J Breast Cancer.
2019 Sep;22(3):472-483. 10.4048/jbc.2019.22.e40.
Early Rehabilitation after Total Mastectomy and Immediate Reconstruction with Tissue Expander Insertion in Breast Cancer Patients: A Retrospective Case-control Study
- Affiliations
-
- 1Department of Physical and Rehabilitation Medicine, Samsung Medical Center, Seoul, Korea. hwanglee@skku.edu
- 2Department of Physical and Rehabilitation Medicine, National Rehabilitation Center, Seoul, Korea.
- 3Department of Plastic Surgery, Samsung Medical Center, Seoul, Korea.
- KMID: 2458867
- DOI: http://doi.org/10.4048/jbc.2019.22.e40
Abstract
- PURPOSE
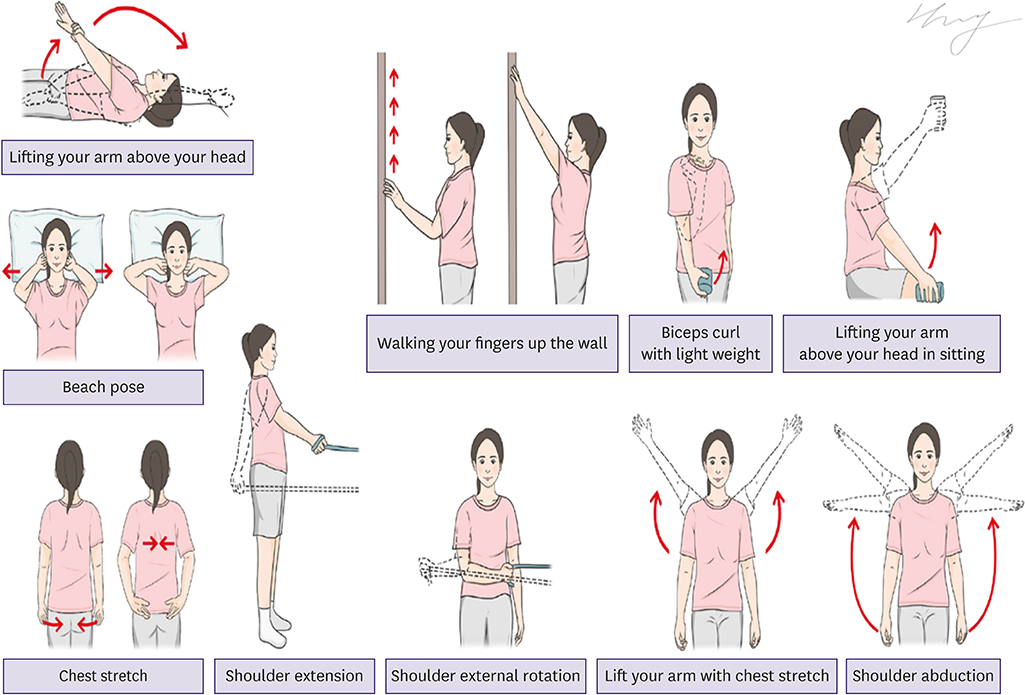
To prevent surgical site complications, many plastic surgeons use the so-called "conventional protocol," which immobilizes the shoulder and upper arm for 1 month after reconstruction. In an effort to improve the shoulder mobility of patients who received immediate breast reconstruction with tissue expander insertion (TEI), we introduced an early rehabilitation protocol with a short-term immobilization period of 2 weeks. This study aims to compare this early rehabilitation exercise program with the conventional protocol and to determine factors affecting shoulder mobility and quality of life of patients after immediate breast reconstruction.
