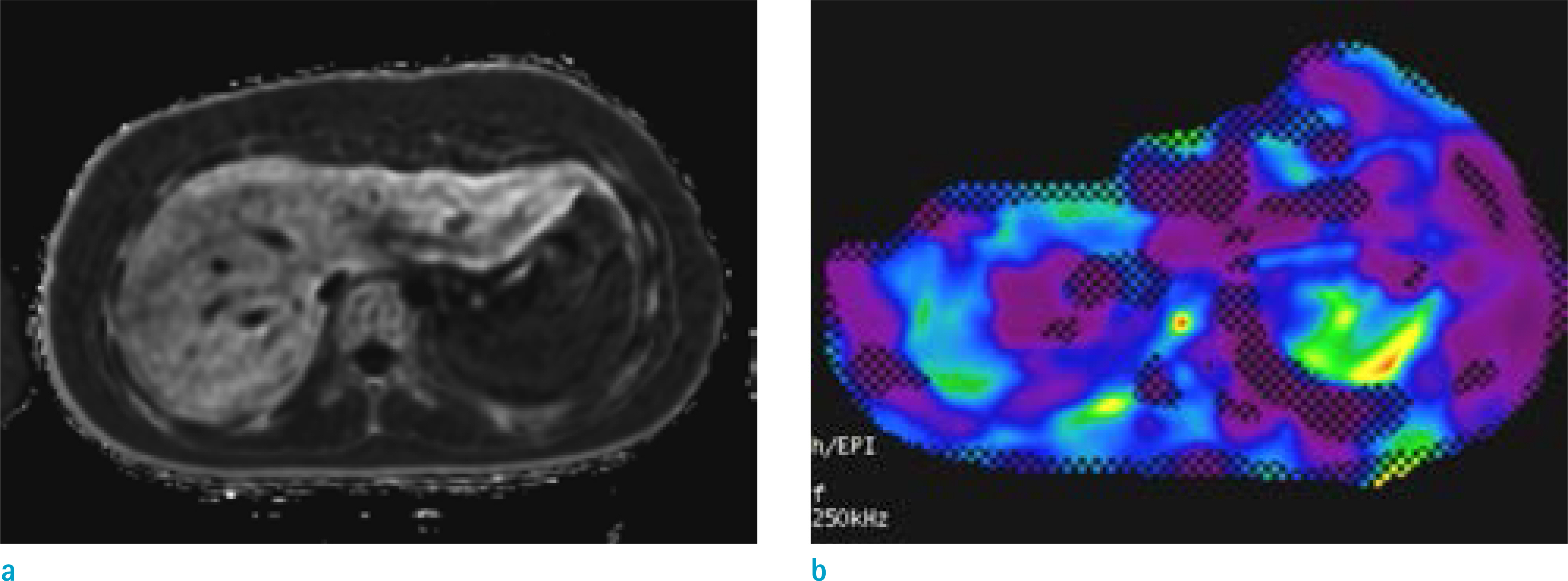
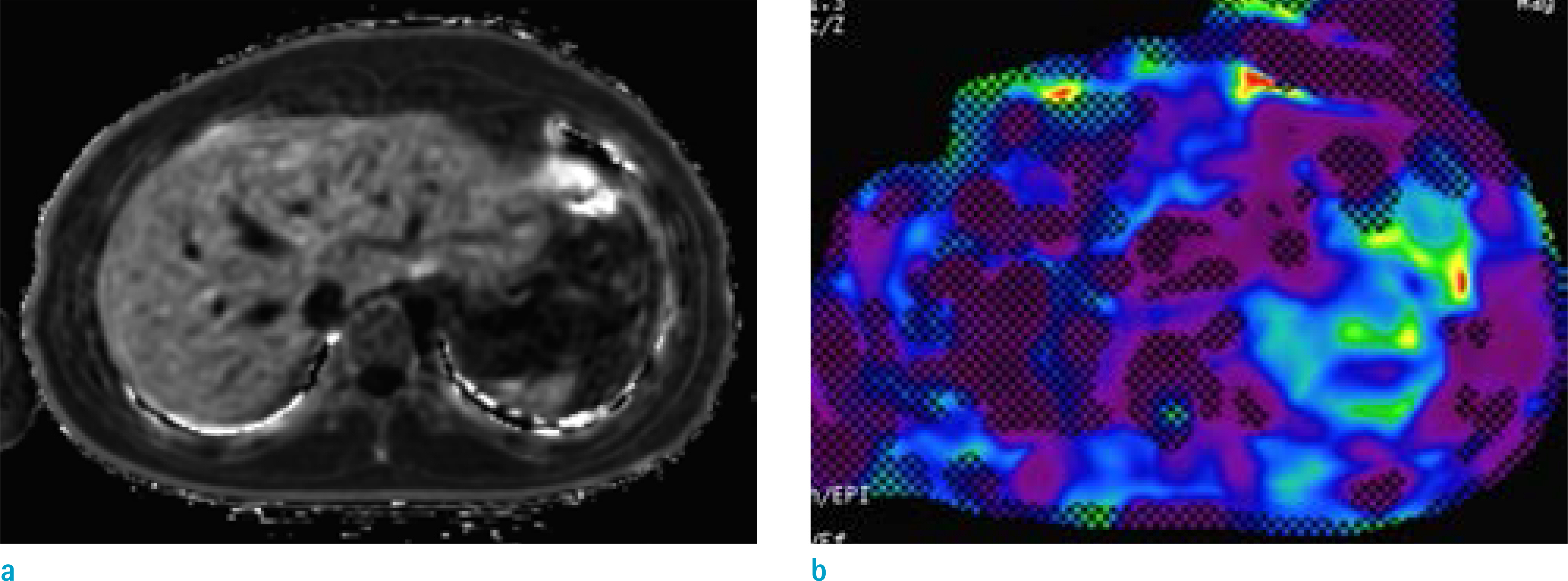
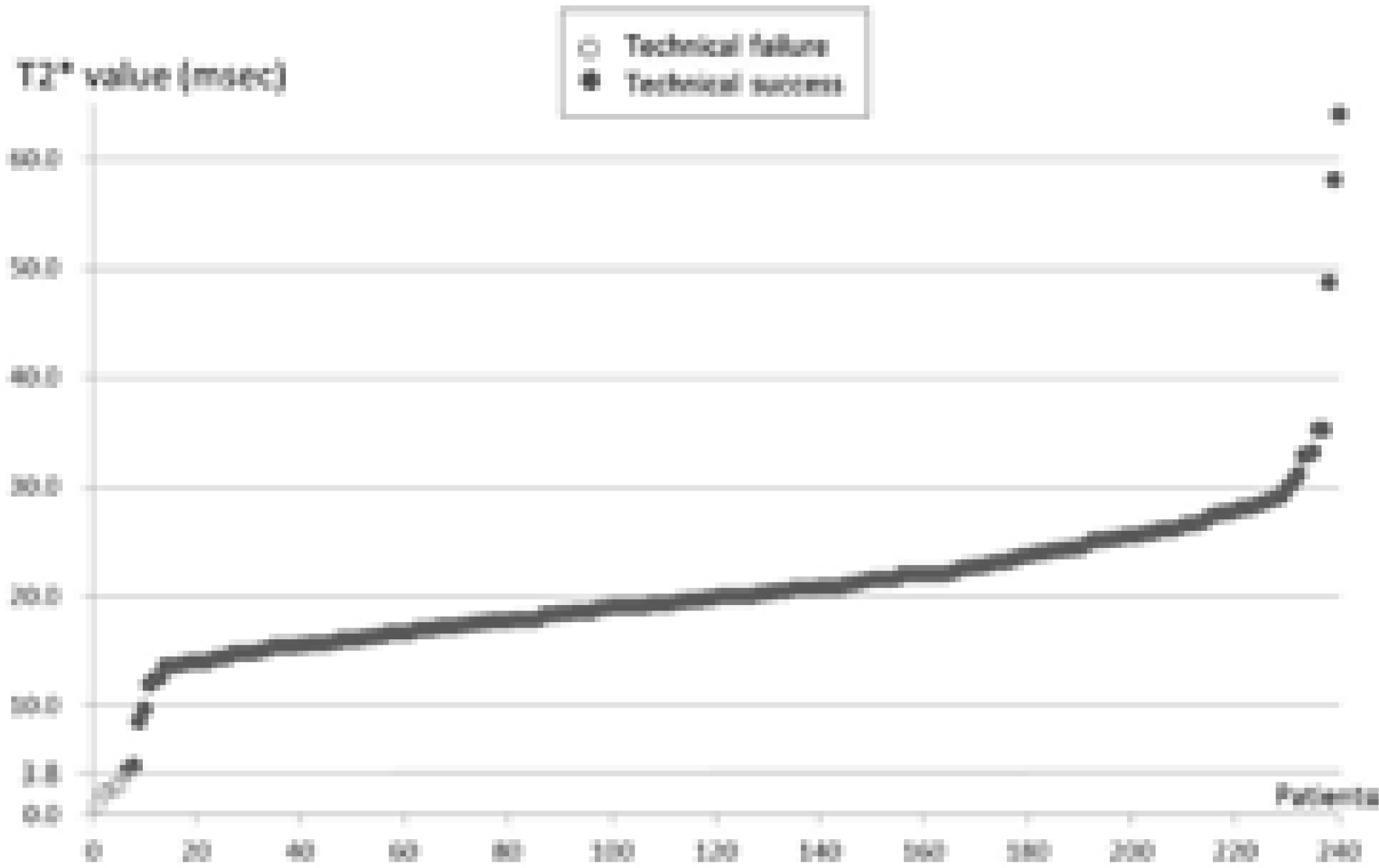
Among total 240 patients (median 15 years, 211 patients in the FAT, 21 patients in the BA, and 8 patients in the IRON groups), technical failure was noted in six patients in the IRON group (6/8 patients, 75%), while there were no failures noted in the FAT and BA groups. These six patients had T2* values ranging from 0.9 to 3.8 ms. The image quality scores were not significantly different between the FAT and BA groups (P > 0.999), while the scores were significantly lower in the IRON group (P < 0.001).
CONCLUSION
The 3T SE-EPI MRE in children and young adults had a high technical success rate. The technical failure was occurred in children with decreased T2* value (≤ 3.8 ms) from iron deposition.
MeSH Terms
Figure
Reference
-
References
