J Korean Soc Spine Surg.
2019 Sep;26(3):111-115. 10.4184/jkss.2019.26.3.111.
Paraspinal Ancient Schwannoma of the Dorsal Ramus Nerve: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Soonchunhyang University Gumi Hospital, Gumi, Korea. kuroo25@schmc.ac.kr
- 2Department of Pathology, College of Medicine, Soonchunhyang University Gumi Hospital, Gumi, Korea.
- KMID: 2459761
- DOI: http://doi.org/10.4184/jkss.2019.26.3.111
Abstract
- STUDY DESIGN: Case report.
OBJECTIVES
We report a case of paraspinal ancient schwannoma located at the upper thoracic level that mimicked an atypical lipoma or complicated epidermoid cyst. SUMMARY OF LITERATURE REVIEW: Few case reports of paraspinal schwannoma have been reported and the incidence of ancient schwannoma in the paraspinal muscle layer is very rare.
MATERIALS AND METHODS
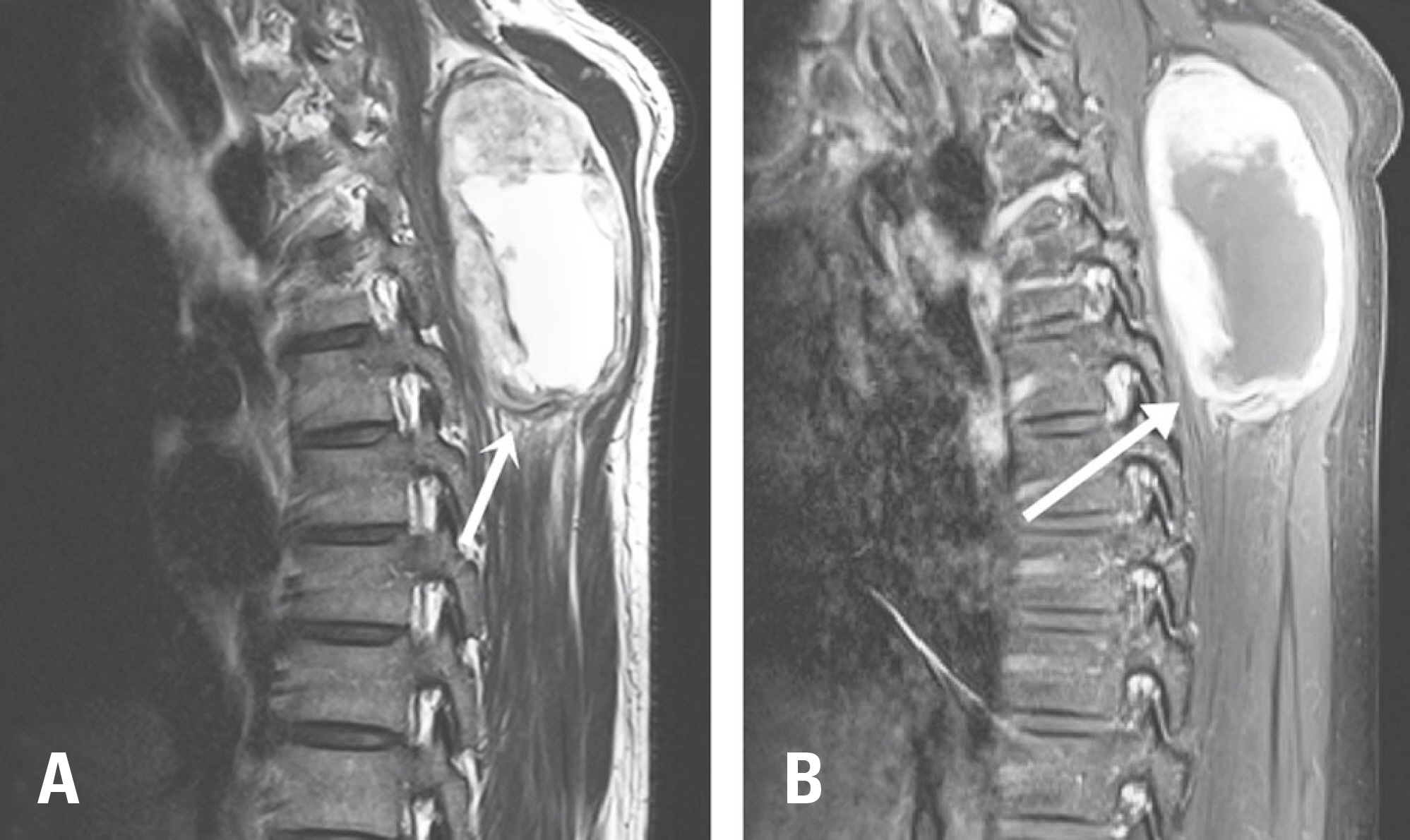
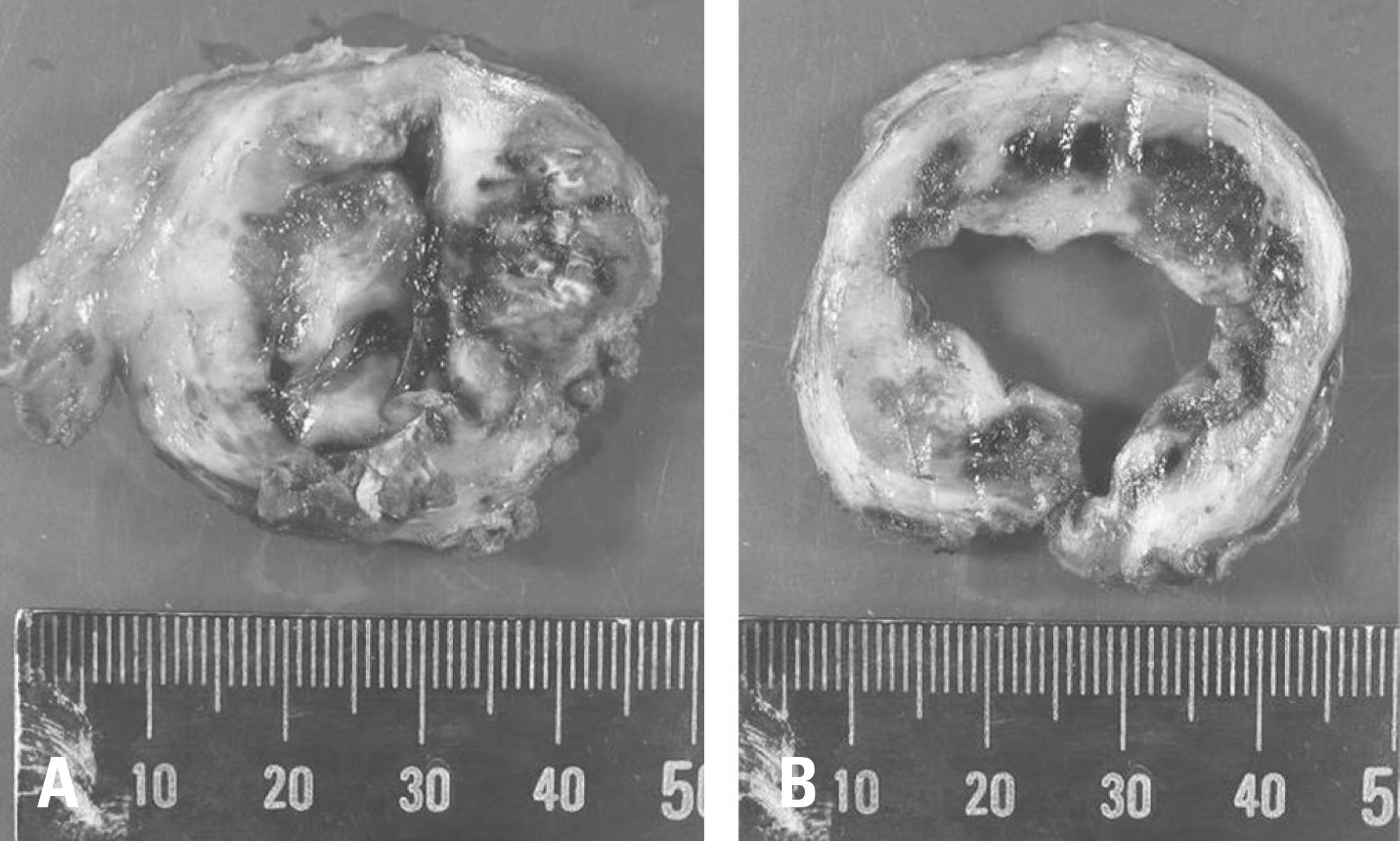
A 39-year-old man complained of a growing palpable back mass for 5 years. He experienced aggravated chronic discomfort around the mass while lying down. Both T1- and T2- weighted magnetic resonance imaging (MRI) showed a well-capsuled and heterogeneous high-signal mass in the muscle layer at the level from the T1 to T4 vertebral bodies on the right side of the midline. The tumor was completely removed by en bloc resection.