METHODS
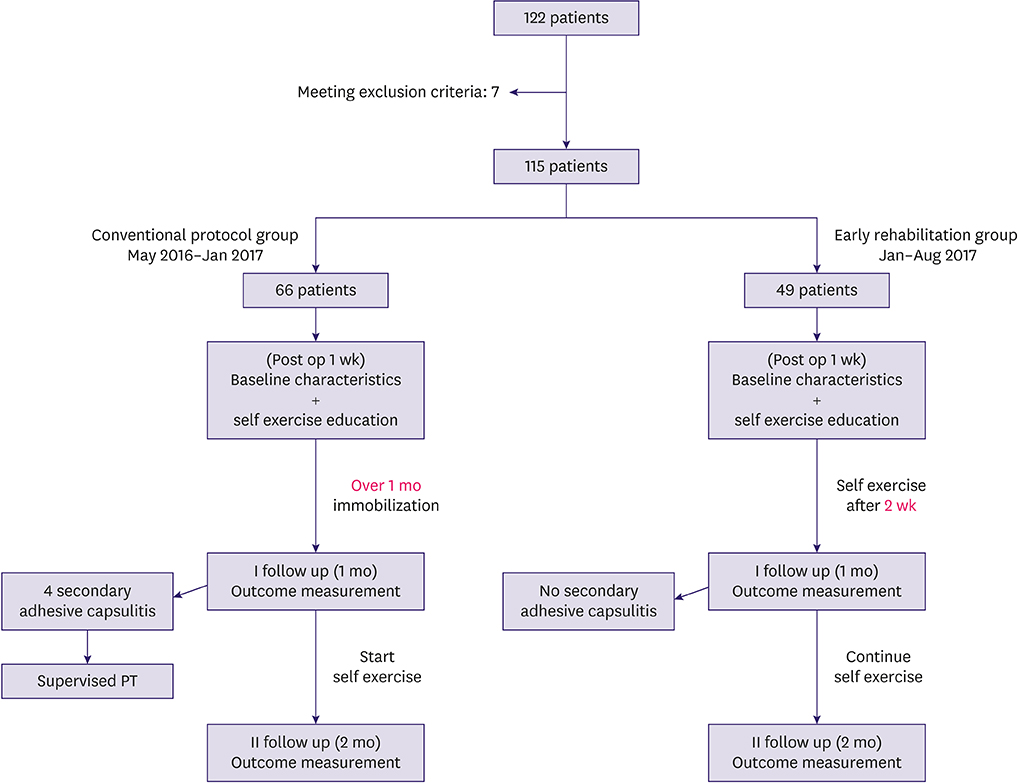
A total of 115 patients with breast cancer who underwent reconstructive surgery were retrospectively reviewed. For patients who underwent reconstruction before January 2017, the conventional protocol was followed with immobilization of their shoulder for over 4 weeks. Patients who underwent reconstruction after January 2017 were educated to undergo a self-exercise program after a short-term immobilization period of 2 weeks. We compared shoulder mobility, pain, quality of life, and complications at postoperative 1 and 2 months between the groups.
RESULTS
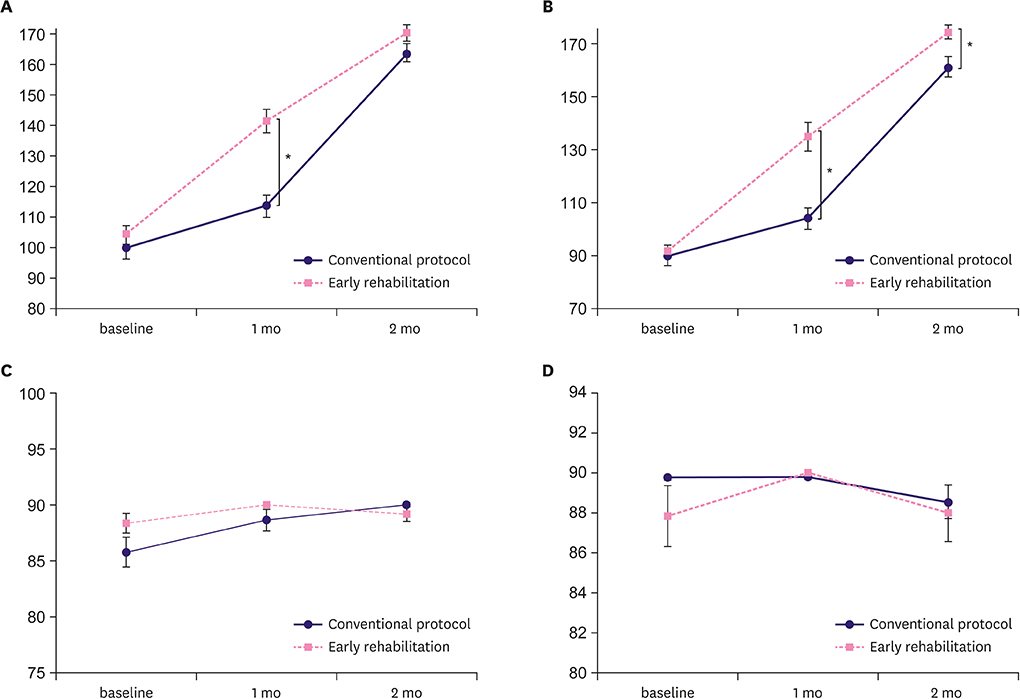
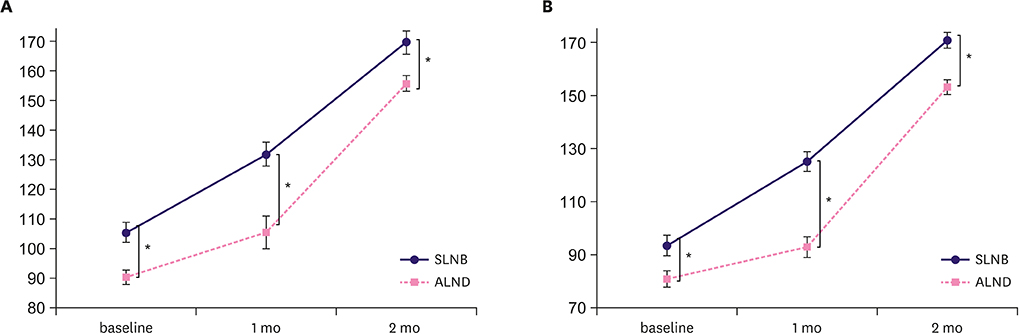
Patients who received early rehabilitation showed greater shoulder flexion and abduction range at postoperative 1 month than those who received the conventional protocol. This increased shoulder abduction range continued until postoperative 2 months. There were no significant surgical site problems in both groups during the 2 months of follow-up.
CONCLUSION
To enhance the recovery of shoulder mobility, early rehabilitation with a shorter immobilization period should be recommended to patients with breast cancer undergoing reconstruction surgery with TEI. TRIAL REGISTRATION: ClinicalTrials.gov Identifier: NCT03541161
Keyword
MeSH Terms
Figure
Reference
-
