Korean J Radiol.
2019 Nov;20(11):1546-1553. 10.3348/kjr.2019.0030.
Symptomatic Retinal Artery Occlusion after Angioplasty and Stenting of the Carotid Artery: Incidence and Related Risk Factors
- Affiliations
-
- 1Department of Neurology, International St. Mary's Hospital, Catholic Kwandong University College of Medicine, Incheon, Korea.
- 2Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. aronnn@naver.com
- 3Department of Neurosurgery, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea.
- 4Department of Neurosurgery, Kwangju Christian Hospital, Gwangju, Korea.
- 5Department of Neurosurgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 6Institute of Biomedical Science, Catholic Kwandong University International St. Mary's Hospital, Incheon, Korea.
- 7Department of Neurosurgery, Veterans Health Service Medical Center, Seoul, Korea.
- KMID: 2459422
- DOI: http://doi.org/10.3348/kjr.2019.0030
Abstract
OBJECTIVE
Retinal artery occlusion (RAO) is rarely seen as a complication in patients undergoing carotid artery stenting (CAS); hence, its characteristics have not been documented in detail. This study aimed to investigate the incidence of this complication and the related risk factors, focusing on differences in ophthalmic artery (OA) supply (whether by the external or internal carotid artery [ECA or ICA]) prior to CAS procedures.
MATERIALS AND METHODS
We retrospectively examined 342 patients who underwent CAS for severe and/or symptomatic carotid artery stenosis between January 2009 and December 2017. Cumulative medical records and radiologic data were assessed. RAO was confirmed by photography and fluorescent angiography of the fundus, which were performed by an ophthalmologist. In all patients, distal filter systems of various types were applied as cerebral protection devices (CPDs) during procedures. Univariate and multivariate analyses were conducted to identify the risk factors for RAO after CAS.
RESULTS
Symptomatic RAO was observed in six patients (1.8%), of which five (6.8%) were ECA-dominant group members (n = 74). In a binary logistic regression analysis, OA supply by the ECA (odds ratio [OR], 9.705; 95% confidence interval [CI], 1.519-62.017; p = 0.016) and older age (OR, 1.159; 95% CI, 1.005-1.336; p = 0.041) were identified as significant risk factors in patients with RAO after CAS. ECA-supplied OA was also associated with the severity of ipsilateral ICA stenosis (p = 0.001) and ulcerative plaque (p = 0.021).
CONCLUSION
In procedures performed using ICA distal filtering CPD systems, RAO as a complication of CAS (performed for severe stenosis) showed a relationship to ECA-supplied OA. For older patients, simultaneous use of ICA-ECA CPDs might help prevent such complications.
Keyword
MeSH Terms
-
Angiography
Angioplasty*
Carotid Arteries*
Carotid Artery, Internal
Carotid Stenosis
Constriction, Pathologic
Humans
Incidence*
Logistic Models
Medical Records
Multivariate Analysis
Ophthalmic Artery
Photography
Retinal Artery Occlusion*
Retinal Artery*
Retinaldehyde*
Retrospective Studies
Risk Factors*
Stents*
Ulcer
Retinaldehyde
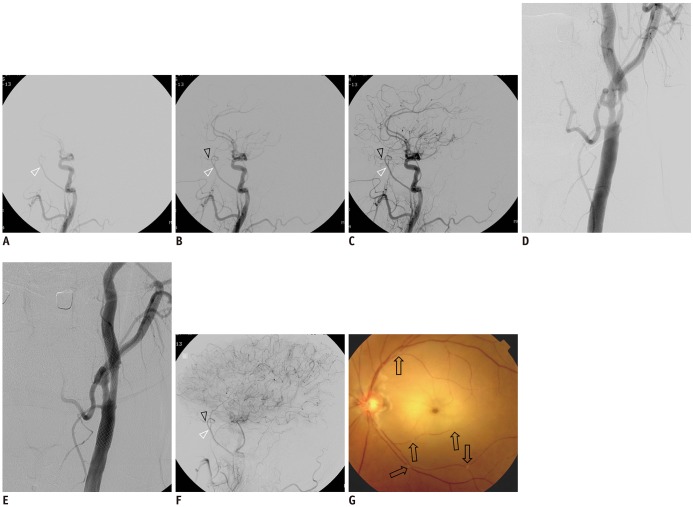
Figure
Reference
-
1. Vos JA, van Werkum MH, Bistervels JH, Ackerstaff RG, Tromp SC, van den Berg JC. Retinal embolization during carotid angioplasty and stenting: periprocedural data and follow-up. Cardiovasc Intervent Radiol. 2010; 33:714–719. PMID: 20033690.
