Ann Surg Treat Res.
2019 Oct;97(4):202-209. 10.4174/astr.2019.97.4.202.
Effect of severe contralateral carotid stenosis or occlusion on early and late outcomes after carotid endarterectomy
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. ypcho@amc.seoul.kr
- 2Department of Clinical Epidemiology and Biostatistics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2459318
- DOI: http://doi.org/10.4174/astr.2019.97.4.202
Abstract
- PURPOSE
We aimed to compare clinical outcomes after carotid endarterectomy (CEA) between Korean patients with and without severe contralateral extracranial carotid stenosis or occlusion (SCSO).
METHODS
Between January 2004 and December 2014, a total of 661 patients who underwent 731 CEAs were stratified by SCSO (non-SCSO and SCSO groups) and analyzed retrospectively. The study outcomes included the occurrence of major adverse cardiovascular events (MACE), defined as stroke or myocardial infarction, and all-cause mortality during the perioperative period and within 4 years after CEA.
RESULTS
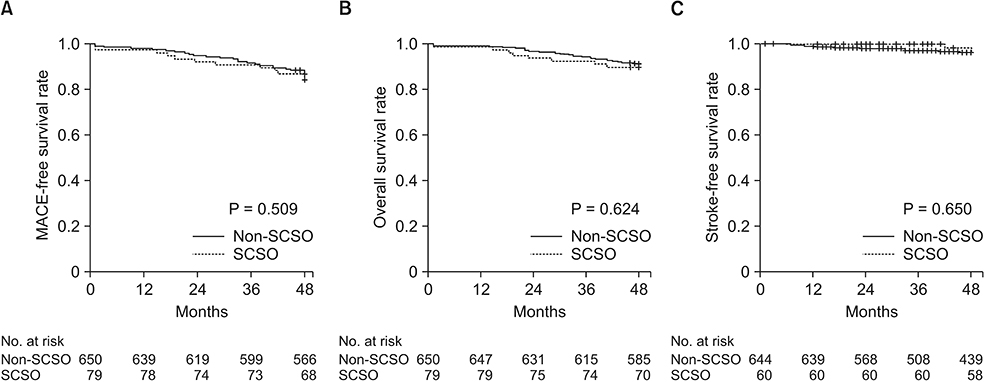
There were no significant differences in the incidence of MACE or any individual MACE manifestations between the 2 groups during the perioperative period or within 4 years after CEA. On multivariate analysis to identify clinical variables associated with long-term study outcomes, older age (hazard ratios [HRs], 1.06; 95% confidence intervals [CIs], 1.03-1.09; P < 0.001) and diabetes mellitus (HR, 1.71; 95% CI, 1.14-2.57; P = 0.010) were significantly associated with an increased risk of MACE occurrence, while preexisting SCSO was not associated with long-term incidence of MACE and individual MACE components. Kaplan-Meier survival analysis showed similar MACE-free (P = 0.509), overall (P = 0.642), and stroke-free (P = 0.650) survival rates in the 2 groups.
CONCLUSION
There were no significant differences in MACE incidence after CEA between the non-SCSO and SCSO groups, and preexisting SCSO was not associated with an increased risk of perioperative or long-term MACE occurrence.
Keyword
MeSH Terms
Figure
Reference
-
1. Ueshima H, Sekikawa A, Miura K, Turin TC, Takashima N, Kita Y, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008; 118:2702–2709.2. Jee SH, Suh I, Kim IS, Appel LJ. Smoking and atherosclerotic cardiovascular disease in men with low levels of serum cholesterol: the Korea Medical Insurance Corporation Study. JAMA. 1999; 282:2149–2155.3. Brott TG, Hobson RW 2nd, Howard G, Roubin GS, Clark WM, Brooks W, et al. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010; 363:11–23.
Article4. Silver FL, Mackey A, Clark WM, Brooks W, Timaran CH, Chiu D, et al. Safety of stenting and endarterectomy by symptomatic status in the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST). Stroke. 2011; 42:675–680.
Article5. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Barnett HJM, Taylor DW, Haynes RB, Sackett DL, Peerless SJ, et al. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991; 325:445–453.
Article6. European Carotid Surgery Trialists' Collaborative Group. MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70-99%) or with mild (0-29%) carotid stenosis. Lancet. 1991; 337:1235–1243.7. Skerritt MR, Block RC, Pearson TA, Young KC. Carotid endarterectomy and carotid artery stenting utilization trends over time. BMC Neurol. 2012; 12:17.
Article8. Lee J, You JH, Oh SH, Shin S, Kim BM, Kim TS, et al. Outcomes of stenting versus endarterectomy for symptomatic extracranial carotid stenosis: a retrospective multicenter study in Korea. Ann Vasc Surg. 2019; 54:185–192.e1.
Article9. Gasecki AP, Eliasziw M, Ferguson GG, Hachinski V, Barnett HJ. Long-term prognosis and effect of endarterectomy in patients with symptomatic severe carotid stenosis and contralateral carotid stenosis or occlusion: results from NASCET. North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group. J Neurosurg. 1995; 83:778–782.10. Kretz B, Abello N, Astruc K, Terriat B, Favier C, Bouchot O, et al. Influence of the contralateral carotid artery on carotid surgery outcome. Ann Vasc Surg. 2012; 26:766–774.
