J Korean Soc Spine Surg.
2019 Sep;26(3):76-83. 10.4184/jkss.2019.26.3.76.
The Effects of Sagittal Spino-Pelvic Alignment on the Clinical Symptoms of Thoracolumbar Kyphosis in Osteoporotic Patients
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Eulji University, Daejeon, Korea. jaystar4u@naver.com
- KMID: 2459756
- DOI: http://doi.org/10.4184/jkss.2019.26.3.76
Abstract
- STUDY DESIGN: Retrospective study.
OBJECTIVES
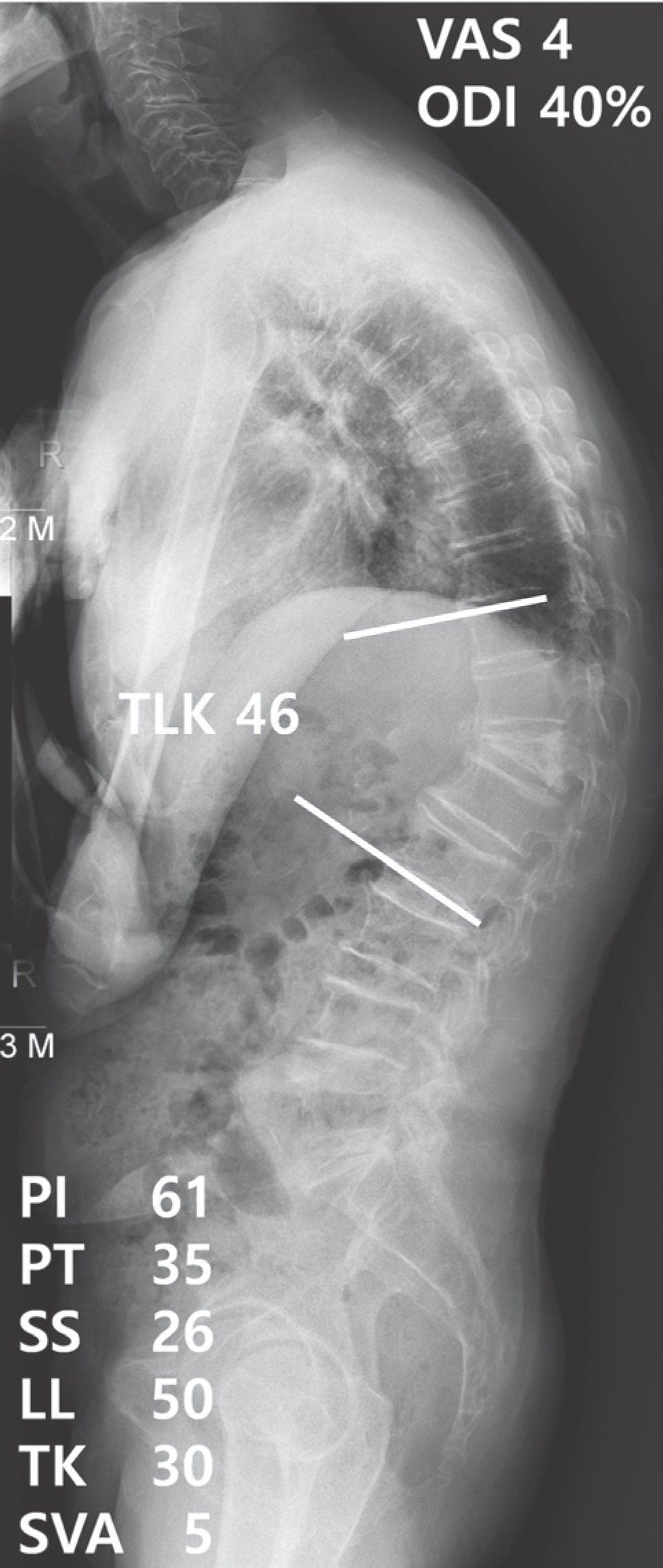
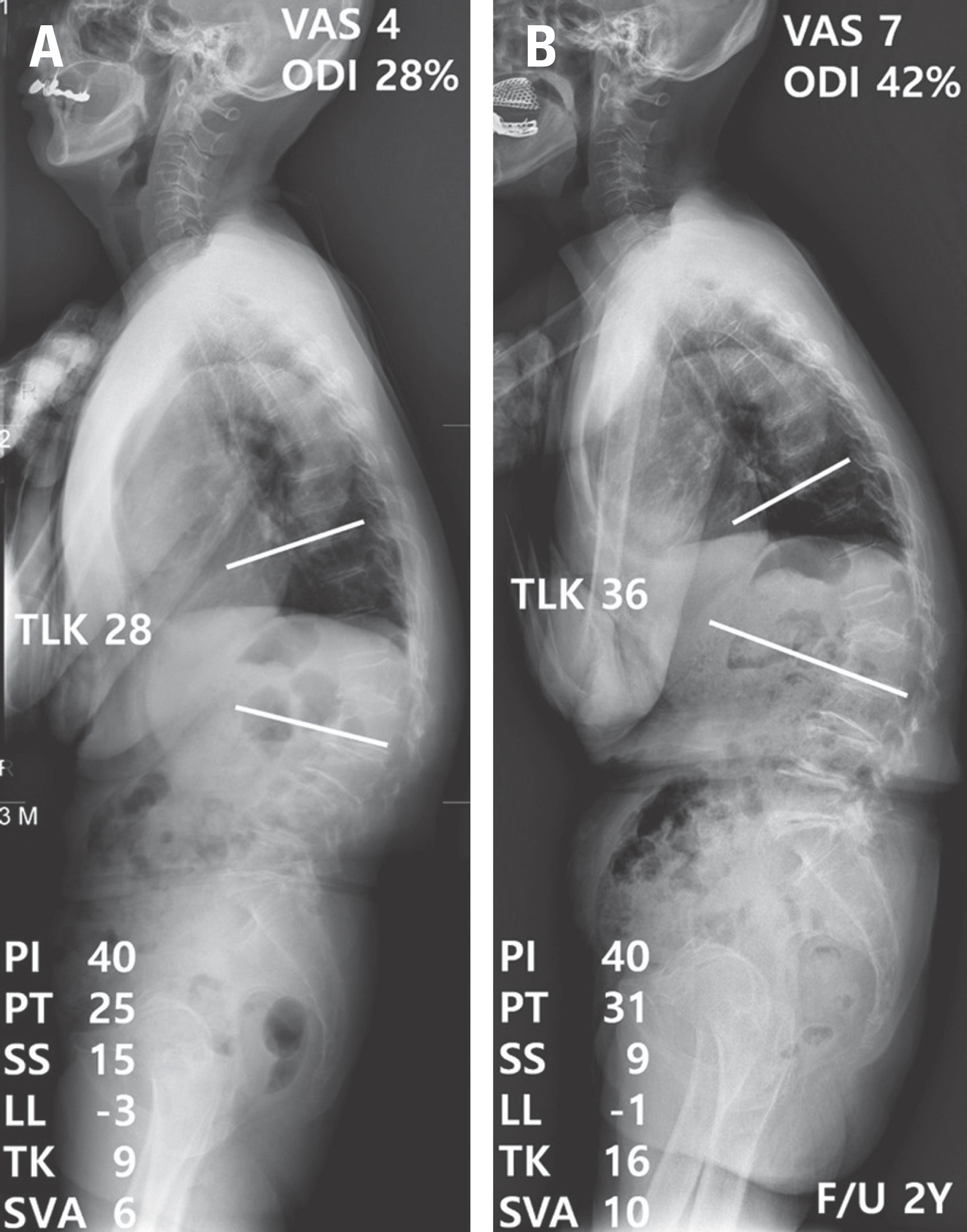
The purpose of this study was to assess the effect of sagittal spino-pelvic alignment on the clinical symptoms of thoracolumbar kyphosis (TLK; T10-L2 Cobb's angle >20°) in osteoporotic patients. SUMMARY OF LITERATURE REVIEW: Few studies have investigated the clinical symptoms and radiological features of TLK caused by degenerative changes. There is also controversy over whether clinical symptoms will deteriorate in patients with TLK or which treatment should be chosen according to the degree of TLK.
