J Breast Cancer.
2019 Sep;22(3):484-490. 10.4048/jbc.2019.22.e31.
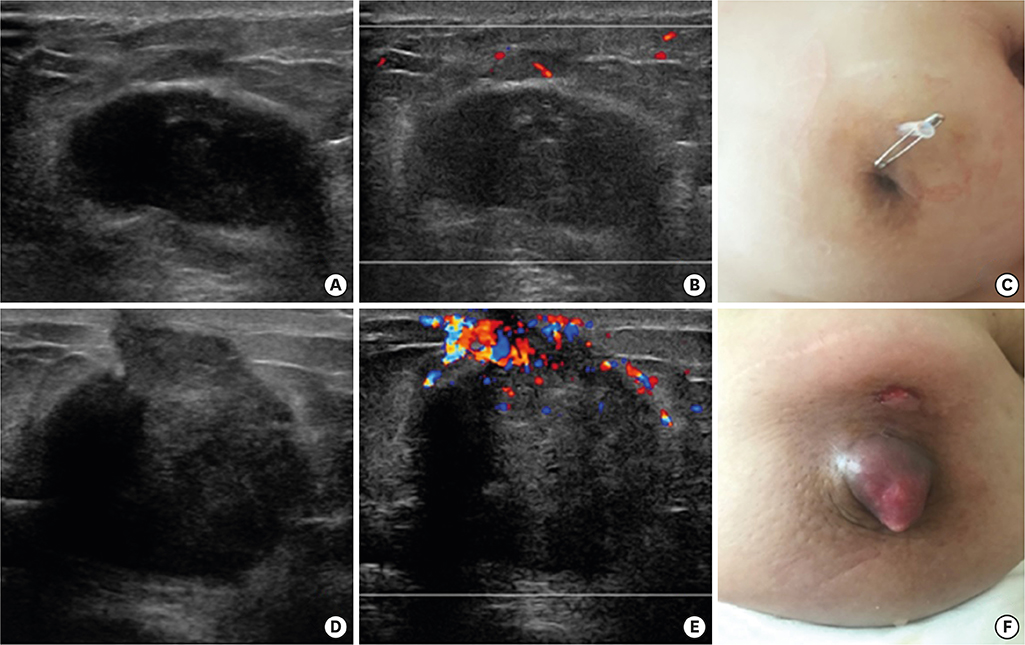
Human Epidermal Growth Factor Receptor 2-Subtype Invasive Ductal Carcinoma Recurring as Basal-Human Epidermal Growth Factor Receptor 2-Subtype Squamous Cell Carcinoma
- Affiliations
-
- 1Department of Surgery, Ewha Womans University School of Medicine, Seoul, Korea. mbit@ewha.ac.kr
- 2Department of Pathology, Ewha Womans University School of Medicine, Seoul, Korea.
- 3Department of Hematology-Oncology, Ewha Woman's University School of Medicine, Seoul, Korea.
- KMID: 2458868
- DOI: http://doi.org/10.4048/jbc.2019.22.e31
Abstract
- Squamous cell carcinoma of the breast and its subtype, basal-human epidermal growth factor receptor 2 (HER2) phenotype, are very rare. Herein, we report a patient who developed recurrence of squamous cell carcinoma of the breast with basal-HER2 subtype 6 years after the initial diagnosis of invasive ductal carcinoma of the HER2 subtype. To the best of our knowledge, recurrence of invasive ductal carcinoma in the form of metaplastic squamous cell carcinoma of basal-HER2 subtype has not been reported previously. We present a pathological perspective of our experience.
Keyword
MeSH Terms
Figure
Reference
-
1. Cardoso F, Leal C, Meira A, Azevedo R, Mauricio MJ, Leal da Silva JM, et al. Squamous cell carcinoma of the breast. Breast. 2000; 9:315–319.
Article2. Aparicio I, Martínez A, Hernández G, Hardisson D, De Santiago J. Squamous cell carcinoma of the breast. Eur J Obstet Gynecol Reprod Biol. 2008; 137:222–226.
Article3. Siegelmann-Danieli N, Murphy TJ, Meschter SC, Stein ME, Prichard J. Primary pure squamous cell carcinoma of the breast. Clin Breast Cancer. 2005; 6:270–272.
Article4. Zhang X, Zhang B, Zang F, Zhao L, Yuan Z, Wang P. Clinical features and treatment of squamous cell carcinoma of the breast. Onco Targets Ther. 2016; 9:3181–3185.
Article5. Weigelt B, Kreike B, Reis-Filho JS. Metaplastic breast carcinomas are basal-like breast cancers: a genomic profiling analysis. Breast Cancer Res Treat. 2009; 117:273–280.
Article6. Hennessy BT, Krishnamurthy S, Giordano S, Buchholz TA, Kau SW, Duan Z, et al. Squamous cell carcinoma of the breast. J Clin Oncol. 2005; 23:7827–7835.
Article7. Shui R, Li A, Yang F, Zhou X, Yu B, Xu X, et al. Primary squamous cell carcinoma of the breast with unusual basal-HER2 phenotype. Int J Clin Exp Pathol. 2014; 7:5203–5209.8. Singh H, Williams SP, Kinsella V, Lynch GR. Postradiation squamous cell cancer of the breast. Cancer Invest. 2000; 18:343–346.
Article9. Bagaria SP, Ray PS, Wang J, Kropcho L, Chung A, Sim MS, et al. Prognostic value of basal phenotype in HER2-overexpressing breast cancer. Ann Surg Oncol. 2012; 19:935–940.
Article10. Liu H, Fan Q, Zhang Z, Li X, Yu H, Meng F. Basal-HER2 phenotype shows poorer survival than basal-like phenotype in hormone receptor-negative invasive breast cancers. Hum Pathol. 2008; 39:167–174.
Article11. Sagara Y, Takada M, Ohi Y, Ohtani S, Kurozumi S, Inoue K, et al. Effectiveness of neo-adjuvant systemic therapy with trastuzumab for basal HER2 type breast cancer: results from retrospective cohort study of Japan Breast Cancer Research Group (JBCRG)-C03. Breast Cancer Res Treat. 2018; 171:675–683.
Article12. Filatenkov A, Baker J, Mueller AM, Kenkel J, Ahn GO, Dutt S, et al. Ablative tumor radiation can change the tumor immune cell microenvironment to induce durable complete remissions. Clin Cancer Res. 2015; 21:3727–3739.
Article13. Keener AB. Shapeshifters in cancer: how some tumor cells change phenotype to evade therapy. Nat Med. 2016; 22:1194–1196.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic significance of epidermal growth factor receptor expression in human gastric carcinoma
- Expression of Epidermal Growth Factor Receptor in Malignant Epidermal Tumors
- Clinical significance of the expression oncosuppressor gene proteins and epidermal growth factor receptor in squamous cell carcinomas of the larynx
- Amplification of epidermal growth factor receptor gene in primary cervical cancer
- Amplification of epidermal growth factor receptor gene in primary cervical cancer