Article11. Kwon H, Kim HK, Kwon SU, Lee SW, Kim MJ, Park JW, et al. Risk of major adverse cardiovascular events in subjects with asymptomatic mild carotid artery stenosis. Sci Rep. 2018; 8:4700.
Article12. Kim A, Kwon TW, Han Y, Kwon SU, Kwon H, Noh M, et al. Clinical outcomes of staged bilateral carotid endarterectomy for bilateral carotid artery stenosis. Ann Surg Treat Res. 2015; 89:261–267.
Article13. Kim JH, Cho YP, Kwon TW, Kim H, Kim GE. Ten-year comparative analysis of bovine pericardium and autogenous vein for patch angioplasty in patients undergoing carotid endarterectomy. Ann Vasc Surg. 2012; 26:353–358.
Article14. Marrocco-Trischitta MM, Melissano G, Kahlberg A, Setacci F, Abeni D, Chiesa R. Increased incidence of cerebral clamping ischemia during early contralateral carotid endarterectomy. J Vasc Surg. 2006; 43:1155–1161.
Article15. Brott T, Adams HP Jr, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989; 20:864–870.
Article16. Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T. Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ. 1980; 58:113–130.17. Kwon H, Moon DH, Han Y, Lee JY, Kwon SU, Kang DW, et al. Impact of subclinical coronary artery disease on the clinical outcomes of carotid endarterectomy. J Neurosurg. 2017; 126:1560–1565.
Article18. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007; 45 Suppl S:S5–S67.
Article19. AbuRahma AF, Stone P, Deem S, Dean LS, Keiffer T, Deem E. Proposed duplex velocity criteria for carotid restenosis following carotid endarterectomy with patch closure. J Vasc Surg. 2009; 50:286–291.
Article20. Berman DS, Abidov A, Kang X, Hayes SW, Friedman JD, Sciammarella MG, et al. Prognostic validation of a 17-segment score derived from a 20-segment score for myocardial perfusion SPECT interpretation. J Nucl Cardiol. 2004; 11:414–423.21. Kim YH, Ahn JM, Park DW, Song HG, Lee JY, Kim WJ, et al. Impact of ischemia-guided revascularization with myocardial perfusion imaging for patients with multivessel coronary disease. J Am Coll Cardiol. 2012; 60:181–190.
Article22. Patel PB, LaMuraglia GM, Lancaster RT, Clouse WD, Kwolek CJ, Conrad MF, et al. Severe contralateral carotid stenosis or occlusion does not have an impact on risk of ipsilateral stroke after carotid endarterectomy. J Vasc Surg. 2018; 67:1744–1751.
Article23. Cunningham EJ, Bond R, Mehta Z, Mayberg MR, Warlow CP, Rothwell PM, et al. Long-term durability of carotid endarterectomy for symptomatic stenosis and risk factors for late postoperative stroke. Stroke. 2002; 33:2658–2663.
Article24. Cheng W, Lu H, Hu Y. Influence of contralateral carotid occlusion on outcomes after carotid endarterectomy: a meta-analysis. J Stroke Cerebrovasc Dis. 2018; 27:2587–2595.
Article25. Kang J, Conrad MF, Patel VI, Mukhopadhyay S, Garg A, Cambria MR, et al. Clinical and anatomic outcomes after carotid endarterectomy. J Vasc Surg. 2014; 59:944–949.
Article26. Chiriano J, Abou-Zamzam AM Jr, Nguyen K, Molkara AM, Zhang WW, Bianchi C, et al. Preoperative carotid duplex findings predict carotid stump pressures during endarterectomy in symptomatic but not asymptomatic patients. Ann Vasc Surg. 2010; 24:1038–1044.
Article27. AbuRahma AF, Mousa AY, Stone PA, Hass SM, Dean LS, Keiffer T. Correlation of intraoperative collateral perfusion pressure during carotid endarterectomy and status of the contralateral carotid artery and collateral cerebral blood flow. Ann Vasc Surg. 2011; 25:830–836.
Article28. GALA Trial Collaborative Group. Lewis SC, Warlow CP, Bodenham AR, Colam B, Rothwell PM, et al. General anaesthesia versus local anaesthesia for carotid surgery (GALA): a multicentre, randomised controlled trial. Lancet. 2008; 372:2132–2142.29. Mozes G, Sullivan TM, Torres-Russotto DR, Bower TC, Hoskin TL, Sampaio SM, et al. Carotid endarterectomy in SAPPHIRE-eligible high-risk patients: implications for selecting patients for carotid angioplasty and stenting. J Vasc Surg. 2004; 39:958–965.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Carotid Artery Occlusive Diseases Treated with Staged Subclavian-carotid Artery bypass and Carotid Endarterectomy: Case Report
- Improved Cerevral Blood Flow and Cerebrovascular Reserve after Carotid Endarterectomy in Patients with Carotid Stenosis and Contralateral Carotid Occlusion: Acetazolamide Stress Brain SPECT Study
- Current Indications of Surgery and Endovascular Treatment in Ischemic Stroke
- Recurrent Carotid Artery Stenosis
- Hemodynamic Depression of Early Carotid Revascularization on Ischemic Stroke Patients with Symptomatic Carotid Stenosis