MATERIALS AND METHODS
From May 2005 to May 2016, we reviewed 75 patients who were diagnosed with TLK (T10-L2 Cobb's angle >20°) and osteoporosis. Patients were excluded from the study if they had neurological symptoms, underlying spinal disorders, or unstable vertebral fractures. Fifty patients with TLK due to an osteoporotic vertebral compression fracture (group F) and 25 patients with senile TLK (group S) were assessed by clinical symptoms and radiological parameters. Thoracolumbar kyphosis angle and sagittal vertical axis (SVA) were also analyzed. Clinical symptoms were assessed using a visual analogue scale (VAS) and the Oswestry Disability Index (ODI).
RESULTS
There were no significant differences in clinical symptoms (VAS, ODI) and radiological parameters between groups F and S, or according to the degree of TLK(20°-30°, 30°-40°, >40°). Clinical symptoms were significantly more severe in patients with sagittal imbalance (SVA >5 cm) than in those with sagittal balance.
CONCLUSIONS
Sagittal imbalance is a more important factor affecting clinical symptoms than the cause or the degree of TLK. Therefore, sagittal imbalance should be considered in the management of TLK in osteoporotic patients.
Figure
Reference
-
1. Khan BI, Yost MT, Badkoobehi H, et al. Prevalence of scoliosis and thoracolumbar kyphosis in patients with achon-droplasia. Spine Deform. 2016 Mar; 4(2):145–8. DOI: 10.1016/j.jspd.2015.08.003.
Article2. Li S, Li Z, Hua W, Wang K, Li S, et al. Clinical outcome and surgical strategies for late post-traumatic kyphosis after failed thoracolumbar fracture operation: case report and literature review. Medicine (Baltimore). 2017 Dec; 96(49):e8770. DOI: 10.1097/MD.0000000000008770.3. Tsirikos A, McMaster M. Infantile developmental thoracolumbar kyphosis with segmental subluxation of the spine. J Bone Joint Surg Br. 2010 Mar; 92(3):430–5. DOI: 10.1302/0301-620X.92B3.23075.
Article4. Rajasekaran S. Kyphotic deformity in spinal tuberculosis and its management. International orthopaedics. Int Orthop. 2012 Feb; 36(2):359–65. DOI: 10.1007/s00264-011-1469-2.5. Lee C-S, Lee C-K, Kim Y-T, et al. Dynamic sagittal imbalance of the spine in degenerative flat back: significance of pelvic tilt in surgical treatment. Spine (Phila Pa 1976). 2001 Sep 15; 26(18):2029–35. DOI: 10.1097/00007632-200109150-0017.6. Lee CS, Chung SS, Chung KH, et al. Significance of pelvic incidence in the development of abnormal sagittal alignment. Journal of the Korean Orthopaedic Association. 2006; 41(2):274–80. DOI: 10.4055/jkoa.2006.41.2.274.
Article7. Zeng Y, Qu X, Chen Z, et al. Posterior corrective surgery for moderate to severe focal kyphosis in the thoracolumbar spine: 57 cases with minimum 3 years follow-up. Eur Spine J. 2017 Jul; 26(7):1833–41. DOI: 10.1007/s00586-016-4875-8. Epub 2016 Dec 28.8. Cecchinato R, Berjano P, Damilano M, et al. Spinal oste-otomies to treat post-traumatic thoracolumbar deformity. Eur J Orthop Surg Traumatol. 2014 Jul; 24(Suppl 1):S31–7. DOI: 10.1007/s00590-014-1464-6.
