Yonsei Med J.
2019 Oct;60(10):992-997. 10.3349/ymj.2019.60.10.992.
Characteristics of Lung Allocation and Outcomes of Lung Transplant according to the Korean Urgency Status
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Ajou University School of Medicine, Suwon, Korea.
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 4Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Thoracic and Cardiovascular Surgery, Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea.
- 6Department of Pulmonology and Critical Care Medicine, Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea.
- 7Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 8Department of Pulmonology and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 9Division of Pulmonary and Critical Care medicine, Department of Medicine, Samsung Medical Center, School of Medicine, Sungkyunkwan University, Seoul, Korea.
- 10Department of Thoracic and Cardiovascular Surgery, Yonsei University College of Medicine, Seoul, Korea. csjglee@yuhs.ac
- KMID: 2459153
- DOI: http://doi.org/10.3349/ymj.2019.60.10.992
Abstract
- PURPOSE
We investigated the characteristics of lung allocation and outcomes of lung transplant (LTx) according to the Korean urgency status.
MATERIALS AND METHODS
LTx registration in the Korean Organ Transplantation Registry (KOTRY) began in 2015. From 2015 to June 2017, 86 patients who received LTx were enrolled in KOTRY. After excluding one patient who received a heart-lung transplant, 85 were included. Subjects were analyzed according to the Korean urgency status.
RESULTS
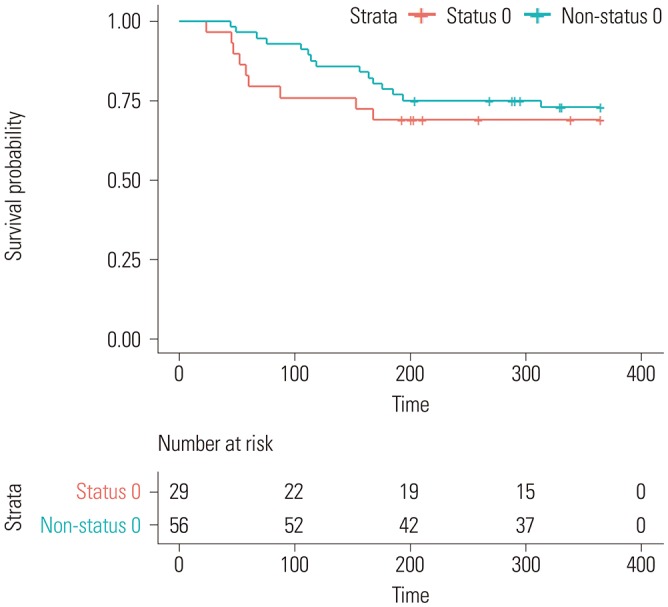
Except for Status 0, urgency status was classified based on partial pressure of oxygen in arterial blood gas analysis and functional status in 52 patients (93%). The wait time for lung allograft was well-stratified by urgency (Status 0, 46.5±59.2 days; Status 1, 104.4±98.2 days; Status 2 or 3, 132.2±118.4 days, p=0.009). Status 0 was associated with increased operative times and higher intraoperative blood transfusion. Status 0 was associated with prolonged extracorporeal membrane oxygenation use, postoperative bleeding, and longer mechanical ventilation after operation. Survival of Status 0 patients seemed worse than that of non-Status 0 patients, although differences were not significant.
CONCLUSION
The Korean urgency classification for LTx is determined by using very limited parameters and may not be a true reflection of urgency. Status 0 patients seem to have poor outcomes compared to the other urgency status patients, despite having the highest priority for donor lungs. Further multi-center and nationwide studies are needed to revise the lung allocation system to reflect true urgency and provide the best benefit of lung transplantation.
MeSH Terms
Figure
Reference
-
1. Kotloff RM, Thabut G. Lung transplantation. Am J Respir Crit Care Med. 2011; 184:159–171. PMID: 21471083.
Article2. Haam SJ, Lee DY, Paik HC. An overview of lung transplantation in Korea. Transplant Proc. 2008; 40:2620–2622. PMID: 18929819.
Article3. Hong SB, Kim HJ, Huh JW, Do KH, Jang SJ, Song JS, et al. A cluster of lung injury associated with home humidifier use: clinical, radiological and pathological description of a new syndrome. Thorax. 2014; 69:694–702. PMID: 24473332.
Article4. Korean Network for Organ Sharing (KONOS). Organ transplantation statistics in 2017 [Internet]. Seoul: KONOS;accessed on 2019 April 1. Available at: https://www.konos.go.kr/konosis/.5. Egan TM, Murray S, Bustami RT, Shearon TH, McCullough KP, Edwards LB, et al. Development of the new lung allocation system in the United States. Am J Transplant. 2006; 6(5 Pt 2):1212–1227. PMID: 16613597.
Article7. Yu WS, Suh JW, Song SH, Paik HC, Kim SY, Park MS, et al. The lung allocation score could evaluate allocation systems in countries that do not use the score. PLoS One. 2019; 14:e0214853. PMID: 30943262.
Article8. Lee JG, Kim SY, Kim YT, Lee HJ, Park S, Choi SM, et al. First report of the Korean lung transplantation registry. Transplant Proc. 2018; 50:2759–2763. PMID: 30401392.
Article9. Jeong YH, Choi S, Park SI, Kim DK. Asan Medical Center Lung Transplantation Team. Clinical outcomes of lung transplantation: experience at Asan Medical Center. Korean J Thorac Cardiovasc Surg. 2018; 51:22–28. PMID: 29430425.
Article10. Health Resources and Services Administration, U.S. Department of Health and Human Services. LAS Calculator [Internet]. Richmond: Health Resources and Services Administration, U.S. Department of Health and Human Services;accessed on 2017 July 1. Available at: https://optn.transplant.hrsa.gov/resources/allocation-calculators/las-calculator/.11. Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995; 57:289–300.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The performance of lung transplantation according to the pattern of changing urgency: KONOS registry analysis
- Allocation of Donor Lungs in Korea
- Performance Changes Following the Revision of Organ Allocation System of Lung Transplant: Analysis of Korean Network for Organ Sharing Data
- Performance changes following the revision of organ allocation system of lung transplant: analysis of Korean Network for Organ Sharing (KONOS) data
- The assessment and outcomes of human leukocyte antigen mismatches of lung transplantation in Korean patients