1. Bonekamp S, Kamel I, Solga S, Clark J. Can imaging modalities diagnose and stage hepatic fibrosis and cirrhosis accurately? J Hepatol. 2009; 50:17–35.
Article2. Mavis AM, Alonso EM. Liver disease in the adolescent. Clin Liver Dis. 2015; 19:171–185.
Article3. Friedman SL. Evolving challenges in hepatic fibrosis. Nat Rev Gastroenterol Hepatol. 2010; 7:425–436.
Article4. Bortolotti F, Guido M. Reversal of liver cirrhosis: a desirable clinical outcome and its pathogenic background. J Pediatr Gastroenterol Nutr. 2007; 44:401–406.
Article5. Castera L, Pinzani M. Biopsy and non-invasive methods for the diagnosis of liver fibrosis: does it take two to tango? Gut. 2010; 59:861–866.
Article6. Pariente D, Franchi-Abella S. Paediatric chronic liver diseases: how to investigate and follow up? Role of imaging in the diagnosis of fibrosis. Pediatr Radiol. 2010; 40:906–919.
Article7. Kennedy P, Wagner M, Castera L, et al. Quantitative elastography methods in liver disease: current evidence and future directions. Radiology. 2018; 286:738–763.
Article8. Trout AT, Sheridan RM, Serai SD, et al. Diagnostic performance of MR elastography for liver fibrosis in children and young adults with a spectrum of liver diseases. Radiology. 2018; 287:824–832.
Article9. Singh S, Venkatesh SK, Wang Z, et al. Diagnostic performance of magnetic resonance elastography in staging liver fibrosis: a systematic review and metaanalysis of individual participant data. Clin Gastroenterol Hepatol. 2015; 13:440–451. e446.
Article10. Serai SD, Dillman JR, Trout AT. Spin-echo echoplanar imaging MR elastography versus gradient-echo MR elastography for assessment of liver stiffness in children and young adults suspected of having liver disease. Radiology. 2017; 282:761–770.
Article11. Kim YS, Jang YN, Song JS. Comparison of gradient-recalled echo and spin-echo echoplanar imaging MR elastography in staging liver fibrosis: a metaanalysis. Eur Radiol. 2018; 28:1709–1718.