Article9. Munting E. Surgical treatment of post-traumatic kyphosis in the thoracolumbar spine: indications and technical aspects. Eur Spine J. 2010 Mar; 19(Suppl 1):S69–73. DOI: 10.1007/s00586-009-1117-3.
Article10. Finocchiaro FM, Nena U, Scalzo VL, et al. Treatment of kyphotic deformities in adults: our experience. Eur Spine J. 2012 May; 21(Suppl 1):S100–7. DOI: 10.1007/s00586-012-2224-0.
Article11. Kim BG, Dan JM, Shin DE. Treatment of thoracolumbar fracture. Asian Spine J. 2015 Feb; 9(1):133–46. DOI: 10.4184/asj.2015.9.1.133.
Article12. Chang KW, Chen YY, Lin CC, et al. Apical lordosating osteotomy and minimal segment fixation for the treatment of thoracic or thoracolumbar osteoporotic kyphosis. Spine (Phila Pa 1976). 2005 Jul 15; 30(14):1674–81. DOI: 10.1097/01.brs.0000170450.77554.bc.
Article13. Dang NR, Moreau MJ, Hill DL, et al. Intra-observer reproducibility and interobserver reliability of the radiographic parameters in the Spinal Deformity Study Group's AIS Radiographic Measurement Manual. Spine (Phila Pa 1976). 2005 May 1; 30(9):1064–9. DOI: 10.1097/01. brs.0000160840.51621.6b.
Article14. Kim MS, Chung SW, Hwang C, et al. A radiographic analysis of sagittal spinal alignment for the standardization of standing lateral position. Journal of the Korean Orthopaedic Association. 2005; 40(7):861–7. DOI: 10.4055/jkoa.2005.40.7.861.
Article15. Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volun-teers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine (Phila Pa 1976). 1994 Jul 15; 19(14):1611–8. DOI: 10.1097/00007632-199407001-00010.16. Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005 Sep 15; 30(18):2024–9. DOI: 10.1097/01. brs.0000179086.30449.96.
Article17. Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society—Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976). 2012 May 20; 37(12):1077–82. DOI: 10.1097/BRS.0b013e31823e15e2.18. Bedbrook GM. Treatment of thoracolumbar dislo-cation and fractures with paraplegia. Clin Orthop Relat Res. 2012 May 20; 37(12):1077–82. DOI: 10.1097/BRS.0b013e31823e15e2.19. Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976). 1992 May; 17(5):528–40. DOI: 10.1097/00007632-199205000-00010.20. DeWald RL. Burst fractures of the thoracic and lumbar spine. Clin Orthop Relat Res. 1984 Oct; 189:150–61.
Article21. Wei Y, Tian W, Zhang G, et al. Thoracolumbar kyphosis is associated with compressive vertebral fracture in postmeno-pausal women. Osteoporos Int. 2017 Jun; 28(6):1925–1929. DOI: 10.1007/s00198-017-3971-x.
Article22. Kim YB, Kim YJ, Ahn YJ, et al. A comparative analysis of sagittal spinopelvic alignment between young and old men without localized disc degeneration. Eur Spine J. 2014 Jul; 23(7):1400–6. DOI: 10.1007/s00586-014-3236-8.
Article23. Kang KB, Kim YJ, Muzaffar N, et al. Changes of sagittal spinopelvic parameters in normal Koreans with age over 50. Asian Spine J. 2010 Dec; 4(2):96–101. DOI: 10.4184/asj.2010.4.2.96.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Normal Age-Adjusted Sagittal Spinal Alignment Is Achieved with Surgical Correction in Adolescent Idiopathic Scoliosis
- What Is the Effect of Spino-Pelvic Sagittal Parameters and Back Muscles on Osteoporotic Vertebral Fracture?
- Surgical Impact on Global Sagittal Alignment and Health-Related Quality of Life Following Cervical Kyphosis Correction Surgery: Systematic Review
- L1 Slope as an Indicator of Thoracolumbar Sagittal Balance in Osteoporotic Vertebral Fractures
- Significance of Pelvic Incidence in the Development of Abnormal Sagittal Alignment