1. Spear SL, Spittler CJ. Breast reconstruction with implants and expanders. Plast Reconstr Surg. 2001; 107:177–187.
Article2. Argenta LC. Reconstruction of the breast by tissue expansion. Clin Plast Surg. 1984; 11:257–264.
Article3. Scaffidi M, Vulpiani MC, Vetrano M, Conforti F, Marchetti MR, Bonifacino A, et al. Early rehabilitation reduces the onset of complications in the upper limb following breast cancer surgery. Eur J Phys Rehabil Med. 2012; 48:601–611.4. Testa A, Iannace C, Di Libero L. Strengths of early physical rehabilitation programs in surgical breast cancer patients: results of a randomized controlled study. Eur J Phys Rehabil Med. 2014; 50:275–284.5. McNeely ML, Campbell K, Ospina M, Rowe BH, Dabbs K, Klassen TP, et al. Exercise interventions for upper-limb dysfunction due to breast cancer treatment. Cochrane Database Syst Rev. 2010; CD005211.
Article6. Davila AA, Mioton LM, Chow G, Wang E, Merkow RP, Bilimoria KY, et al. Immediate two-stage tissue expander breast reconstruction compared with one-stage permanent implant breast reconstruction: a multi-institutional comparison of short-term complications. J Plast Surg Hand Surg. 2013; 47:344–349.
Article7. Gabriel SE, Woods JE, O'Fallon WM, Beard CM, Kurland LT, Melton LJ 3rd. Complications leading to surgery after breast implantation. N Engl J Med. 1997; 336:677–682.