Article12. Felker ER, Choi KS, Sung K, et al. Liver MR elastography at 3 T: agreement across pulse sequences and effect of liver R2* on image quality. AJR Am J Roentgenol. 2018; 211:588–594.
Article13. Wagner M, Corcuera-Solano I, Lo G, et al. Technical failure of MR elastography examinations of the liver: experience from a large singlecenter study. Radiology. 2017; 284:401–412.14. Joshi M, Dillman JR, Towbin AJ, Serai SD, Trout AT. MR elastography: high rate of technical success in pediatric and young adult patients. Pediatr Radiol. 2017; 47:838–843.
Article15. Alustiza Echeverria JM, Castiella A, Emparanza JI. Quantification of iron concentration in the liver by MRI. Insights Imaging. 2012; 3:173–180.
Article16. Shin HJ, Kim HG, Kim MJ, et al. Normal range of hepatic fat fraction on dual- and triple-echo fat quantification MR in children. PLoS One. 2015; 10:e0117480.
Article17. Wahidiyat PA, Iskandar SD, Sekarsari D. Evaluation of iron overload between age groups using magnetic resonance imaging and its correlation with iron profile in transfusion-dependent thalassemia. Acta Med Indones. 2018; 50:230–236.18. Serai SD, Towbin AJ, Podberesky DJ. Pediatric liver MR elastography. Dig Dis Sci. 2012; 57:2713–2719.
Article19. Binkovitz LA, El-Youssef M, Glaser KJ, Yin M, Binkovitz AK, Ehman RL. Pediatric MR elastography of hepatic fibrosis: principles, technique and early clinical experience. Pediatr Radiol. 2012; 42:402–409.
Article20. Petitclerc L, Sebastiani G, Gilbert G, Cloutier G, Tang A. Liver fibrosis: review of current imaging and MRI quantification techniques. J Magn Reson Imaging. 2017; 45:1276–1295.
Article21. Mariappan YK, Glaser KJ, Ehman RL. Magnetic resonance elastography: a review. Clin Anat. 2010; 23:497–511.
Article22. Srinivasa Babu A, Wells ML, Teytelboym OM, et al. Elastography in chronic liver disease: modalities, techniques, limitations, and future directions. Radiographics. 2016; 36:1987–2006.
Article23. Wagner M, Besa C, Bou Ayache J, et al. Magnetic resonance elastography of the liver: qualitative and quantitative comparison of gradient echo and spin echo echoplanar imaging sequences. Invest Radiol. 2016; 51:575–581.24. Rump J, Klatt D, Braun J, Warmuth C, Sack I. Fractional encoding of harmonic motions in MR elastography. Magn Reson Med. 2007; 57:388–395.
Article25. Venkatesh SK, Yin M, Ehman RL. Magnetic resonance elastography of liver: technique, analysis, and clinical applications. J Magn Reson Imaging. 2013; 37:544–555.
Article26. Yin M, Glaser KJ, Talwalkar JA, Chen J, Manduca A, Ehman RL. Hepatic MR elastography: clinical performance in a series of 1377 consecutive examinations. Radiology. 2016; 278:114–124.
Article27. Serai SD, Trout AT. Can MR elastography be used to measure liver stiffness in patients with iron overload? Abdom Radiol (NY). 2019; 44:104–109.
Article28. Kim YS, Song JS, Kannengiesser S, Seo SY. Comparison of spin-echo echoplanar imaging and gradient recalled echo-based MR elastography at 3 Tesla with and without gadoxetic acid administration. Eur Radiol. 2017; 27:4120–4128.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis of Meniscal Tear of the Knee Using Proton-weighted Fast Spin-Echo MR Imaging: Can be an Alternative to Conventional Spin-Echo Imaging?
- Meniscal Tears of the Knee: Diagnosis with Fast Spin-Echo MR Imaging and Role of Gadolinium-Enhancement
- Ultrafast Magnetic Resonance Imaging: Echo Planar Imaging and Spiral Scan Imaging
- Slow flow and mural thrombus in aortic diseases: Spin-echo MR findings and their differentiation
- Multi-slice Multi-echo Pulsed-gradient Spin-echo (MePGSE) Sequence for Diffusion Tensor Imaging MRI: A Preliminary Result