Article2. Song G, Sun R, Chen YF, Ma Y, Wang YB, Jiao LQ, et al. Retinal embolization after carotid endarterectomy and stenting for carotid artery stenosis. J Clin Neurosci. 2015; 22:1298–1302. PMID: 25986182.
Article3. Cohn EJ Jr, Sandager GP, Benjamin ME, Lilly MP, Hanna DJ, Flinn WR. Assessment of ocular perfusion after carotid endarterectomy with color-flow duplex scanning. J Vasc Surg. 1999; 29:665–671. PMID: 10194494.
Article4. Costa VP, Kuzniec S, Molnar LJ, Cerri GG, Puech-Leão P, Carvalho CA. The effects of carotid endarterectomy on the retrobulbar circulation of patients with severe occlusive carotid artery disease. An investigation by color Doppler imaging. Ophthalmology. 1999; 106:306–310. PMID: 9951482.5. Rosenkranz K, Langer R, Felix R. Transcranial Doppler sonography: collateral pathways in internal carotid artery obstructions. Angiology. 1991; 42:819–826. PMID: 1952270.
Article6. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Endarterectomy for asymptomatic carotid artery stenosis. JAMA. 1995; 273:1421–1428. PMID: 7723155.7. European Carotid Surgery Trialists' Collaborative Group. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998; 351:1379–1387. PMID: 9593407.8. Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998; 339:1415–1425. PMID: 9811916.9. Halliday A, Mansfield A, Marro J, Peto C, Peto R, Potter J, et al. MRC Asymptomatic Carotid Surgery Trial (ACST) Collaborative Group. Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomised controlled trial. Lancet. 2004; 363:1491–1502. PMID: 15135594.10. Narins CR, Illig KA. Patient selection for carotid stenting versus endarterectomy: a systematic review. J Vasc Surg. 2006; 44:661–672. PMID: 16950453.
Article11. Bonati LH, Jongen LM, Haller S, Flach HZ, Dobson J, Nederkoorn PJ, et al. ICSS-MRI study group. New ischaemic brain lesions on MRI after stenting or endarterectomy for symptomatic carotid stenosis: a substudy of the International Carotid Stenting Study (ICSS). Lancet Neurol. 2010; 9:353–362. PMID: 20189458.
Article12. Wilentz JR, Chati Z, Krafft V, Amor M. Retinal embolization during carotid angioplasty and stenting: mechanisms and role of cerebral protection systems. Catheter Cardiovasc Interv. 2002; 56:320–327. PMID: 12112883.
Article13. Henderson RD, Eliasziw M, Fox AJ, Rothwell PM, Barnett HJ. Angiographically defined collateral circulation and risk of stroke in patients with severe carotid artery stenosis. North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group. Stroke. 2000; 31:128–132. PMID: 10625727.14. Ansel GM, Hopkins LN, Jaff MR, Rubino P, Bacharach JM, Scheinert D, et al. Investigators for the ARMOUR Pivotal Trial. Safety and effectiveness of the INVATEC MO.MA proximal cerebral protection device during carotid artery stenting: results from the ARMOUR pivotal trial. Catheter Cardiovasc Interv. 2010; 76:1–8. PMID: 20222019.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Retinal Artery Occlusion after Carotid Angioplasty and Stenting: A Case Report
- A Case of Transseptal Approach to Carotid Artery Stenting in Right Internal Carotid Stenosis
- Central Retinal Artery Occlusion After Carotid Artery Angioplasty and Stenting in an Elderly Patient: A Case Report
- Ophthalmic Artery Occlusion After Carotid Revascularization
- Percutaneous Transluminal Angioplasty with Palmaz-Schatz Stent in the Carotid Artery Stenosis