RESULTS
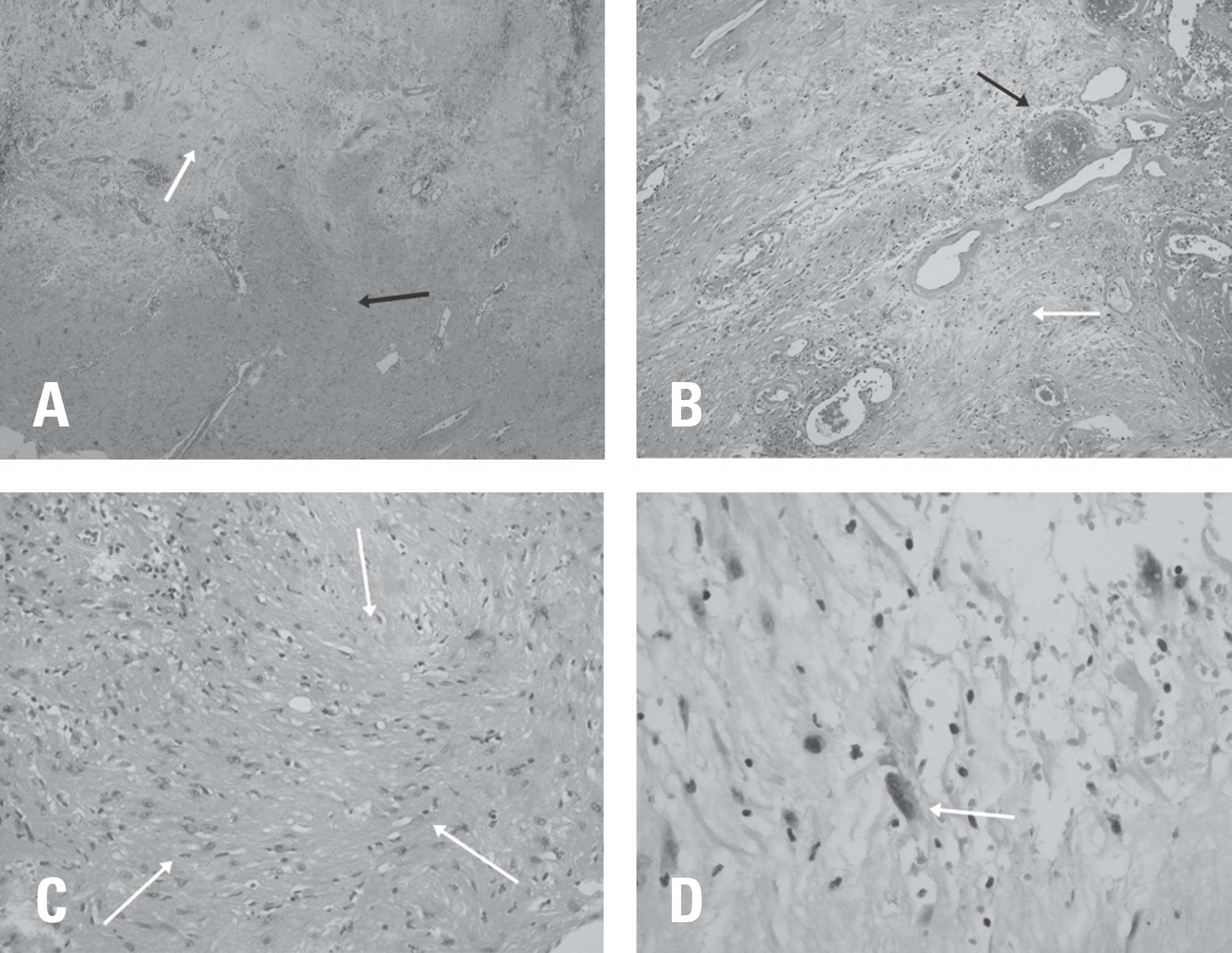
The pathologic examination revealed S-100 protein expression with degenerative changes. The lesion was diagnosed as an ancient schwannoma.