Article8. Recchia TL, Prim AC, Luz CM. Upper limb functionality and quality of life in women with five-year survival after breast cancer surgery. Rev Bras Ginecol Obstet. 2017; 39:115–122.
Article9. Chan DN, Lui LY, So WK. Effectiveness of exercise programmes on shoulder mobility and lymphoedema after axillary lymph node dissection for breast cancer: systematic review. J Adv Nurs. 2010; 66:1902–1914.
Article10. Petrek JA, Peters MM, Nori S, Knauer C, Kinne DW, Rogatko A. Axillary lymphadenectomy. A prospective, randomized trial of 13 factors influencing drainage, including early or delayed arm mobilization. Arch Surg. 1990; 125:378–382.11. Rodier JF, Gadonneix P, Dauplat J, Issert B, Giraud B. Influence of the timing of physiotherapy upon the lymphatic complications of axillary dissection for breast cancer. Int Surg. 1987; 72:166–169.12. Lee SH, Yoon C, Chung SG, Kim HC, Kwak Y, Park HW, et al. Measurement of shoulder range of motion in patients with adhesive capsulitis using a Kinect. PLoS One. 2015; 10:e0129398.
Article13. Yang S, Park DH, Ahn SH, Kim J, Lee JW, Han JY, et al. Prevalence and risk factors of adhesive capsulitis of the shoulder after breast cancer treatment. Support Care Cancer. 2017; 25:1317–1322.
Article14. Finch E, Brooks D, Stratford PW, Mayo NE. Physical Rehabilitation Outcome Measures. 2nd ed. Toronto: B.C. Decker Inc.;2002.15. Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005; 14:798–804.
Article16. Treanor C, Donnelly M. A methodological review of the Short Form Health Survey 36 (SF-36) and its derivatives among breast cancer survivors. Qual Life Res. 2015; 24:339–362.
Article17. Han CW, Lee EJ, Iwaya T, Kataoka H, Kohzuki M. Development of the Korean version of Short-Form 36-Item Health Survey: health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J Exp Med. 2004; 203:189–194.
Article18. Gupta S, King WD, Korzeniowski M, Wallace DL, Mackillop WJ. The effect of waiting times for postoperative radiotherapy on outcomes for women receiving partial mastectomy for breast cancer: a systematic review and meta-analysis. Clin Oncol (R Coll Radiol). 2016; 28:739–749.
Article19. Blomqvist L, Stark B, Engler N, Malm M. Evaluation of arm and shoulder mobility and strength after modified radical mastectomy and radiotherapy. Acta Oncol. 2004; 43:280–283.
Article20. Krynyckyi BR, Kim CK. Short-term morbidity of the upper limb after sentinel lymph node biopsy or axillary lymph node dissection for stage I or II breast carcinoma. Cancer. 2004; 101:2367–2368.
Article21. Lauridsen MC, Christiansen P, Hessov I. The effect of physiotherapy on shoulder function in patients surgically treated for breast cancer: a randomized study. Acta Oncol. 2005; 44:449–457.
Article22. Helms G, Kühn T, Moser L, Remmel E, Kreienberg R. Shoulder-arm morbidity in patients with sentinel node biopsy and complete axillary dissection--data from a prospective randomised trial. Eur J Surg Oncol. 2009; 35:696–701.
Article23. Leidenius M, Leppänen E, Krogerus L, von Smitten K. Motion restriction and axillary web syndrome after sentinel node biopsy and axillary clearance in breast cancer. Am J Surg. 2003; 185:127–130.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Immediate Tissue Expander Insertion for Breast Reconstruction Following Mastectomy for Breast Cancer Patients. Our Experience of Breast Surgeon - MDbP 101
- A Comparison of Permanent Expander-Implant in Immediate and Delayed Breast Reconstruction after Modified Radical Mastectomy
- Technical approach and clinical outcomes of delayed two-stage tissue expander/implant breast reconstruction: a single-institution experience
- Nipple Reconstruction using the C-V Flap Technique after Breast Reconstruction with the Only Breast Expander
- A Clinical Study of Subcutaneous Mastectomy with Immediate Reconstruction as Treatment for Early Breast Carcinoma