CONCLUSIONS
Schwannoma is one among the multiple possible causes of benign back masses. If a mass reveals a well-encapsulated heterogeneous mass on contrast MRI, a schwannoma should be suspected.
Keyword
MeSH Terms
Figure
Reference
-
1. Putney FJ, Moran JJ, Thomas GK. Neurogenic Tumors of the Head and Neck. Laryngoscope. 1964 Aug; 74:1037–59. DOI: 10.1288/00005537-196408000-00002.
Article2. Kim JH, Cho TG, Kim CH, et al. Erector Spinal Muscular Schwannoma of the Dorsal �amus Nerve: A Case �eport. Korean J Spine. 2015 Sep; 12(3):204–6. DOI: 10.14245/kjs.2015.12.3.204.3. Shah KA, Shah AC. Paraspinal Schwannoma of dorsal ramus nerve: A case report. J Clin Orthop Trauma. 2018 Jun; 9(2 Suppl):1–4. DOI: 10.1016/j.jcot.2018.04.012.
Article4. Dahl I. Ancient neurilemmoma (schwannoma). Acta Pathol Microbiol Scand A. 1977 Nov; 85:812–8. DOI: 10.1111/j.1699-0463.1977.tb03896.x.
Article5. Kransdorf MJ. Benign soft-tissue tumors in a large referral population: distribution of specific diagnoses by age, sex, and location. AJ� Am J �oentgenol. 1995 Feb; 164:395–402. DOI: 10.2214/ajr.164.2.7839977.
Article6. Joshi �. Learning from eponyms: Jose Verocay and Verocay bodies, Antoni A and B areas, Nils Antoni and Schwanno-mas. Indian Dermatol Online J. 2012 Sep-Dec; 3:215–9. DOI: 10.4103/2229-5178.101826.7. Antonopoulos C, Lilimpakis C, Karagianni M, et al. Ancient schwannoma of lumbar spine and review of the literature on paraspinal tumors, the role of preoperative biopsy: a case report. Cases J. 2009 Dec; 2:9325. DOI: 10.1186/1757-1626-2-9325.
Article8. Gaskin CM, Helms CA. Lipomas, lipoma variants. and well-differentiated liposarcomas (atypical lipomas): results of M�I evaluations of 126 consecutive fatty masses. 2004 Mar; 182(3):733–9. DOI: 10.2214/ajr.182.3.1820733.9. Hong SH, Chung HW, Choi JY, et al. M�I findings of subcutaneous epidermal cysts: emphasis on the pres-ence of rupture. 2006 Apr; 186(4):961–6. DOI: 10.2214/AJ�.05.0044.10. Ackerman LV, Taylor FH. Neurogenous tumors within the thorax; a clinicopathological evaluation of forty-eight cases. Cancer. 1951 July; 4:669–91. DOI: 10.1002/1097-0142 (195107)4: 4< 669:: aid-cncr2820040405> 3.0.co; 2-b.
Article